2014 Slide Library Case Summary Questions & Answers With
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rare Skin Cancers in General Practice
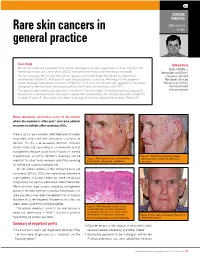
CLINICAL PRACTICE Skin cancer Rare skin cancers in series general practice Case study Anthony Dixon Mr LA has long been troubled with actinic damage to his skin, especially his face. He has had MBBS, FACRRM, is many squamous cell carcinomas (SCCs) removed and many solar keratoses managed. dermasurgeon and Director On this occasion Mr LA had two actinic lesions on his left cheek that failed to respond to of Research, Skin Alert cryotherapy (Figure 1). A biopsy of each site produced a surprise. Histology of the superior Skin Cancer Clinics and lesion revealed sebaceous carcinoma (Figure 2). This is an uncommon yet aggressive cutaneous Skincanceronly, Belmont, malignancy derived from sebaceous glands. The 5 year survival rate is 60–70%. Victoria. anthony@ The tumour was widely excised with a minimum 10 mm margin. A multidisciplinary approach skincanceronly.com resulted in a decision not to proceed to adjunctive radiotherapy. The wound was well healed by 8 weeks (Figure 3). Four years on there is no sign of local or regional recurrence (Figure 4). Many sebaceous carcinomas occur on the eyelids where the outcome is often poor;1 and some patients are prone to multiple other cutaneous SCCs. There is also a rare syndrome called Muir-torre of visceral neoplasms associated with sebaceous carcinoma on the skin.2 As this is an autosomal dominant condition, family history and counselling is an esssential part of management (enquire about family history of internal malignancies). A family member's diagnosis can be Figure 3. Satisfactory healing 8 weeks Figure 1. Two actinic lesions on the left face following wide excision of sebaceous important for other family members and offers screening have failed to respond to cryotherapy carcinoma for internal and cutaneous malignancies. -

Immunohistochemical Analysis of S100-Positive Epidermal
An Bras Dermatol. 2020;95(5):627---630 Anais Brasileiros de Dermatologia www.anaisdedermatologia.org.br DERMATOPATHOLOGY Immunohistochemical analysis of S100-positive ଝ,ଝଝ epidermal Langerhans cells in dermatofibroma Mahmoud Rezk Abdelwhaed Hussein Department of Pathology, Assuit University Hospital, Assuit, Egypt Received 3 February 2020; accepted 12 April 2020 Available online 12 July 2020 Abstract Dermatofibroma is a dermal fibrohistiocytic neoplasm. The Langerhans cells are the KEYWORDS immunocompetent cells of the epidermis, and they represent the first defense barrier of the Histiocytoma, benign immune system towards the environment. The objective was to immunohistologically compare fibrous; the densities of S100-positive Langerhans cells in the healthy peritumoral epidermis against Skin neoplasms; those in the epidermis overlying dermatofibroma (20 cases), using antibodies against the S100 S100 Proteins molecule (the immunophenotypic hallmark of Langerhans cells). The control group (normal, healthy skin) included ten healthy age and sex-matched individuals who underwent skin biopsies for benign skin lesions. A significantly high density of Langerhans cells was observed both in the epidermis of the healthy skin (6.00 ± 0.29) and the peritumoral epidermis (6.44 ± 0.41) vs. those in the epidermis overlying the tumor (1.44 ± 0.33, p < 0.05). The quantitative deficit of Langerhans cells in the epidermis overlying dermatofibroma may be a possible factor in its development. © 2020 Sociedade Brasileira de Dermatologia. Published by Elsevier Espana,˜ S.L.U. This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/4.0/). Langerhans cells (LCs) are the exclusive antigen-presenting tions stained with hematoxylin and eosin as ‘‘clear cells’’ cells of the normal human epidermis. -

