A Distalising Tibial Tubercle Osteotomy for Patellar
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2 0 1 2 Media Guide
2 0 1 2 MEDIA GUIDE www.SCCA.com CONTENTS 2 Letter from the President 3 What is SCCA? 4 SCCA Club Racing National Staff 5 SCCA Club Racing Style Guide 6 SCCA Sponsors 10 Club Racing Categories and Classes 14 The Structure of Club Racing 15 SCCA Divisions 16 The SCCA National Championship Runoffs® 19 The Future of Club Racing 20 BFGoodrich Tires Super Tour 21 SCCA Club Racing Super Sweep Winners 22 2011 National Champions 28 Former National Champions 47 Inactive Class National Champions 61 Multiple National Championships 63 Consecutive Championships 64 Multiple Class Champions 74 Runoffs Pole Winners 91 Inactive Class Pole Winners 102 Multiple Pole Winners 104 Consecutive Poles 105 Miscellaneous Records 106 Manufacturer Records 110 Runoffs Lap Records 114 Divisional Championship Records 116 National Point Championships 119 Major Club Racing Awards 131 BFGoodrich Tires Worker of the Year SCCA Club Racing (800) 770-2055 FAX (785) 232-7214 www.SCCA.com © Copyright 2012 Sports Car Club of America, Inc. 2012 SCCA® Club Racing Media Guide 1 Dear SCCA Media Partners: Welcome to another extraordinary season of SCCA Club Racing, the highest-caliber grassroots racing program in North America. Not content to stay stagnate, our Club Racing program continues to evolve. In 2011, we began the BFGoodrich Tires SCCA Super Tour program. With the help of our partner, BFGoodrich Tires, the series expanded to nine events for 2012, and included one special event in each division. These race weekends featured elements that aren’t always available at National Races, adding to the competitors’ experi- ence. We also unveiled the Majors program in the middle part of the coun- try this season, giving racers in the Rocky Mountain, Midwest and Southwest Divisions an opportunity to run for a larger championship without having to travel the country. -

Fast Parts for Faster Cars
BATBATBAT Fast Parts For Faster Cars Formula Ford 1600 Club Ford 1600 Ford 2000 Sports 2000 4 -Cylinder Ford Powered Parts Catalog BAT - your headquarters for FF1600 & FF2000 2 A word from Peter One July afternoon in 1967 I stood at the Paddock Bend of Brands Hatch Race Track in England and watched 14 freshly painted single-seat race cars take to the track driven by a bunch of unknown drivers, hopeful I'm sure that this could be the start of a successful career as a racing driver. I felt a tingle of excitement myself and a feeling that somehow these little, affordable, cars would finally bring me into a more active role in motor racing. That race was the first Formula Ford race ever held in the world, from which grew a legendary training ground for many modern greats in motor sport. World Champions such as James Hunt, Jody Schecter, Aryton Senna and Emerson Fittipaldi all cut their teeth in Formula Ford. The list of famous Formula Ford "graduates" worldwide is too long to mention here, but impressive it is. Formula Ford has now grown into other step-up formula such as Formula Ford 2000, Sports 2000 and yes, even Formula Atlantic. Since Formula Ford allowed me to become active in motor racing and because I was always helping out my fellow competitors in the USA by acquiring hard to get racing equipment from my native England, it was only natural that British American Transfer or BAT as you know us would evolve. Throughout the years we have expanded our racing expertise beyond Formula Ford to all 4 Cylinder Ford based racing cars. -
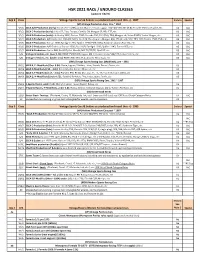
HSR 2021 RACE / ENDURO CLASSES (Updated 1/8/21)
