Overview of Follow-Up
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Delayed Multiple Port Sites Metastases After Laparoscopic Radical Prostatectomy
CASE REPORT Delayed Multiple Port Sites Metastases After Laparoscopic Radical Prostatectomy Brusabhanu Nayak, MS, MCH, Prem Nath Dogra, MS, MCH, Vaibhav Saxena, MS, MCH, Ashis Saini, MS, MCH Department of Urology, All India Institute of Medical Sciences, New Delhi, India (all authors). ABSTRACT Introduction: Laparoscopic port site metastases are recurrent nodular lesions developing locally in the abdominal wall within the scar tissue of one or more trocar sites. We are reporting an extremely rare case of delayed multiple port site metastases 3 years after laparoscopic radical prostatectomy. In this case, 3 port site metastases appeared 3 years after laparoscopic radical prostatectomy. Case Description: A 65-year-old man was evaluated for lower urinary tract symptoms and found to have raised serum prostate-specific antigen of 9.06 ng/mL. Transrectal ultrasonography-guided biopsy of the prostate revealed an adeno- carcinoma of the prostate (Gleason score 3 ϩ 4 ϭ 7), with 5 of 12 cores positive for tumor. Contrast-enhanced computed tomography showed localized disease with no involvement of seminal vesicle or lymph nodes. The bone scan was normal. He underwent laparoscopic radical prostatectomy for localized carcinoma of the prostate. He developed 3 port site metastases 3 years after surgery. In view of multiple port site metastatic disease, bilateral orchiectomy was done. The patient is doing well after 1 year of follow-up. Conclusion: We report an occurrence of delayed multiple port site metastases after laparoscopic radical prostatectomy. The 3 sites of metastases in our case included the extraction site, the most active instrument site, and the drain placement site. -

Gender Dysphoria Treatment – Commercial Medical Policy
UnitedHealthcare® Commercial Medical Policy Gender Dysphoria Treatment Policy Number: 2021T0580J Effective Date: April 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ....................................................................... 1 • Blepharoplasty, Blepharoptosis and Brow Ptosis Documentation Requirements ...................................................... 3 Repair Definitions ...................................................................................... 4 • Botulinum Toxins A and B Applicable Codes .......................................................................... 5 • Cosmetic and Reconstructive Procedures Description of Services ................................................................. 9 • Gonadotropin Releasing Hormone Analogs Benefit Considerations .................................................................. 9 Clinical Evidence ......................................................................... 10 • Habilitative Services and Outpatient Rehabilitation U.S. Food and Drug Administration ........................................... 15 Therapy References ................................................................................... 15 • Panniculectomy and Body Contouring Procedures Policy History/Revision Information ........................................... 16 • Rhinoplasty and Other Nasal Surgeries Instructions for Use ..................................................................... 17 Community Plan Policy • Gender Dysphoria -

Gender Dysphoria Treatment – Community Plan Medical Policy
UnitedHealthcare® Community Plan Medical Policy Gender Dysphoria Treatment Policy Number: CS145.I Effective Date: March 1, 2021 Instructions for Use Table of Contents Page Related Community Plan Policies Application ..................................................................................... 1 • Blepharoplasty, Blepharoptosis, and Brow Ptosis Coverage Rationale ....................................................................... 1 Repair Definitions ...................................................................................... 3 • Botulinum Toxins A and B Applicable Codes .......................................................................... 4 • Cosmetic and Reconstructive Procedures Description of Services ................................................................. 8 • Gonadotropin Releasing Hormone Analogs Benefit Considerations .................................................................. 9 Clinical Evidence ........................................................................... 9 • Panniculectomy and Body Contouring Procedures U.S. Food and Drug Administration ........................................... 14 • Rhinoplasty and Other Nasal Surgeries References ................................................................................... 14 • Speech Language Pathology Services Policy History/Revision Information ........................................... 16 Commercial Policy Instructions for Use ..................................................................... 16 • Gender Dysphoria Treatment -

