2012 SCIENTIFIC MEETINGS Program Book
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Wonder Woman Matters
Why Wonder Woman Matters When I was a kid, being a hero seemed like the easiest thing in the world to be- A Blue Beetle quote from the DC Comics publication The OMAC Project. Introduction The superhero is one of modern American culture’s most popular and pervasive myths. Though the primary medium, the comic book, is often derided as juvenile or material fit for illiterates the superhero narrative maintains a persistent presence in popular culture through films, television, posters and other mediums. There is a great power in the myth of the superhero. The question “Why does Wonder Woman matter?” could be answered simply. Wonder Woman matters because she is a member of this pantheon of modern American gods. Wonder Woman, along with her cohorts Batman and Superman represent societal ideals and provide colorful reminders of how powerful these ideals can be.1 This answer is compelling, but it ignores Wonder Woman’s often turbulent publication history. In contrast with titles starring Batman or Superman, Wonder Woman comic books have often sold poorly. Further, Wonder Woman does not have quite the presence that Batman and Superman both share in popular culture.2 Any other character under similar circumstances—poor sales, lack of direction and near constant revisions—would have been killed off or quietly faded into the background. Yet, Wonder Woman continues to persist as an important figure both within her comic universe and in our popular consciousness. “Why does Wonder Woman matter?” To answer this question an understanding of the superhero and their primary medium, the comic book, is required, Wonder Woman is a comic book character, and her existence in the popular consciousness largely depends on how she is presented within the conventions of the comic book superhero narrative. -

Mason 2015 02Thesis.Pdf (1.969Mb)
‘Page 1, Panel 1…” Creating an Australian Comic Book Series Author Mason, Paul James Published 2015 Thesis Type Thesis (Professional Doctorate) School Queensland College of Art DOI https://doi.org/10.25904/1912/3741 Copyright Statement The author owns the copyright in this thesis, unless stated otherwise. Downloaded from http://hdl.handle.net/10072/367413 Griffith Research Online https://research-repository.griffith.edu.au ‘Page 1, Panel 1…” Creating an Australian Comic Book Series Paul James Mason s2585694 Bachelor of Arts/Fine Art Major Bachelor of Animation with First Class Honours Queensland College of Art Arts, Education and Law Group Griffith University Submitted in fulfillment for the requirements of the degree of Doctor of Visual Arts (DVA) June 2014 Abstract: What methods do writers and illustrators use to visually approach the comic book page in an American Superhero form that can be adapted to create a professional and engaging Australian hero comic? The purpose of this research is to adapt the approaches used by prominent and influential writers and artists in the American superhero/action comic-book field to create an engaging Australian hero comic book. Further, the aim of this thesis is to bridge the gap between the lack of academic writing on the professional practice of the Australian comic industry. In order to achieve this, I explored and learned the methods these prominent and professional US writers and artists use. Compared to the American industry, the creating of comic books in Australia has rarely been documented, particularly in a formal capacity or from a contemporary perspective. The process I used was to navigate through the research and studio practice from the perspective of a solo artist with an interest to learn, and to develop into an artist with a firmer understanding of not only the medium being engaged, but the context in which the medium is being created. -