Atypical Compound Nevus Arising in Mature Cystic Ovarian Teratoma
J Cutan Pathol 2005: 32: 71–123 Copyright # Blackwell Munksgaard 2005 Blackwell Munksgaard. Printed in Denmark Journal of Cutaneous Pathology Abstracts of the Papers Presented at the 41st Annual Meeting of The American Society of Dermatopathology Westin Copley Place Boston, Massachusetts, USA October 14–17, 2004 These abstracts were presented in oral or poster format at the 41st Annual Meeting of The American Society of Dermatopathology on October 14–17, 2004. They are listed on the following pages in alphabetical order by the first author’s last name. 71 Abstracts IN SITU HYBRIDIZATION IS A VALUABLE DIAGNOSTIC A 37-year-old woman with diagnosis of Sjogren’s syndrome (SS) TOOL IN CUTANEOUS DEEP FUNGAL INFECTIONS presented with asymptomatic non-palpable purpura of the lower J.J. Abbott1, K.L. Hamacher2,A.G.Bridges2 and I. Ahmed1,2 extremities. Biopsy of a purpuric macule revealed a perivascular Departments of Laboratory Medicine and Pathology1 and and focally nodular lymphocytic infiltrate with large numbers of Dermatology2, plasma cells, seemingly around eccrine glands. There was no vascu- litis. The histologic findings in the skin were strikingly similar to those Mayo Clinic and Mayo Foundation, Rochester, MN, USA of salivary, parotid, and other ‘‘secretory’’ glands affected in SS. The cutaneous manifestations of SS highlighted in textbooks include Dimorphic fungal infections (histoplasmosis, blastomycosis, coccidiomy- xerosis, annular erythema, small-vessel vasculitis, and pigmented cosis, and cryptococcosis) can occur in immunocompromised and purpura. This case illustrates that purpura in skin of patients with healthy individuals. Cutaneous involvement is often secondary and SS may be caused by a peri-eccrine plasma-rich infiltrate. -

Storiform Collagenoma: Case Report Colagenoma Estoriforme: Relato De Caso
CASE REPORT Storiform collagenoma: case report Colagenoma estoriforme: relato de caso Guilherme Flosi Stocchero1 ABSTRACT INTRODUCTION Storiform collagenoma is a rare tumor, which originates from the Storiform collagenoma or sclerotic fibroma is a rare proliferation of fibroblasts that show increased production of type-I benign skin tumor that usually affects young adults collagen. It is usually found in the face, neck and extremities, but and middle-age individuals of both sexes. This tumor is it can also appear in the trunk, scalp and, less frequently, in the slightly predominant in women. Storiform collagenoma oral mucosa and the nail bed. It affects both sexes, with a slight female predominance. It may be solitary or multiple, the latter being appears as a small papule or solid fibrous nodule. an important marker for Cowden syndrome. It presents as a painless, It is well-circumscribed, pink, whitish or skin color, solid nodular tumor that is slow-growing. It must be considered in the painless and of slow-growing. This tumor is often differential diagnosis of other well-circumscribed skin lesions, such as found in face and limbs, but it can also appears in dermatofibroma, pleomorphic fibroma, sclerotic lipoma, fibrolipoma, the chest, scalp and, rarely, in oral mucosa and nail giant cell collagenoma, benign fibrous histiocytoma, intradermal Spitz bed. Storiform collagenoma often appears as single nevus and giant cell angiohistiocytoma. tumor, and the occurrence of multiple tumors is an important indication of Cowden syndrome, which is Keywords: Collagen; Hamartoma; Skin neoplasms; Fibroma; Skin; Case a heritage genodermatosis of autosomal dominant reports condition.(1-4) Storiform collagenoma has as differential diagnosis other well-circumscribed skin tumors such RESUMO as dermatofibroma, pleomorphic fibroma, sclerotic O colagenoma estoriforme é um tumor raro originado a partir da lipoma, fibrolipoma, giant cell collagenoma, benign proliferação de fibroblastos com produção aumentada de colágeno tipo I. -

Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

A Case of Discoid Lupus Erythematosus Masquerading As Acne
Letters to the Editor 175 A Case of Discoid Lupus Erythematosus Masquerading as Acne Anastasios Stavrakoglou, Jenny Hughes and Ian Coutts Department of Dermatology, Hillingdon Hospital, Pield Heath Road, Uxbridge UB8 3NN, UK. E-mail: [email protected] Accepted July 4, 2007. Sir, On examination he had a widespread acneiform eruption, We describe here a case of discoid lupus erythemato- which was distributed on his face, pre-sternal area and back, particularly down the length of his spine. He had multiple sus (DLE) masquerading as acne vulgaris. Cutaneous brown-red follicular papules and open comedones, especially manifestations of lupus erythematosus (LE) are usually on his back, and hypopigmented atrophic scars. There were no characteristic enough to permit straightforward diagnosis. pustules or nodulocystic lesions (Fig. 1). However, occasionally they may be variable and mimic Treatment was started with erythromycin 500 mg bid and other dermatological conditions. adapalene cream once daily to treat a presumed diagnosis of acne vulgaris. He was seen 3 months later with a deterioration Acneiform presentation is one of the most rarely re- of his clinical appearance and increased pruritus. This was ported and one of the most confusing, as it resembles a attributed by the patient to increased sun exposure. The photo- very common inflammatory skin disease and therefore aggravation, the intense pruritus and the absence of pustules can be easily missed clinically. Only 5 cases have been and nodulocystic lesions broadened our differential diagnosis reported in the literature (1–4). The patient described and therefore diagnostic biopsies were obtained. A biopsy from the back where the rash was most suggestive clinically here presented with a widespread pruritic acneiform of acne vulgaris, showed hyperkeratosis with orthokeratosis, rash, which was initially diagnosed and treated as epidermal atrophy and extensive vacuolar degeneration of the acne vulgaris with no response. -

Acute Pancreatitis, Non-Alcoholic Fatty Pancreas Disease, and Pancreatic Cancer
JOP. J Pancreas (Online) 2017 Sep 29; 18(5):365-368. REVIEW ARTICLE The Burden of Systemic Adiposity on Pancreatic Disease: Acute Pancreatitis, Non-Alcoholic Fatty Pancreas Disease, and Pancreatic Cancer Ahmad Malli, Feng Li, Darwin L Conwell, Zobeida Cruz-Monserrate, Hisham Hussan, Somashekar G Krishna Division of Gastroenterology, Hepatology and Nutrition, The Ohio State University Wexner Medical Center, Columbus, Ohio, USA ABSTRACT Obesity is a global epidemic as recognized by the World Health Organization. Obesity and its related comorbid conditions were recognized to have an important role in a multitude of acute, chronic, and critical illnesses including acute pancreatitis, nonalcoholic fatty pancreas disease, and pancreatic cancer. This review summarizes the impact of adiposity on a spectrum of pancreatic diseases. INTRODUCTION and even higher mortality in the setting of AP based on multiple reports [8, 9, 10, 11, 12]. Despite the rising incidence Obesity is a global epidemic as recognized by the World of AP over the past two decades, there has been a decrease Health Organization [1]. One third of the world’s population in its overall mortality rate without any obvious decrement is either overweight or obese, and it has doubled over the in the mortality rate among patients with concomitant AP past two decades with an alarming 70% increase in the and morbid obesity [12, 13]. Several prediction models and prevalence of morbid obesity from year 2000 to 2010 [2, risk scores were proposed to anticipate the severity and 3, 4]. Obesity and its related comorbid conditions were prognosis of patient with AP; however, their clinical utility recognized to have an important role in a multitude of is variable, not completely understood, and didn’t take acute, chronic, and critical pancreatic illnesses including obesity as a major contributor into consideration despite the acute pancreatitis, non-alcoholic fatty pancreas disease, aforementioned association [14]. -