Robotic Surgery for Male Infertility
Robotic Surgery for Male Infertility Annie Darves-Bornoz, MD, Evan Panken, BS, Robert E. Brannigan, MD, Joshua A. Halpern, MD, MS* KEYWORDS Robotic surgical procedures Infertility Male Vasovasostomy Varicocele KEY POINTS Robotic-assisted approaches to male infertility microsurgery have potential practical benefits including reduction of tremor, 3-dimensional visualization, and decreased need for skilled surgical assistance. Several small, retrospective studies have described robotic-assisted vasectomy reversal with com- parable clinical outcomes to the traditional microsurgical approach. Few studies have described application of the robot to varicocelectomy, testicular sperm extrac- tion, and spermatic cord denervation. The use of robotic-assistance for male infertility procedures is evolving, and adoption has been limited. Rigorous studies are needed to evaluate outcomes and cost-effectiveness. INTRODUCTION with intraperitoneal and pelvic surgery. On the other hand, many of the theoretic and practical ad- Up to 15% of couples have infertility, with approx- 1,2 vantages offered by the robotic approach are imately 50% of cases involving a male factor. A highly transferrable to surgery for male infertility: substantial proportion of men with subfertility have surgically treatable and even reversible etiologies, High quality, 3-dimensional visualization is such as a varicocele or vasal obstruction. The essential for any microsurgical procedure. introduction of the operating microscope revolu- Improved surgeon ergonomics are always desir- tionized the field of male infertility, dramatically able, particularly given the surgeon morbidity improving visualization of small, complex associated with microsurgery.3 anatomic structures. The technical precision Filtering of physiologic tremor can improve pre- afforded has improved operative outcomes across cision during technically demanding micro- the board. -
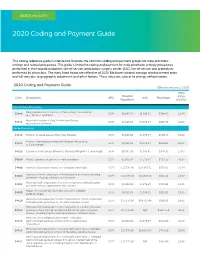
2020 Coding and Payment Guide
MEN’S HEALTH 2020 Coding and Payment Guide This coding reference guide is intended to illustrate the common coding and payment groups for male prosthetic urology and related procedures. This guide is limited to coding and payment for male prosthetic urology procedures performed in the hospital outpatient site-of-service, ambulatory surgery center (ASC) site-of-service and procedures performed by physicians. The rates listed below are reflective of 2020 Medicare national average reimbursement rates and will vary due to geographic adjustment and other factors. These rates are subject to change without notice. 2020 Coding and Payment Guide Effective January 1, 2020 Total Hospital Code Description APC ASC Physicians RVUs Outpatient (Facility) Urinary Sling Procedures Sling operation for correction of male urinary incontinence 53440 5376 $8,067.93 $6.546.11 $784.59 21.74 (e.g., fascia or synthetic) Removal or revision of sling for male incontinence 53442 5375 $4,231.62 $1,976.27 $816.35 22.62 (e.g., fascia or synthetic) Penile Procedures 54110 Excision of penile plaque (Peyronie’s Disease) 5374 $3,018.54 $1,376.97 $650.33 18.02 Excision of penile plaque (Peyronie’s Disease); with graft up 54111 5375 $4,231.62 $1,976.27 $834.03 23.11 to 5 cm in length 54112 Excision of penile plaque (Peyronie’s Disease); with graft > 5 cm in length 5376 $8,067.93 $3,995.65 $976.95 27.07 54360 Plastic operation on penis to correct angulation 5374 $3,018.54 $1,376.97 $751.39 20.82 54400 Insertion of penile prosthesis; non-inflatable (semi-rigid) 5377 $17,573.96 -

