Result S of Intraocular Lens Implantation in Paediatric Aphakia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Improved Preservation of Human Corneal Basement Membrane
BritishJournal ofOphthalmology 1994; 78: 863-870 863 Improved preservation ofhuman corneal basement membrane following freezing of donor tissue for Br J Ophthalmol: first published as 10.1136/bjo.78.11.863 on 1 November 1994. Downloaded from epikeratophakia Robert D Young, W John Armitage, Paul Bowerman, Stuart D Cook, David L Easty Abstract States, good results continue to be achieved by Current methods for the production of the small number ofBritish surgeons performing lenticules for epikeratophakia involve rapid the technique.4 However, no comprehensive freezing, cryolathing, and slow warming of the account of its long term outcome has yet been donor cornea. We have found that this pro- published. cedure causes structural damage to the Several complications resulting in the failure epithelial basement membrane in the donor of epikeratophakia have been reported, includ- cornea which may subsequently contribute to ing infection, graft dehiscence, persistent inter- poor postoperative re-epithelialisation of the face haze or opacity, ulceration, and imperfect implant, leading to graft failure. Endeavouring re-epithelialisation. Among these, the failure of to overcome these problems, the effects of host epithelial cells to migrate over and re- cryoprotection of donor cornea were investi- surface the anterior face of the grafted tissue gated, using dimethyl sulphoxide, in conjunc- continues to be the major reason for the removal tion with different cooling and warming rates ofepikeratophakia lenticules.'-'0 as part of the protocol for cryolathing. The Epithelial healing is itselfa complex phenome- structural integrity of the epithelial basement non involving mitosis of host cells at the graft membrane zone (BMZ) was then assessed by periphery, centripetal migration, and attach- electron microscopy and by immunofluores- ment. -

Infantile Aphakia and Successful Fitting of Pediatric Contact Lenses; a Case Presentation Authors: Virji N, Patel A, Libassi D
Infantile aphakia and successful fitting of pediatric contact lenses; a case presentation Authors: Virji N, Patel A, Libassi D An eleven month old male presents with bilateral aphakia secondary to congenital cataracts. The patient is currently successfully wearing B&L Silsoft Pediatric contact lenses, with good prognosis for vision in both eyes. I. Case History -Patient demographics: African American male, DOB 8/18/2009 -Chief complaint: patient presents with bilateral aphakia secondary to bilateral congenital cataract extraction -Ocular, medical history: S/P CE with anterior vitrectomy OD 09/22/2009, followed by OS 09/29/09. (+) squinting, rubs eyes, light sensitivity -Medications: none -Other salient information: patient has been seen by SUNY Contact Lens clinic since 2 months old, 10/14/2009 II. Pertinent findings -Clinical: Keratometry readings 41.00/41.25 @ 005 OD, 38.50/41.00 @ 046 Axial length, immeasurable Horizontal corneal diameter 8mm OD/OS Fundus exam WNL OU -Others: surgical dates: successful CE OU, September 2009 III. Differential diagnosis -Primary/leading: Idiopathic -Others: Posterior lenticonus, persistent hyperplastic primary vitreous, anterior segment dysgenesis, and posterior pole tumors, trauma, intrauterine infection (rubella), maternal hypoglycemia, trisomy (eg, Down, Edward, and Patau syndromes), myotonic dystrophy, infectious diseases (eg, toxoplasmosis, rubella, cytomegalovirus, and herpes simplex [TORCH]), and prematurity. (5) IV. Diagnosis and discussion -Elaborate on the condition: Bilateral infantile cataracts are one of the major treatable causes of visual impairment in children. (2) Hubel and Weisel’s research on the critical period of visual development determined that if infantile cataracts are removed within the critical period and appropriate correction is worn, vision is greatly improved. -