Alumni Relations Provides a Vehicle to Further Engage Graduates Who Have a Vested Interest in Our Local Schools
▌INVOLVEMENT Broadening Community-Based Support Alumni Relations provides a vehicle to further engage graduates who have a vested interest in our local schools. It allows us to utilize successful graduates as role models and provides a venue for alumni to build relationships with other classmates. Behind every great Miamian there’s a teacher. Senator Bob Graham (Miami Senior High, Class of 1955) salutes his most inspiring teacher, Lamar Louise Curry Miami-Dade County Public Schools alumni.dadeschools.net Miami-Dade County Public Schools Alumni Hall of Fame Inaugural Inductees A panel of community leaders met May 11, 2011 to select the first inductees into the District’s new Alumni Hall of Fame. The panel chose by consensus the following alumni in established categories: Arts & Entertainment Andy Garcia Actor Miami Beach Senior High School (Class of 1974) Nautilus Junior High School Biscayne Elementary School Business Jeffrey Preston Bezos Founder & CEO, Amazon.com Miami Palmetto Senior High School (Class of 1982) Public Service Bob Graham Former Florida Governor Former U.S. Senator Miami Senior High School Science, Technology, Engineering & Math Wendy Chung, M.D., Ph.D. Molecular Geneticist Assistant Professor for Pediatrics, Columbia University Medical Center Westinghouse Science Prize Winner Miami Killian Senior High School (Class of 1986) Glades Middle School Kenwood Elementary School Sports Andre Dawson Major League Baseball Hall of Famer Southwest Miami Senior High School (Class of 1972) South Miami Junior High School Singular Achievement Dr. Dorothy Jenkins Fields Historian, Preservationist, retired M-DCPS Librarian Booker T. Washington High School (Class of 1960) Phillis Wheatley Elementary School Miami-Dade County Public Schools Alumni Hall of Fame Inaugural Inductees In addition to naming an inductee in each established category, the panel also chose to award a special citation to the four M-DCPS alumni who have flown in space as U.S. -
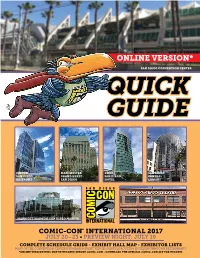
Online Version*
ONLINE VERSION* SAN DIEGO CONVENTION CENTER QUICK GUIDE HILTON MANCHESTER OMNI SAN DIEGO SAN DIEGO GRAND HYATT SAN DIEGO CENTRAL BAYFRONT SAN DIEGO HOTEL LIBRARY MARRIOTT MARQUIS SAN DIEGO MARINA COMIC-CON® INTERNATIONAL 2017 JULY 20–23 • PREVIEW NIGHT: JULY 19 COMPLETE SCHEDULE GRIDS • EXHIBIT HALL MAP • EXHIBITOR LISTS MAPS OF THE CONVENTION CENTER/PROGRAM & EVENT VENUES/SHUTTLE ROUTES & HOTELS/DOWNTOWN RESTAURANTS *ONLINE VERSION WILL NOT BE UPDATED BEFORE COMIC-CON • DOWNLOAD THE OFFICIAL COMIC-CON APP FOR UPDATES COMIC-CON INTERNATIONAL 2017 QUICK GUIDE WELCOME! to the 2017 edition of the Comic-Con International Quick Guide, your guide to the show through maps and the schedule-at-a-glance programming grids! Please remember that the Quick Guide and the Events Guide are once again TWO SEPARATE PUBLICATIONS! For an in-depth look at Comic- Con, including all the program descriptions, pick up a copy of the Events Guide in the Sails Pavilion upstairs at the San Diego Convention Center . and don’t forget to pick up your copy of the