The Role of Cytogenetics and Molecular Diagnostics in the Diagnosis of Soft-Tissue Tumors Julia a Bridge
Modern Pathology (2014) 27, S80–S97 S80 & 2014 USCAP, Inc All rights reserved 0893-3952/14 $32.00 The role of cytogenetics and molecular diagnostics in the diagnosis of soft-tissue tumors Julia A Bridge Department of Pathology and Microbiology, University of Nebraska Medical Center, Omaha, NE, USA Soft-tissue sarcomas are rare, comprising o1% of all cancer diagnoses. Yet the diversity of histological subtypes is impressive with 4100 benign and malignant soft-tissue tumor entities defined. Not infrequently, these neoplasms exhibit overlapping clinicopathologic features posing significant challenges in rendering a definitive diagnosis and optimal therapy. Advances in cytogenetic and molecular science have led to the discovery of genetic events in soft- tissue tumors that have not only enriched our understanding of the underlying biology of these neoplasms but have also proven to be powerful diagnostic adjuncts and/or indicators of molecular targeted therapy. In particular, many soft-tissue tumors are characterized by recurrent chromosomal rearrangements that produce specific gene fusions. For pathologists, identification of these fusions as well as other characteristic mutational alterations aids in precise subclassification. This review will address known recurrent or tumor-specific genetic events in soft-tissue tumors and discuss the molecular approaches commonly used in clinical practice to identify them. Emphasis is placed on the role of molecular pathology in the management of soft-tissue tumors. Familiarity with these genetic events -

Case Reports Article – Rapidly Growing Mass in the Ear Canal: A
Arepen et al. (2020): Rapidly growing mass in the ear canal May 2020 Vol. 23 Issue 8 Case reports article – Rapidly growing mass in the ear canal: A rare case of isolated superficial angiomyxoma Siti Asmat Md Arepen1,2, Nor Eyzawiah Hassan1,2, Azlina Abd Rani1, Shahrul Hitam2 Mohd Khairi Md Daud3 1Faculty of Medicine & Health Sciences,Universiti Sains Islam Malaysia, Selangor, Malaysia. 2Department of Otorhinolaryngology Head & Neck Surgery, Hospital Ampang, Selangor, Malaysia. 3Department of Otorhinolaryngology Head & Neck Surgery, Faculty of Medicine & Health Sciences, Universiti Sains Malaysia, Kelantan, Malaysia. Corresponding author: Nor Eyzawiah Hassan ([email protected]) Abstract: Superficial angiomyxoma is a rare benign skin tumour and usually present as an asymptomatic lesion. It is known to be highly recurrent and complete wide excision is the best treatment. This cace reported of 56 yr old gentleman presented with fleshy, pink coloured right external auditory mass. The mass arisen from the posterior wall of the canal at the bony–cartilaginous junction. Clinical diagnosis of an anaural polyp was made and the mass was excised. However, it rapidly recurred bigger than its actual size within a week. The histopathological examination was reported as superficial angiomyxoma. A differential diagnosis of isolated superficial angiomyxoma should be considered in the case of external auditory canal mass and Carney complex needs to be considered. Complete excision and regular follow up is recommended. Keywords: Benign tumour, external auditory canal, myxoma How to cite this article: How to cite this article: Arepen et al. (2020): Case reports article – Rapidly growing mass in the ear canal: A rare case of isolated superficial angiomyxoma, Ann Trop & Public Health, 23 (S8): 1279–1282. -