Photorefractive Keratectomy for Correction of Epikeratophakia
CASE REPORTS AND SMALL CASE SERIES high myopia resulting from poste- results might be related to the pre- Photorefractive Keratectomy rior lenticonus. Postsurgical refrac- existing corneal stromal abnormali- for Correction of tion was stable for 8 years, then a ties in their patients, which were not Epikeratophakia Regression rapid myopic regression of the epi- observed in our group. Thus, PRK keratophakic lenses was observed can effectively be used to treat epi- Excimer laser photorefractive kera- the following year (Table). In- keratophakic regressed lenses in a se- tectomy (PRK) is widely used for the stead of removing the failed epikera- lected group of patients in whom correction of myopia, astigmatism, tophakic lenses, we performed PRK both the epikeratograft and the sur- and hyperopia.1,2 It has also been on the eyes. rounding cornea are clear. This used for correction of astigmatism method eliminates the need for re- after penetrating keratoplasty.3 Results. Two and a half years after moval of the epikeratograft and ex- Epikeratophakia has been used PRK, the refraction in all 4 eyes is posing the patient to the risks of suc- in the treatment of nontolerant con- stable and the epigrafts are clear. The cessive penetrating keratoplasty. tact lens keratoconous patients.4,5 Table presents the refraction and vi- The epigrafts were made from ma- sual acuity results for the eyes be- Hirsh Ami, MD chined corneal tissue that was found fore PRK and at 3 months, 1 year, Solberg Yoram, MD, PhD unsuitable for penetrating kerato- and 21⁄2 years after PRK. No haze has Cahana Michael, MD plasty. -
Intraocular Lenses and Spectacle Correction
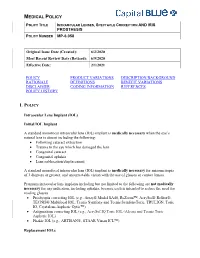
MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER MP-6.058 Original Issue Date (Created): 6/2/2020 Most Recent Review Date (Revised): 6/9/2020 Effective Date: 2/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Intraocular Lens Implant (IOL) Initial IOL Implant A standard monofocal intraocular lens (IOL) implant is medically necessary when the eye’s natural lens is absent including the following: Following cataract extraction Trauma to the eye which has damaged the lens Congenital cataract Congenital aphakia Lens subluxation/displacement A standard monofocal intraocular lens (IOL) implant is medically necessary for anisometropia of 3 diopters or greater, and uncorrectable vision with the use of glasses or contact lenses. Premium intraocular lens implants including but not limited to the following are not medically necessary for any indication, including aphakia, because each is intended to reduce the need for reading glasses. Presbyopia correcting IOL (e.g., Array® Model SA40, ReZoom™, AcrySof® ReStor®, TECNIS® Multifocal IOL, Tecnis Symfony and Tecnis SymfonyToric, TRULIGN, Toric IO, Crystalens Aspheric Optic™) Astigmatism correcting IOL (e.g., AcrySof IQ Toric IOL (Alcon) and Tecnis Toric Aspheric IOL) Phakic IOL (e.g., ARTISAN®, STAAR Visian ICL™) Replacement IOLs MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER -

Solved/Unsolved
Supplementary Materials: Supplementary table 1. Demographic details for the 54 individual patients (solved/unsolved) and their clinical features including cataract type, details of ocular co-morbidities, systemic features and whether cataract was the presenting feature (non-isolated cataract patients only). Abbreviations: yes (Y), no (N), not applicable (N/A). Age at Famil Ag M/ Age at Cataract Cataract Cataract Systemic Consanguinit Patient ID Gene Confirmed genetic diagnosis Ethnicity diagnosi Ocular co-morbidities FH y ID e F surgery type RE type LE presenting sign features y s (days) Aniridia, nystagmus, 23 years Posterior Posterior 1-1 1 PAX6 Aniridia White British 25 F - glaucoma, foveal N N N Y 4 months subcapsular subcapsular hypoplasia Cleft palate, epilepsy, high Aphakia Aphakia Macular atrophy, myopia, 7 years 9 7 years 8 arched palate, 2-1 2 COL11A1 Stickler syndrome, type II Not Stated 34 F (post- (post- lens subluxation, vitreous N N N months months flattened surgical) surgical) anomaly maxilla, short stature (5'2ft) Anterior segment dysgenesis, pupillary abnormalities including 12 years Posterior Posterior ectopic pupils, ectropion 3-1 3 CPAMD8 Anterior segment dysgenesis 8 Other, Any other 27 F - N N Y N 5 months subcapsular subcapsular UVAE and irodensis, nystagmus, dysplastic optic discs, large corneal diameters Gyrate atrophy of choroid and 23 years 29 years 1 Posterior Posterior Retinal dystrophy, Bipolar 4-1 4 OAT White British 42 F N N N retina 7 months month subcapsular subcapsular exotropia disorder 1 year 6 1 year -