Souvenir Book, too! It’s our biggest book ever, chock full of great articles and art! CONTENTS 4 Comic-Con 2017 Programming & Event Locations COMIC-CON 5 RFID Badges • Morning Lines for Exclusives/Booth Signing Wristbands 2017 HOURS 6-7 Convention Center Upper Level Map • Mezzanine Map WEDNESDAY 8 Hall H/Ballroom 20 Maps Preview Night: 9 Hall H Wristband Info • Hall H Next Day Line Map 6:00 to 9:00 PM 10 Rooms 2-11 Line Map THURSDAY, FRIDAY, 11 Hotels and Shuttle Stops Map SATURDAY: 9:30 AM to 7:00 PM* 14-15 Marriott Marquis San Diego Marina Program Information and Maps SUNDAY: 16-17 Hilton San Diego Bayfront Program Information and Maps 9:30 AM to 5:00 PM 18-19 Manchester Grand Hyatt Program Information and Maps *Programming continues into the evening hours on 20 Horton Grand Theatre Program Information and Map Thursday through 21 San Diego Central Library Program Information and Map Saturday nights. -

Sunday at Comic Con Files/SDCC Sundays Newsletter.Pdf
T O D AY Daily Newsletter of Comic-Con International Sunday, July 15, 2012 Featuring: * Highlights * Last Minute Updates * Autograph Info * Anime and Film Schedule * Programming Grids * Photo Gallery * And More Inside! Top left: Crowds swarm into the Gaslamp Quarter as the convention winds down for the day. Top right: Cartoon voice actress Debi Derryberry entertains a packed room with her impressions of Snow White. For a complete Middle left: Lucky fan Mike Castelo got a personal recognition from Chris Hardwick (The Nerdist) during the Warner Bros. presentation. Middle right: The 501st Legion gathers for their annual Comic-Con picture. listing of all things Bottom left: Keith Knight participates in his first ever Quick Draw with Scott Shaw!, SergioAragonés, and Mark Evanier. Comic-Con, see the Bottom center: Aaron Paul gets in a Fan’s face at the Breaking Bad signing. Bottom right: The Rellama familty stays together by cosplaying together. Events Guide. ©2012 Viacom, International, Inc. All Rights Reserved. PDF processed with CutePDF evaluation edition www.CutePDF.com SUNDAY PROGRAMS PANELS FOR KIDS OF ALL AGES SUNDAY ANIME • FILM FESTIVAL 10 11 12 1 2 3 4 5 COMIC-CON New Methods in Jim Lee in ANIME SCREENINGS • MARRIOTT MARQUIS & MARINA COMIC-CON From Manuscript From Book in Print HOW-TO Digital Painting and Coloring Conversation with INTERNATIONAL ROOM 2 to Industry to Reader’s Hand MARRIOTT HALL 4 MARRIOTT HALL 5 MARRIOTT HALL 6 with Brian Haberlin Scott Brick INDEPENDENT Keenspot 2012: 10:00 Someday’s Dreamers 10:00 Clamp School Detectives -

Marvel September to December 2021
MARVEL Marvel's Black Widow: The Art of the Movie Marvel Comics Summary After seven appearances, spanning a decade in the Marvel Cinematic Universe, Natasha Romanoff , a.k.a. the Black Widow, takes the lead in an adventure unlike any other she's known before. Continuing their popular ART OF series of movie tie-in books, Marvel presents another blockbuster achievement! Featuring exclusive concept artwork and in-depth interviews with the creative team, this deluxe volume provides insider details about the making of the highly anticipated film. Marvel 9781302923587 On Sale Date: 11/23/21 $50.00 USD/$63.00 CAD Hardcover 288 Pages Carton Qty: 16 Ages 0 And Up, Grades P to 17 Comics & Graphic Novels / Superheroes CGN004080 27.6 cm H | 18.4 cm W The Marvels Vol. 1 Kurt Busiek, Yildiray Cinar Summary Kurt Busiek (MARVELS) is back, with the biggest, wildest, most sprawling series you’ve ever seen — telling stories that span decades and range from cosmic