8.5 X12.5 Doublelines.P65
Cambridge University Press 978-0-521-87409-0 - Modern Soft Tissue Pathology: Tumors and Non-Neoplastic Conditions Edited by Markku Miettinen Index More information Index abdominal ependymoma, 744 mucinous cystadenocarcinoma, 631 adult fibrosarcoma (AF), 364–365, 1026 abdominal extrauterine smooth muscle ovarian adenocarcinoma, 72, 79 adult granulosa cell tumor, 523–524 tumors, 79 pancreatic adenocarcinoma, 846 clinical features, 523 abdominal inflammatory myofibroblastic pulmonary adenocarcinoma, 51 genetics, 524 tumors, 297–298 renal adenocarcinoma, 67 pathology, 523–524 abdominal leiomyoma, 467, 477 serous cystadenocarcinoma, 631 adult rhabdomyoma, 548–549 abdominal leiomyosarcoma. See urinary bladder/urogenital tract clinical features, 548 gastrointestinal stromal tumor adenocarcinoma, 72, 401 differential diagnosis, 549 (GIST) uterine adenocarcinomas, 72 genetics, 549 abdominal perivascular epithelioid cell tumors adenofibroma, 523 pathology, 548–549 (PEComas), 542 adenoid cystic carcinoma, 1035 aggressive angiomyxoma (AAM), 514–518 abdominal wall desmoids, 244 adenomatoid tumor, 811–813 clinical features, 514–516 acquired elastotic hemangioma, 598 adenomatous polyposis coli (APC) gene, 143 differential diagnosis, 518 acquired tufted angioma, 590 adenosarcoma (mullerian¨ adenosarcoma), 523 genetics, 518 acral arteriovenous tumor, 583 adipocytic lesions (cytology), 1017–1022 pathology, 516 acral myxoinflammatory fibroblastic sarcoma atypical lipomatous tumor/well- aggressive digital papillary adenocarcinoma, (AMIFS), 365–370, 1026 differentiated -

Dermatopathology
Dermatopathology Clay Cockerell • Martin C. Mihm Jr. • Brian J. Hall Cary Chisholm • Chad Jessup • Margaret Merola With contributions from: Jerad M. Gardner • Talley Whang Dermatopathology Clinicopathological Correlations Clay Cockerell Cary Chisholm Department of Dermatology Department of Pathology and Dermatopathology University of Texas Southwestern Medical Center Central Texas Pathology Laboratory Dallas , TX Waco , TX USA USA Martin C. Mihm Jr. Chad Jessup Department of Dermatology Department of Dermatology Brigham and Women’s Hospital Tufts Medical Center Boston , MA Boston , MA USA USA Brian J. Hall Margaret Merola Department of Dermatology Department of Pathology University of Texas Southwestern Medical Center Brigham and Women’s Hospital Dallas , TX Boston , MA USA USA With contributions from: Jerad M. Gardner Talley Whang Department of Pathology and Dermatology Harvard Vanguard Medical Associates University of Arkansas for Medical Sciences Boston, MA Little Rock, AR USA USA ISBN 978-1-4471-5447-1 ISBN 978-1-4471-5448-8 (eBook) DOI 10.1007/978-1-4471-5448-8 Springer London Heidelberg New York Dordrecht Library of Congress Control Number: 2013956345 © Springer-Verlag London 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. -

Biomaterials and the Foreign Body Reaction: Surface Chemistry Dependent Macrophage Adhesion, Fusion, Apoptosis, and Cytokine Production
BIOMATERIALS AND THE FOREIGN BODY REACTION: SURFACE CHEMISTRY DEPENDENT MACROPHAGE ADHESION, FUSION, APOPTOSIS, AND CYTOKINE PRODUCTION by JACQUELINE ANN JONES Submitted in partial fulfillment of the requirements For the degree of Doctor of Philosophy Dissertation Advisor: James Morley Anderson, M.D., Ph.D. Department of Biomedical Engineering CASE WESTERN RESERVE UNIVERSITY May, 2007 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the dissertation of ______________________________________________________ candidate for the Ph.D. degree *. (signed)_______________________________________________ (chair of the committee) ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ (date) _______________________ *We also certify that written approval has been obtained for any proprietary material contained therein. Copyright © 2007 by Jacqueline Ann Jones All rights reserved iii Dedication This work is dedicated to… My ever loving and ever supportive parents: My mother, Iris Quiñones Jones, who gave me the freedom to be and to dream, inspires me with her passion and courage, and taught me the true meaning of friendship. My father, Glen Michael Jones, a natural-born teacher who taught me to be an inquisitive student of life, inspires me with his strength and perseverance, and gave me his kind, earnest heart that loves deeply and always