Feasibility and Outcome of Descemet Membrane Endothelial Keratoplasty in Complex Anterior Segment and Vitreous Disease
CLINICAL SCIENCE Feasibility and Outcome of Descemet Membrane Endothelial Keratoplasty in Complex Anterior Segment and Vitreous Disease Julia M. Weller, MD, Theofilos Tourtas, MD, and Friedrich E. Kruse, MD escemet membrane endothelial keratoplasty (DMEK), Purpose: Descemet membrane endothelial keratoplasty (DMEK) is Da technique for posterior lamellar keratoplasty, involves becoming the method of choice for treating Fuchs endothelial a graft consisting only of the thin Descemet membrane with dystrophy and pseudophakic bullous keratopathy. We investigated adherent corneal endothelial cells. Introduced in 2006 by whether DMEK can serve as a routine procedure in endothelial Melles et al,1 DMEK is becoming more popular as several decompensation even in complex preoperative situations. studies show its superiority to Descemet stripping automated Methods: Of a total of 1184 DMEK surgeries, 24 consecutive eyes endothelial keratoplasty (DSAEK), regarding visual function 2,3 with endothelial decompensation and complex preoperative situa- and the time of visual rehabilitation after DMEK. However, tions were retrospectively analyzed and divided into 5 groups: group because DMEK grafts are thinner than DSAEK grafts, it is fi 1: irido-corneo-endothelial syndrome (n = 3), group 2: aphakia, more dif cult to handle them and typically takes surgeons subluxated posterior chamber intraocular lens or anterior chamber longer to learn. intraocular lens (n = 6), group 3: DMEK after trabeculectomy (n = In difficult situations, most surgeons prefer DSAEK or 4), group 4: DMEK with simultaneous intravitreal injection (n = 6), penetrating keratoplasty to DMEK because of its possible and group 5: DMEK after vitrectomy (n = 5). Main outcome intraoperative complications. For example, if corneal edema 4 parameters were best-corrected visual acuity, central corneal thick- is advanced, Ham et al recommend performing DSAEK first ness, endothelial cell density, rebubbling rate, and graft failure rate. -

Glaucoma-Related Adverse Events in the Infant Aphakia Treatment Study 1-Year Results
CLINICAL SCIENCES ONLINE FIRST Glaucoma-Related Adverse Events in the Infant Aphakia Treatment Study 1-Year Results Allen D. Beck, MD; Sharon F. Freedman, MD; Michael J. Lynn, MS; Erick Bothun, MD; Daniel E. Neely, MD; Scott R. Lambert, MD; for the Infant Aphakia Treatment Study Group Objectives: To report the incidence of glaucoma and glau- sistent fetal vasculature and 1.6 times higher for each coma suspects in the IATS, and to evaluate risk factors for month of age younger at cataract surgery. the development of a glaucoma-related adverse event in patients in the IATS in the first year of follow-up. Conclusions: Modern surgical techniques do not elimi- nate the early development of glaucoma following con- Methods: A total of 114 infants between 1 and 6 months genital cataract surgery with or without an intraocular of age with a unilateral congenital cataract were as- lens implant. Younger patients with or without persis- signed to undergo cataract surgery either with or with- tent fetal vasculature seem more likely to develop a glau- out an intraocular lens implant. Standardized defini- coma-related adverse event in the first year of follow- tions of glaucoma and glaucoma suspect were created and up. Vigilance for the early development of glaucoma is used in the IATS. needed following congenital cataract surgery, especially when surgery is performed during early infancy or for a Results: Of these 114 patients, 10 (9%) developed glau- child with persistent fetal vasculature. Five-year fol- coma and 4 (4%) had glaucoma suspect, for a total of 14 low-up data for the IATS will likely reveal more glaucoma- patients (12%) with a glaucoma-related adverse event in related adverse events. -