adventure to intense human drama, from street-level to the far reaches of space, starring literally anyone from Marvel’s very first heroes to the superstars of tomorrow! Featuring Captain America, Spider-Man, the Punisher, the Human Torch, Storm, the Black Cat, the Golden Age Vision, Melinda May, Aero, Iron Man, Thor and many more — and introducing two brand-new characters destined to be fan-favorites — a thriller begins that will take readers across the Marvel Universe…and beyond! Get to know Kevin Schumer, an ordinary guy with some big secrets — and the mysterious Threadneedle as well! But who (or what) is KSHOOM? It all starts here. -

Frankfurt 2015 Rights Guide
Frankfurt 2015 Rights Guide www.apub.com For Global Rights inquiries, please contact: Jennifer Bassuk—Director, Global Rights Jodi Marchowsky—Manager, Global Rights Alexandra Levenberg—Manager, Global Rights Amazon Publishing 1350 Avenue of the Americas, 17th Floor New York, New York 10019 [email protected] Rights Guide Table of Contents 47North . 3 Amazon Publishing . 22 French and German Titles — Amazon Publishing . 29 Grand Harbor Press . 41 Jet City Comics . 45 Lake Union Publishing . 51 Little A . .82 Montlake Romance . 92 StoryFront . 123 Thomas & Mercer . 129 Waterfall . 165 For information about our backlist titles, please refer to our backlist rights guide, which is available on our website at www.apub.com. For Media Inquiries, please contact: [email protected] 2 This Way to the New Unknown 47North, whose name is based on the latitude coordinates for Seattle, offers a wide array of new novels and cult favorites for avid readers of science fiction, fantasy, and horror. 3 Seed Ania Ahlborn Horror Publication Date: 7/17/2012 Page Count: 246 Rights Available: All Languages Rights Sold: German Seed plants its page-turning terror deep in your soul, and lets it grow wild. With nothing but the clothes on his back—and something horrific snapping at his heels—Jack Winter fled his rural Georgia home when he was still just a boy. Watching the world he knew vanish in a trucker’s rearview mirror, he thought he was leaving an unspeakable nightmare behind forever. But years later, the bright new future he’s built suddenly turns pitch black, as something fiendishly familiar looms dead ahead. -

Justice League Vol. 2: Outbreak (Rebirth) Summary a Part of DC Universe: Rebirth!
PRHPS - Graphic Novel & Manga Newsletter May 2017 Justice League Vol. 2: Outbreak (Rebirth) Summary A part of DC Universe: Rebirth! Spinning directly out of the events of DC UNIVERSE: REBIRTH, a new day dawns for the Justice League as they welcome a slew of new members into their ranks. The question remains though, can the world’s greatest superheroes trust these new recruits? And will the members of League be able to come together against an ancient evil that threatens to reclaim not just the world, but the entire universe! Masterful storytelling, epic action, and unbelievable art come together in JUSTICE LEAGUE from best-selling comic book writer Bryan Hitch (JLA) and superstar artist Tony S. Daniel (BATMAN, DETECTIVE COMICS). Collects JUSTICE LEAGUE #6-11. Rebirth honors the richest history in comics, while continuing to look towards the future. These are the most innovative and modern stories featuring the DC Comics world’s greatest superheroes, told by some of the finest storytellers in the 9781401268701 business. On Sale Date: 5/2/2017 $16.99 Honoring the past, protecting our present, and looking towards the future. This Trade Paperback is the next chapter in the ongoing saga of the DC Universe. The legacy 144 Pages continues. Comics & Graphic Novels / Superheroes Territory: World except UK/Ireland Status:ACTIVE PRHPS - Graphic Novel & Manga Newsletter May 2017 Justice League Unwrapped by Jim Lee Summary SUPERSTAR ARTIST JIM LEE BRINGS TOGETHER THE WORLD’S GREATEST HEROES…FOR THE FIRST TIME! It’s the dawn of a new age. Superheroes—like Superman in Metropolis and Gotham’s Dark Knight, Batman—are new and frightening to the world at large. -