Standards for Oncology Registry Entry STORE 2018
STandards for Oncology Registry Entry STORE 2018 Effective for Cases Diagnosed January 1, 2018 STORE STandards for Oncology Registry Entry Released 2018 (Incorporates all updates to Commission on Cancer, National Cancer Database Data standards since FORDS was revised in 2016) Effective for cases diagnosed January 1, 2018 See Appendix A for Updates since FORDS: Revised for 2016. Version 1.0 © 2018 AMERICAN COLLEGE OF SURGEONS All Rights Reserved STORE 2018 Table of Contents Table of Contents Table of Contents ......................................................................................................................... ii Foreword ..................................................................................................................................... 1 FROM “FORDS” TO “STORE” ..................................................................................................................... 1 Preface 2018 ................................................................................................................................ 2 Comorbidities and Complications ............................................................................................................. 2 Revisions to Staging Requirements ........................................................................................................... 2 Staging Data Items No Longer Required for Cases Diagnosed in 2018 and Later (Required for Cases Diagnosed 2017 and Earlier) ................................................................................................................ -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Castration of Male Cats
Castration of Male Cats Ronald M. Bright, DVM, MS, DACVS Purpose of Procedure of the scrotum and the testes) is necessary in some instances of Castration is performed in cats to cancer, trauma, or infection. • Reduce overpopulation and unwanted cats Preparation of Animal • Decrease male aggressiveness, fighting with other tom cats, Your veterinarian will instruct you to withhold food and sometimes and roaming behavior water for a certain period of time, depending on the anesthesia to • Lessen the likelihood of cat bite abscesses from fighting with be used for the surgery. other cats Potential Complications • Decrease the incidence of undesirable urination behaviors Complications following castration are uncommon. • Prevent, eliminate, or remove tumors involving the testes or • Excessive licking may occur, and some type of restraint device, scrotum such as an Elizabethan collar, is required to prevent trauma to • Repair traumatic wounds when surgery may not be able to the incision. preserve the scrotum or testes • A small amount of blood may be noted at the edges of the scrotal • Control certain type of hormonal (endocrine) abnormalities incision. • Some cats that are castrated because of roaming or behavioral Description of Technique problems have no significant improvement after castration. Castration, or orchiectomy , is surgical removal of the testicles. • Similarly, the incidence of cat bite abscesses may not decrease Incisions are made directly over the scrotum. If one or both tes- noticeably. ticles are located in the abdomen (retained testicle or cryptorchid- ism), an abdominal exploratory surgery is necessary. Another site Postoperative/Follow-up Care where one or both testicles may be retained is under the skin near It is advisable to avoid granular, clay, or clumping kitty litter for the last nipple or groin area of the abdomen. -

Surgical and Nonsurgical Procedures in Short-Stay Hospitals: United States, 1979
Surgical and Nonsurgical Procedures in Short-Stay Hospitals: United States, 1979 Statistics are presented on the number and rate of procedures performed for inpatients in non-Federal short-stay hospitals by age and sex. These estimates are based on data abstracted from a national sample of hospital records of discharged patients. This report also presents estimates of average length of stay for single-listed procedures, data on preoperative and postoperative days of care, day of the week of procedures, and discharge status of patients. Data From the National Health Survey Series 13, No. 70 DHHS Publication No. (PHS) 83-1731 U.S. Department of Health and Human Services Public Health Service National Center for Health Statistics Hyattsville, Md. February 1983 COPYRIGHT INFORMATION All material appear!ng In this report is In the public doma!n and may be reproduced 01 copied w!thout permission; cnatlon as to source, however. IS appreciated. SUGGESTEO CITATION National Center for Health Statistics, R. Pokras: Surgical and nonsurgical procedures !n short-stay hospitals, United States, 1979. Vita/ and Hea/fh .Stati.sties. Series 13-No. 70. DHHS Pub. No. (PHS) 83–1 731. Publlc Health Service. Washington. U.S. Government Prmtmg Offlcet February 1983. Library of Congress Cataloging in Publication Oata Pokras, Robert. Surgical and nonsurgical procedures m short-stay hospitals: Un!ted States, 1979. (Data from the national health survey. Ser!es 13: no. 70) (DHHS publication ; no. (PHS) 83–1731) Includes bibliographical references. Supt. of Dots. no.: HE 20.6209:1 3/70 I 1. Operations, Surgical—United States—Stat!stlcs. 2. Hospital utilization—United States—Statistics. -