HSR 2021 RACE / ENDURO CLASSES (updated 1/8/21) Grp 2 Class Vintage Sports Cars & Sedans as produced and raced thru +/- 1967 Enduro Special (VP) Vintage Production Cars, thru ~ 1967 VP/1 SCCA A/B-Production (early): Corvette C-1 (283); Aston Martin; Ferrari; Jaguar 120/140/150, XKE (3.8); Porsche 356 Carrera/GS, etc. V3 IAC VP/2 SCCA C-Production (early): Lotus S7, Elan, Europa; Ginetta G4; Morgan SS; Alfa GTZ, etc. V3 IAC VP/3 SCCA D-Production (early): A-Healey 3000; Datsun 2000; Porsche 356, 911 (FIA); TR4; Morgan +4; Volvo P1800; Yenko Stinger, etc. V4 IAC VP/4 SCCA E-Production: A/R Giulia; A-H 100-4/6; MGB; Fiat 124; Elva Courier; Morgan 4/4; 356 (drum), 912; TR3, GT6; Turner 1500; TVR, etc. V5 IAC VP/5 SCCA F-Production: Datsun 1600; Spridget 1275; Spitfire 1296/1500; MGA; Sunbeam Alpine; Fiat 124, etc. V5 IAC VP/6 SCCA G-Production: A/R Giulietta; Datsun 1500; Fiat X1/9; Spridget 1100; Spitfire 1147; Turner 950, etc. V5 IAC VP/7 SCCA H-Production: Sprite 948; Fiat 850; Fiat Abarth; MG TC/TD/TF; Opel GT, etc. V5 IAC S/5 Vintage B-Sedans, etc. (over 1.5L): BMW 1500/1600; Jaguar Mk II; Corvair; Volvo 544/122; Lotus Cortina, etc. V4 IAC S/6 Vintage C-Sedans, etc. (under 1.5L): BMW 700; Mini; Fiat; Abarth; NSU; Saab, etc. V5 IAC (VM) Vintage Sports Racing Cars (Modifieds), pre ~ 1961 VM/1 SCCA B, C -Modifieds (Over 3.0L): Devin, Jaguar; Echidna; Lister; Scarab; Ferrari; Bocar, etc. -

Tiga Cars Media Information
Tiga Media Information For immediate release Press Release First Public Appearance of the Tiga CN212B Brands Hatch, UK, 25th July 2013: This weekend sees the new Tiga CN212B alongside the CN212A at Rounds 3 & 4 of the Speed Euroseries at Brands Hatch, Fawkham, Kent. Orex Competition will be fielding both models of the Tiga CN12 stable with Mike Newton and Alan Bonner behind the wheel of the CN212A Car 61 and the updated Tiga CN212B Car 59 driven by Alex Champkin and Australian, Roman Krumins. The wet British summer, until the last two weeks heatwave, has limited the testing of the new development parts on the Tiga CN212A, so it was decided to debut the Tiga CN212B, which has also had suspension updates over the summer months. Mike Newton will be co-driving this weekend with experienced GT racer, Alan Bonner. Mike's regular partner, Dean Stirling unable to change his other commitments when the dates for these rounds changed. Roman Krumins from Australia joins the team for the first time and is partnered by 2012 Clubmans BARC Cup Champion Alex Champkin. Roman and all the team drivers have been familiarising themselves with the Brands Hatch GP circuit on the Tiga Cars simulator at Tiga's Cheshire base. Both cars will be sporting the now iconic “AD NetVu Connected” red, white and blue livery for AD Team Tiga. • QUOTES Mike Newton (Tiga Cars) : “We have been very frustrated by the weather, as we have made a number of exciting and significant changes to both the mechanical and aero package of the CN212A, and had such limited opportunities for dry weather testing. -

Club Racing Media Guide and Record Book
PLAYGROUND EARTH BEGINS WHERE YOUR DRIVEWAY ENDS. © 2013 Michelin North America, Inc. BFGoodrich® g-ForceTM tires bring track-proven grip to the street. They have crisp steering response, sharp handling and predictable feedback that bring out the fun of every road. They’re your ticket to Playground EarthTM. Find yours at bfgoodrichtires.com. Hawk Performance brake pads are the most popular pads used in the Sports Car Club of America (SSCA) paddock. For more, visit us at www.hawkperformance.com. WHAT’SW STOPPING YOU? Dear SCCA Media Partners, Welcome to what is truly a new era of the Sports Car Club of America, as the SCCA National Champi- onship Runoffs heads west for the first time in 46 years to Mazda Raceway Laguna Seca. This event, made possible with the help of our friends and partners at Mazda and the Sports Car Rac- ing Association of the Monterey Peninsula (SCRAMP), was met with questions at its announcement that have been answered in a big way, with more than 530 drivers on the entry list and a rejunvenaton of the west coast program all season long. While we haven’t been west of the Rockies since River- side International Raceway in 1968, it’s hard to believe it will be that long before we return again. The question on everyone’s mind, even more than usual, is who is going to win? Are there hidden gems on the west coast who may be making their first Runoffs appearance that will make a name for themselves on the national stage, or will the traditional contenders learn a new track quickly enough to hold their titles? My guess is that we’ll see some of each. -