Previews #323 (Vol
PREVIEWS #323 (VOL. XXV #8, AUG15) PREVIEWS PUBLICATIONS PREVIEWS #325 OCTOBER 2015 SAME GREAT PREVIEWS! NEW LOWER PRICE: $3.99! Since 1988, PREVIEWS has been your ultimate source for all of the comics and merchandise to be available from your local comic book shop… revealed up to two months in advance! Hundreds of comics and graphic novels from the best comic publishers; the coolest pop-culture merchandise on Earth; plus PREVIEWS exclusive items available nowhere else! Now more than ever, PREVIEWS is here to show the tales, toys and treasures in your future! This October issue features items scheduled to ship in December 2015 and beyond. Catalog, 8x11, 500+pg, PC SRP: $3.99 MARVEL PREVIEWS VOLUME 2 #39 Each issue of Marvel Previews is a comic book-sized, 120-page, full-color guide and preview to all of Marvel’s upcoming releases — it’s your #1 source for advanced information on Marvel Comics! This October issue features items scheduled to ship in December 2015 and beyond. FREE w/Purchase of PREVIEWS Comic-sized, 120pg, FC SRP: $1.25 PREVIEWS #325 CUSTOMER ORDER FORM — OCTOBER 2015 PREVIEWS makes it easy for you to order every item in the catalog with this separate order form booklet! This October issue features items scheduled to ship in December 2015 and beyond. Comic-sized, 62pg, PC SRP: PI COMICS SECTION PREMIER VENDORS DARK HORSE COMICS ABE SAPIEN #27 Mike Mignola (W/Cover), Scott Allie (W), Alise Gluškova (A/C), and Dave Stewart (C) Abe’s memories of his life as a man in the nineteenth century come to the surface as secret societies fight over an object that could prove the true origins of the human race! FC, 32 pages SRP: $3.50 B.P.R.D. -

Dc Entertainment Aug20 7071 Action Comics #1026 Cvr A
DC ENTERTAINMENT AUG20 7071 ACTION COMICS #1026 CVR A JOHN ROMITA JR & KLAUS JANSON $3.99 AUG20 7072 ACTION COMICS #1026 CVR B LUCIO PARRILLO VAR $3.99 AUG20 7073 ACTION COMICS #1026 CVR C FRANK CHO WONDER WOMAN 1984 VAR $3.99 AUG20 7026 AMERICAN VAMPIRE 1976 #1 (OF 9) CVR A RAFAEL ALBUQUERQUE (MR) $3.99 AUG20 7027 AMERICAN VAMPIRE 1976 #1 (OF 9) CVR B DUSTIN NGUYEN VAR $3.99 AUG20 7028 AMERICAN VAMPIRE 1976 #1 (OF 9) CVR C BLANK (MR) $3.99 AUG20 7077 AMETHYST #6 (OF 6) $3.99 AUG20 7078 AQUAMAN #64 CVR A ROBSON ROCHA & DANIEL HENRIQUES $3.99 AUG20 7079 AQUAMAN #64 CVR B GILBERT VIGONTE VAR $3.99 AUG20 7014 BATGIRL #50 CVR A JOSHUA MIDDLETON $5.99 AUG20 7015 BATGIRL #50 CVR B TERRY DODSON & RACHEL DODSON VAR $5.99 AUG20 7001 BATMAN #100 CVR A JORGE JIMENEZ WRAPAROUND (JOKER WAR) $6.99 AUG20 7002 BATMAN #100 CVR B FRANCESCO MATTINA CARD STOCK VAR (JOKER WAR) $7.99 AUG20 7004 BATMAN #100 CVR C PURPLE BLANK VAR (JOKER WAR) $6.99 AUG20 7005 BATMAN #101 CVR A GUILLEM MARCH $3.99 AUG20 7006 BATMAN #101 CVR B FRANCESCO MATTINA CARD STOCK VAR $4.99 AUG20 7007 BATMAN #101 CVR C J SCOTT CAMPBELL WONDER WOMAN 1984 VAR $3.99 AUG20 7087 BATMAN & THE OUTSIDERS #17 CVR A TYLER KIRKHAM $3.99 AUG20 7088 BATMAN & THE OUTSIDERS #17 CVR B SANFORD GREENE VAR $3.99 AUG20 7080 BATMAN BEYOND #48 CVR A DAN MORA $3.99 AUG20 7081 BATMAN BEYOND #48 CVR B FRANCIS MANAPUL VAR $3.99 AUG20 7084 BATMAN SUPERMAN #13 CVR A DAVID MARQUEZ $3.99 AUG20 7085 BATMAN SUPERMAN #13 CVR B MARK BROOKS CARD STOCK VAR $4.99 AUG20 7086 BATMAN SUPERMAN #13 CVR C JENNY FRISON WONDER WOMAN -