Solitary Testicular Metastasis from Prostate Cancer: a Rare Case of Isolated Recurrence After Radical Prostatectomy
ANTICANCER RESEARCH 30: 1747-1750 (2010) Solitary Testicular Metastasis from Prostate Cancer: A Rare Case of Isolated Recurrence after Radical Prostatectomy STEFAN JANSSEN1, JOACHIM BERNHARDS2, ARISTOTELIS G. ANASTASIADIS3 and FRANK BRUNS1 1Department of Radiation Oncology, Hannover Medical School, Hannover, Germany; 2Department of Pathology, Robert Koch Krankenhaus Gehrden, Germany; 3Department of Urology, Großburgwedel Hospital, Germany Abstract. Background: The prognosis of prostate cancer spread of prostate cancer to the testis is commonly accepted (PC) is mainly determined by the presence or absence of as a sign of advanced disease and is often accompanied by metastases. An isolated testicular metastasis of PC is rare. multiple metastases to other organs, especially to the skeletal Case Report: A 71-year-old patient with PC presented with system (4). an increased serum prostate-specific antigen (PSA) level of We report the case of a 71-year-old patient who presented 2.07 ng/ml two and a half years after radical prostatectomy. with a solitary testicular metastasis of prostate cancer two Assuming a local recurrence in the prostatic fossa, local and a half years after prostatectomy. The patient remains free radiotherapy with 64.8 Gy was performed. Unfortunately, the of disease two years after unilateral orchiectomy. PSA level rose again, accompanied by a swelling of the left testis approximately one month after radiotherapy. A Case Report unilateral orchiectomy was then performed, presenting a testicular metastasis of the PC. After orchiectomy, the PSA A 71-year-old Caucasian male consulted his family doctor decreased to <0.07 ng/ml. Two years later, the patient is still complaining of haematospermia. -

Department of Urology
07/21/2020 www.ucsfmedicalcenter.org/medstaffoffice/privilege_form.asp?LINK=995 www.ucsfmedicalcenter.org/medstaffoffice/privilege_form.asp?LINK=995 Department of Urology CAT 1 Basic Privileges: Patient management including H & Ps and diagnostic and therapeutic treatments, procedures and interventions encompassing the areas described below and similar activities Requiring a level of training generally associated with persons who have completed the residency program prescribed by the American Board of Urology, and a level of skill and ability generally associated with persons who are diplomates of that board. A) Diagnosis and treatment of diseases and abnormalities of the female urinary tract and the male urogenital tract, including administration of topical and local anesthesia. Includes minor urologic procedures such as dorsal slit, circumcision, biopsymeatotomy, and vasectomy. CAT 2 Subspecialty Privileges: Patient management at this level encompasses the items marked below, and similar activities Requiring a level of training, skill and ability generally associated with persons who are diplomates of the American Board of Urology and who have had additional training and/or experience in specific patient management problems and specialized expertise and training in order to perform the procedures A) Radical procedures such as radical cystectomy, radical prostatectomy, radical penectomy, radical nephrectomy, lymphadenectomy, extenterations, laparoscopic and percutaneous procedures, laser and renovascular surgery. B) Renal transplantation CAT 3 Special Privileges: Patient management at this level encompasses the items marked below, and similar activities Requiring a level of training, skill and ability generally associated with persons who are diplomates of the American Board of Urology and who have had additional training and/or experience in specific patient management problems. -
The Case of Mr. Powers' Prostate Cancer Recurrence
Prostate Cancer 2 - The Case of Mr. Powers’ Prostate Cancer Recurrence Mr. Powers is a young appearing, healthy 73-year old male who underwent a radical prostatectomy nine years ago for prostate cancer. He now has evidence of prostate cancer recurrence. You are expected to direct the evaluation, education, and management of this patient. LEARNING OBJECTIVES 1.Describe the natural history and the common patterns of progression of prostate cancer 2.List the signs & symptoms of metastatic prostate cancer 3.List the options for management of metastatic prostate cancer and describe the mechanisms by which these treatments work Mr. Powers Finally Returns to Clinic Mr. Powers has spent the last several years travelling the world and enjoying himself (“Yea, baby”). He underwent a radical prostatectomy nine years ago for Gleason 6 prostate cancer. While his initial PSA was undetectable his first year, it began to rise slowly after that. He suffered moderate erectile dysfunction after the procedure, but has now recovered fully. Unfortunately, his jet setting lifestyle has filled up his schedule and he was lost to follow-up. Now, Mr. Powers reports no urinary problems and no bone pain. On physical exam, his MoJo is intact and the prostate bed is empty on DRE (as would be expected). His PSA level is checked and comes back 68 ng/ml. Managing Mr. Powers High PSA Mr. Powers cringes upon learning that the traditional therapy for advanced prostate cancer was bilateral orchiectomy. "Not my wedding tackle, Baby," he rants. The rationale for this therapy is that testosterone (and other androgens) actively stimulate the growth of prostate cancer.