Championship Listing
RACE ENTRIES Brands Hatch - October 26/27 2019 Entries as at 12:00 Tuesday October 22nd 2019 # Competitor Entrant/Sponsor Vehicle Hometown Class Aimshop.com Formula Ford Festival 1 Joshua Smith Driver Van Diemen JL13 Nr Milnthorpe Pro 2 Chris Middlehurst Team Dolan Van Diemen LA10 St Helens Pro 3 Peter Dempsey Cliff Dempsey Racing/Turn 3 Motorsport Ray GR15 Chicago Pro 4 Ciaran Haggerty Driver Ray GR14 Elderslie Pro 5 Adam Fathers AF Racing Ray GR16 Swanscombe Pro 6 Peter Hardman Milly Moo Pumpkin Ray GR16 Rockingham Northants Pro 9 Terry Walkingshaw Driver Van Diemen RF03 Poyntzpass Pro 11 Ross Martin Team Dolan, Allied Vehicles Van Diemen RF99 Gartocharn Pro 12 Colm Blackburn MCP Motorsport Car Preparation/Sweeneys Garage/SpiVan Diemen RF00 Ballyfermot Dublin Pro 16 Michael Macpherson Kevin Mills Racing Spectrum 011 Inverness Pro 17 Tom McArthur B-M Racing Medina Sport JL18 Warrington Pro 18 Bryce Aron OLDFIELD MOTORSPORT / IMPERIAL MOTORS JAGUAR Van Diemen JL13 Chicago Pro 21 Josh Green Cliff Dempsey Racing/Team USA Scholarship Ray GR19 Mount Kisco, New York Pro 22 Scott Huffaker Cliff Dempsey Racing/Team USA Scholarship Ray GR18 Menlo Park, California Pro 23 Jonathan Woolridge Cliff Dempsey Racing/ Team Canada Scholarship Ray GR11 Oshawa, Ontario Pro 24 Zachary Vanier Cliff Dempsey Racing / Team Canada Scholarship Ray GR15 Garson, Ontario Canada Pro 27 Ivor McCullough Driver Van Diemen RF00 Ballymena Pro 28 Tom Hawkins Driver Ray GR11 Uxbridge Pro 29 James Hadfield Driver Van Diemen RF03 Shepshed Pro 30 Steve Barlow Veterans Brewing -
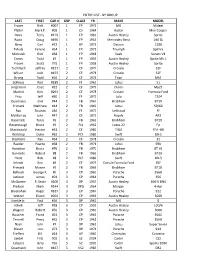
ENTRY LIST - by GROUP LAST FIRST CAR # GRP CLASS YR MAKE MODEL Fraser Rick #007 1 FP 1972 MG Midget Pfaller Mark F
ENTRY LIST - BY GROUP LAST FIRST CAR # GRP CLASS YR MAKE MODEL Fraser Rick #007 1 FP 1972 MG Midget Pfaller Mark F. #09 1 CS 1964 Austin Mini Cooper Davis Terry #119 1 FP 1960 Austin Healey Sprite Radix Doug #190 1 FP 1955 Mercedes-Benz 190 SL Berg Carl #22 1 GP 1971 Datsun 1200 Tirkala Ferenc #54 1 FP 1971 Triumph Spitfire Michalek Rick #68 1 FP 1968 Saab Sonett V4 Crews Todd #7 1 FP 1959 Austin Healey Sprite Mk 1 Fraser Scott #79 1 FP 1958 Austin Healey Sprite Tschiltsch Jeffrey #127 2 CF 1977 Crossle 32F Wilson Josh #155 2 CF 1978 Crossle 32F Strong Todd #16 2 CF 1974 Titan Mk9 Bolhous Rod #189 2 FF 1965 Lotus 51 Jurgenson Jesse #22 2 CF 1979 Dulon Mp21 Madrid Kim #291 2 CF 1978 Crossle Formula Ford Fritz Jeff #30 2 FF 1972 Lola T204 Quadracci Joel #44 2 FB 1967 Brabham BT29 Primack Matthew #44 2 FB 1969 Lotus 59/69 Rao Ricardo #46 2 FF 1972 LeGraud FF McMurray John #47 2 CF 1972 Royale AR3 Kasemets Tonis #6 2 FB 1969 Brabham BT29 Revennaugh Bruce #6 2 FJ1 1962 Lotus 22 Fjr Macdonald Hector #61 2 CF 1980 TIGA FFA -80 Waldrop Duke #62 2 PCF 1989 Swift DB-1 Stephens Ray #64 2 CF 1978 Crossle 32 Raeder Pearce #68 2 FB 1971 Lotus 69b Hamilton Bruce #76 2 FB 1970 Brabham BT 36 Burnside Robert #8 2 FB 1969 Brabham BT29 Hatle Bob #8 2 PCF 1989 Swift DB-3 Inkrott Eric #9 2 CF 1979 Crossle Formula Ford 35F Primack Marvin #9 2 FB 1966 Brabham BT18 Balbach George F. -
We Race Race It.It