Program Book September 27-28, 2014
LONG BEACH COMIC CON LOGO 2014 PROGRAM BOOK SEPTEMBER 27-28, 2014 FEATURING: Mike & Laura Allred Sandy King Carpenter Amanda Conner Gerry Conway Bob Layton Mike Mignola James O’Barr Jimmy Palmiotti Marc Silvestri Richard Starkings and more! UM O Long Beach Comic Con is proudly sponsored by Scan this code with your phone to get the latest program book. LOLA XOXO ©2014 SIYA ©2014 SIYA LOLA XOXO welcomeletter elcome to the Sixth Annual Long Beach Comic Con! We hope you’ll agree that this year we’ve really pumped up the volume Won our programming, guests and exhibitors. We’re very proud STAFF to introduce our new Hero Complex Theater and our incredible Kids Programming that features a LEGO Fun Zone, laser tag, a gaming area MArtHA DONATO for the entire family, and much more! And don’t forget to visit Cosplay Executive Director Corner to see and hang out with some of your favorite costumed PHIL LAWRENCE characters. Sales Director This weekend, you’ll find some of most talented creators from the GABE FIERAMOSCO worlds of comics, animation and horror – all under one roof! Add to Marketing Manager that a fabulous blend of exhibitors from the comics and pop culture world, plus an array of entertainment that will keep you hoppin’ all STEVE HOVEKE day long. Security Director Keep in mind, Artist Alley is still the centerpiece of the exhibit floor. DAVID HYDE Don’t miss this unique chance to meet your favorite artists, writers and Press & Guest Relations creators as well as opportunities to discover new talent. -

NOVEDADES Eccediciones.Com TM & © DC Comics
© 2008 by CARLSEN VERLAG GMBH, Hamburg © 2008 by CARLSEN ABRIL 2013 << NI PUTA GRACIA COMUNICADO DE NOVEDADES eccediciones.coM TM & © DC Comics ANTES DE WATCHMEN: MINUTEMEN núm. 5 (de 6) GUION DARWYN COOKE + JOHN HIGGINS DIBUJO DARWYN COOKE + JOHN HIGGINS EDICIÓN ORIGINAL Before Watchmen: Minutemen núm. 5 USA PERIODICIDAD Mensual FORMATO 32 págs. | Grapa | Color | 168x257 mm. PVP 2,50 € De la mano de los mejores artistas de la industria del cómic, llega a nosotros Antes de Watchmen, una genial colección de series limitadas y números especiales que indagan en el mundo de Watchmen y sus personajes, con un respeto absoluto hacia la obra original. En Minutemen, con firma del magistral Darwyn Cooke, asistimos a la creación y el desarrollo del mítico primer equipo de superhéroes del universo Watchmen. EL HOMENAJE DE LA GENERACIÓN AL CÓMIC QUE CRECIÓ CON WATCHMEN eccediciones.com MÁS IMPORTANTE DE LA HISTORIA 9 7 8 8 4 1 5 8 4 4 1 5 0 TM & © DC Comics ANTES DE WATCHMEN: EL COMEDIANTE núm. 5 (de 6) GUION BRIAN AZZARELLO + JOHN HIGGINS DIBUJO J.G. JONES + JOHN HIGGINS EDICIÓN ORIGINAL Before Watchmen: Comedian núm. 5 USA PERIODICIDAD Mensual FORMATO 32 págs. | Grapa | Color | 168x257 mm. PVP 2,50 € De la mano de los mejores artistas de la industria del cómic, llega a nosotros Antes de Watchmen, una genial colección de series limitadas y números especiales que indagan en el mundo de Watchmen y sus personajes, con un respeto absoluto hacia la obra original. En esta serie, Brian Azzarello y J.G. Jones nos narran las inclasificables aventuras del Comediante, sin duda uno de los personajes más tridimensionales y polémicos del universo Watchmen.