Visual Management of Aphakia with Concomitant Severe Corneal Irregularity by Mini-Scleral Design Contact Lenses
HOSTED BY Available online at www.sciencedirect.com ScienceDirect Journal of Current Ophthalmology 28 (2016) 27e31 http://www.journals.elsevier.com/journal-of-current-ophthalmology Original research Visual management of aphakia with concomitant severe corneal irregularity by mini-scleral design contact lenses Fateme Alipur, Seyedeh Simindokht Hosseini* Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran Received 30 October 2015; accepted 28 January 2016 Available online 30 March 2016 Abstract Purpose: To evaluate visual results, comfort of use, safety, and efficacy of mini scleral contact lenses in optical management in patients with traumatic aphakia and severe concomitant irido-corneal injury. Methods: In a case series, eight eyes with post traumatic aphakia and severe concomitant irido-corneal injury that were evaluated at the Contact Lens Clinic of Farabi Eye Hospital, Tehran, Iran for contact lens fitting and could not be corrected with conventional corneal RGP contact lenses were fitted with miniscleral contact lenses. Uncorrected visual acuity (UCVA), best spectacle corrected visual acuity (BSCVA), and BCVA (Best corrected visual acuity) with miniscleral lens were recorded. Slit lamp examination, comfortable daily wearing time, and any contact lens-related complication were documented in each follow-up visit. Results: The mean UCVA and BSCVA of the cases was >2.7 and 0.41 LogMAR, respectively (BSCVA could not be assessed in one case due to severe corneal irregularity). The mean final BCVA with the miniscleral lens was 0.05 LogMAR (range from 0.4 to À0.04 LogMAR). The mean follow-up period was 14.6 months. The mean comfortable daily wearing time (CDWT) was 11.6 h, ranging from 8 to 16 h. -

Eleventh Edition
SUPPLEMENT TO April 15, 2009 A JOBSON PUBLICATION www.revoptom.com Eleventh Edition Joseph W. Sowka, O.D., FAAO, Dipl. Andrew S. Gurwood, O.D., FAAO, Dipl. Alan G. Kabat, O.D., FAAO Supported by an unrestricted grant from Alcon, Inc. 001_ro0409_handbook 4/2/09 9:42 AM Page 4 TABLE OF CONTENTS Eyelids & Adnexa Conjunctiva & Sclera Cornea Uvea & Glaucoma Viitreous & Retiina Neuro-Ophthalmic Disease Oculosystemic Disease EYELIDS & ADNEXA VITREOUS & RETINA Blow-Out Fracture................................................ 6 Asteroid Hyalosis ................................................33 Acquired Ptosis ................................................... 7 Retinal Arterial Macroaneurysm............................34 Acquired Entropion ............................................. 9 Retinal Emboli.....................................................36 Verruca & Papilloma............................................11 Hypertensive Retinopathy.....................................37 Idiopathic Juxtafoveal Retinal Telangiectasia...........39 CONJUNCTIVA & SCLERA Ocular Ischemic Syndrome...................................40 Scleral Melt ........................................................13 Retinal Artery Occlusion ......................................42 Giant Papillary Conjunctivitis................................14 Conjunctival Lymphoma .......................................15 NEURO-OPHTHALMIC DISEASE Blue Sclera .........................................................17 Dorsal Midbrain Syndrome ..................................45 -

Ocular Colobomaâ
Eye (2021) 35:2086–2109 https://doi.org/10.1038/s41433-021-01501-5 REVIEW ARTICLE Ocular coloboma—a comprehensive review for the clinician 1,2,3 4 5 5 6 1,2,3,7 Gopal Lingam ● Alok C. Sen ● Vijaya Lingam ● Muna Bhende ● Tapas Ranjan Padhi ● Su Xinyi Received: 7 November 2020 / Revised: 9 February 2021 / Accepted: 1 March 2021 / Published online: 21 March 2021 © The Author(s) 2021. This article is published with open access Abstract Typical ocular coloboma is caused by defective closure of the embryonal fissure. The occurrence of coloboma can be sporadic, hereditary (known or unknown gene defects) or associated with chromosomal abnormalities. Ocular colobomata are more often associated with systemic abnormalities when caused by chromosomal abnormalities. The ocular manifestations vary widely. At one extreme, the eye is hardly recognisable and non-functional—having been compressed by an orbital cyst, while at the other, one finds minimalistic involvement that hardly affects the structure and function of the eye. In the fundus, the variability involves the size of the coloboma (anteroposterior and transverse extent) and the involvement of the optic disc and fovea. The visual acuity is affected when coloboma involves disc and fovea, or is complicated by occurrence of retinal detachment, choroidal neovascular membrane, cataract, amblyopia due to uncorrected refractive errors, etc. While the basic birth anomaly cannot be corrected, most of the complications listed above are correctable to a great 1234567890();,: 1234567890();,: extent. Current day surgical management of coloboma-related retinal detachments has evolved to yield consistently good results. Cataract surgery in these eyes can pose a challenge due to a combination of microphthalmos and relatively hard lenses, resulting in increased risk of intra-operative complications. -