SomeSome People People CollectCollect Art...Art... WeWe Race Race It.It. VINTAG R E A C R S A T C R I N O G P S A SS N OCIATIO Setting the New Standard for Vintage Racing Nationwide www.SVRA.com • 1312 Regency Ct, Southlake, TX 76092 VINTAG R E A C R S A T C R I N O G P S SVRA OVERVIEW A SS N OCIATIO Mission Statement The Sports Car Vintage Racing Association, through the establishment of a truly national sanctioning organization, is dedicated to presenting a series of premium racing events at legendary race circuits throughout the United States. By encouraging the principles of safe, fast and enjoyable competition at its events, as well as adherence to period-correct standards of car preparation, the SVRA will continue to keep the rich heritage of motorsports alive for generations of enthusiasts now and into the future. Founded in 1976 Purchased by Parella Motorsports Holdings LLC in September 2012 Purchased HSR West in September 2012 Formed the first and only national vintage racing sanctioning body in the US Largest vintage racing organization in the United States Over 2,500 licensed members Created the U.S. Vintage National Championship Purchased General Racing in July 2014 Formed Vintage Racing Quarterly Magazine LLC in August of 2014 Currently has scheduled 13 events across the United States Traditionally have 11 different race groups at our events Standardized the safety and car preparation rules across the US Launched Vintage Racing Quarterly in October 2014 Pursuit of Passions TV pilot aired in April 2015 Purchased a percentage of the contemporary Trans Am Series in 2016 Driver School licensing program in March 2017 at Roebling Road in Savannah, GA Vintage race cars are the marvels in motorsports, enthusiasts can never get enough: no matter the year, make or model. -

SVRA Cars and Classes
General Outline of Groups and Classes for The WeatherTech® International Challenge with Brian Redman presented by HAWK at Road America ~ 2020 (revised 11/11/19) (1) Can-Am (1965 ~ 1974) Class CA1 Unlimited (including all turbocharged) Class CA2 Small block (over 5.9L) Class CA3 Monocoque (under 5.9L) Class CA4 Tube frame (unlimited) Class CA5 USRRC (1962-1968) Treaded tires (2) (a) Vintage Production Class VAP Vintage A-Production Class VBP Vintage B-Production Class VCP Vintage C-Production Class VDP Vintage D-Production Class VEP Vintage E-Production Class VFP Vintage F-Production Class VHP Vintage G/H-Production Class VBS Vintage B/Sedans (1.5 ~ 1.8L) Class VCS Vintage C/D Sedans (under 1.5L) (b) Vintage Sports Racing Cars Class VCM Vintage C Modified ~ Specials, Sports Racers & Modifieds (over 3000cc) Class VEM Vintage D/E Modified ~ Specials, Sports Racers & Modifieds (1600-3000cc) Class VFM Vintage F Modified ~ Specials, Sports Racers & Modifieds (1100-1500cc) Class VGM Vintage G Modified ~ Specials, Sports Racers & Modifieds (850-1100cc) Class VHM Vintage H Modified ~ Specials, Sports Racers & Modifieds (under 850cc) Class VDSR Vintage D Sports Racers (under 1.0L) (c) Post Historic Street Stock Class SSD Post Historic Street Stock; Firehawk, Escort Series, IT, etc. as appropriate (4) (a) Monoposto Classic Formula Cars (thru ~ 1972) Class VFA Formula 2 & pre 1966 Formula 1 Class VFB Formula B Class VFC Formula C & Later Formula Junior Class VFF Pre-1973 Formula Ford (Dunlop/Avon/Hoosier spec tires, steel wheels only) Class VFJ Formula Junior (Dunlop L tires) Class VFV Formula V, Front Engine Formula Junior (b) Monoposto Formula 70, post 1972, etc. -

The Scca® National Championship Runoffs®
2016 Media Guide CONTENTS 3 What is SCCA? 4 SCCA Club Racing National Staff 4 SCCA Club Racing Style Guide 5 SCCA Sponsors 7 Club Racing Categories and Classes 9 The Structure of Club Racing 9 SCCA Divisions 10 The SCCA National Championship Runoffs® 11 The Future of Club Racing 12 SCCA Club Racing Super Sweep and Winners 12 U.S. Majors Tour 14 2015 National Champions 17 Former National Champions 23 Inactive Class National Champions 30 Multiple National Championships 31 Consecutive Championships 32 Multiple Class Champions 36 Runoffs Pole Winners 41 Inactive Class Pole Winners 47 Multiple Pole Winners 48 Consecutive Poles 49 Miscellaneous Records 49 Manufacturer Records 51 Mid-Ohio Lap Records 53 National Point Championships 55 U.S. Majors Tour Point Championships 60 Major Club Racing Awards 65 Worker of the Year SCCA Club Racing (800) 770-2055 FAX (785) 232-7214 www.SCCA.com © Copyright 2016 Sports Car Club of America, Inc. 2 2016 SCCA® Club Racing Media Guide WHAT IS SCCA®? Sports Car Club of America, Inc. was founded in 1944 by a group of amateur motorsports enthusiasts and today boasts nearly 67,500 members. SCCA now sanctions more than 2,000 amateur and professional motorsports events each year. With 115 regional chapters covering the entire United States, Guam and Puerto Rico, SCCA provides true grassroots participation and is the largest active motorsports membership organization in the world. Local events at nearby circuits remain the backbone of Club activities. SCCA’s volunteer staff provides everything from course marshaling to timing and scoring at both Club and professional events. -

2019 January Historic Torque
The Official Journal of the Historic Racing Car Club (Queensland) Inc. August, 2019 Coming Events Sydney Master Blast Aug 31 - Sep 1 HSCC Baskerville Historics Sept 21 -22 HSRCA Spring Festival Sept 28 -29 CAMS Qld State Champ. Sept 28 -29 VHRR Historic Sandown Oct 25 - 27 Noosa Hillclimb - Summer Nov 9 - 10 See Back Page for more info Noosa Hillclimb Summer It is just a few months away now and although entry is not open yet, it is time to plan and prepare. Organizers are seeking to attract 1963 to 1973 V8 powered MUSCLE CARS and there may be some entry incentives offered as an enticement. It is also the last opportunity for HRCC members to grab some points towards the 2019 club championship trophies so don’t miss it. Even if you are not running a car, support the club and go as a spectator. It makes a great day trip out from Brisbane in a great setting while being a relaxed carnival event. If you don’t want to trek up the hill, there are regular bus rides. Stay tuned for more news….. Kevin Bartlett at HRCC Social Night Living Australian motorsport legends are becoming rare on the ground these days, so HRCC members and friends were treated to something special when Kevin Bartlett ran through the years and cars of his racing career. As he is known to do, Kevin gave a frank and at times, humorous account of his passion to drive race cars as often as he could. And unabashed, he stated that the only cars he wanted to talk about on the night were open wheel cars which were to see him a two time winner of the Australian Drivers Championship, a winner of the Macau Grand Prix, the first ever driver to secure a 100mph lap at Mt Panorama in a Repco Brabham BT11, driving an Indy car at Indianapolis USA as well as many other achievements. -

Anthony Lazzaro
PIERRE KAFFER Birthdate: November 7, 1976 Birthplace: Bad-Neuenahr-Ahrweiler, Germany Height/Weight: 5-7, 150 pounds Residence: Salenstein, Switzerland Family: Single Team (Class): Risi Competizione – Ferrari F430 GT (GT2) Websites: pierre-kaffer.com, risicompetizione.com PR Contact: Fiona Miller +44-777-037-1332 [email protected] Special Interests: Mountain biking, karting, fitness Pierre Kaffer is returning to American Le Mans Series GT2 action in 2009 beginning at Sebring with Risi Competizione behind the wheel of the Ferrari F430. … A two-time overall winner in the Series, he will team with Jaime Melo to contest for the GT2 title. … A former Audi factory driver who has seen stints in the Series with Farnbacher Loles Racing, JMB Racing and Audi. 2009: At Sebring, teamed with Mika Salo/Jaime Melo for his first race with Risi Competizione. The trio kept Ferrari F430 GT clean on track and the crew performed flawless pit stops for team’s second Sebring win in three seasons. … At St. Petersburg, started first in GT2 after Melo’s pole run. Gave way to Wolf Henzler’s Porsche before front suspension snapped and broke under braking at Turn 1 after 27 laps. … At Long Beach, finished second in class despite starting from rear of grid after Melo pole run (ride-height violation). Advanced from 11th in class at start to fifth before pit stop. … At Utah, started second in GT2 but knocked to rear in incident with BMW M3 at start. No damage but team changed tires and cleaned out radiator on fifth lap to avoid overheating. Drove back third-place podium finish.