Clinical Manifestations of Congenital Aniridia
Clinical Manifestations of Congenital Aniridia Bhupesh Singh, MD; Ashik Mohamed, MBBS, M Tech; Sunita Chaurasia, MD; Muralidhar Ramappa, MD; Anil Kumar Mandal, MD; Subhadra Jalali, MD; Virender S. Sangwan, MD ABSTRACT Purpose: To study the various clinical manifestations as- were subluxation, coloboma, posterior lenticonus, and sociated with congenital aniridia in an Indian population. microspherophakia. Corneal involvement of varying degrees was seen in 157 of 262 (59.9%) eyes, glaucoma Methods: In this retrospective, consecutive, observa- was identified in 95 of 262 (36.3%) eyes, and foveal hy- tional case series, all patients with the diagnosis of con- poplasia could be assessed in 230 of 262 (87.7%) eyes. genital aniridia seen at the institute from January 2005 Median age when glaucoma and cataract were noted to December 2010 were reviewed. In all patients, the was 7 and 14 years, respectively. None of the patients demographic profile, visual acuity, and associated sys- had Wilm’s tumor. temic and ocular manifestations were studied. Conclusions: Congenital aniridia was commonly as- Results: The study included 262 eyes of 131 patients sociated with classically described ocular features. with congenital aniridia. Median patient age at the time However, systemic associations were characteristically of initial visit was 8 years (range: 1 day to 73 years). Most absent in this population. Notably, cataract and glau- cases were sporadic and none of the patients had par- coma were seen at an early age. This warrants a careful ents afflicted with aniridia. The most common anterior evaluation and periodic follow-up in these patients for segment abnormality identified was lenticular changes. -

Retropupillary Iris-Claw Intraocular Lens in Ectopia Lentis Due To
ndrom Sy es tic & e G n e e n G e f T o Forlini et al., J Genet Syndr Gene Ther 2013, 4:8 Journal of Genetic Syndromes h l e a r n a r p DOI: 10.4172/2157-7412.1000170 u y o J & Gene Therapy ISSN: 2157-7412 Case Report Open Access Retropupillary Iris-Claw Intraocular Lens in Ectopia Lentis Due to Marfan Syndrome Matteo Forlini1, Ana Laura Gramajo2, Robert Rejdak3, Agata Prokopiuk3, Oxana Levkina4, Adriana IonelaBratu5, Paolo Rossini5, Perfecto R Cagampang6, Gian Maria Cavallini1 and Cesare Forlini5* 1Institute of Ophthalmology, University of Modena, Modena, Italy 2Centro Privado de Ojos Romagosa – Fundación VER, Córdoba, Argentina 3Department of Ophthalmology, Medical University of Lublin, Lublin, Poland 4European Medical Center, Moscow, Russia 5Department of Ophthalmology, “Santa Maria Delle Croci” Hospital, Ravenna, Italy 6Eye Referral Center, TM Kalaw, Ermita, Manila, Philippines Abstract Background: Surgical treatment of ectopia lentis in Marfan syndrome cases represents a great challenge for ophthalmic surgeons due to zonular weakness, capsular instability and postoperative aphakia correction. We report three cases of surgical treatment of ectopia lentis due to Marfan syndrome and our approach to aphakia correction by implantation of the retroiridally fixated iris-claw intraocular lens. Methods: Prospective interventional case series. All patients underwent extraction of the subluxated lens with or without combined vitrectomy. Aphakia correction was performed using the Iris-claw intraocular lens, positioned retroiridally by traditional enclavation of both haptics into iris midperiphery. Patients were followed-up for 6 months. Intraocular lens power was calculated using the SRK-T formula. Diagnosis of Marfan syndrome was confirmed in all cases by molecular diagnosis.