Written Answers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

TBEX FAM Press Tour Preview: PRE-TBEX FAM
TBEX FAM Press Tour Preview: PRE-TBEX FAM Region: North-West Dates: Depart for Donegal on Saturday, 28th September and return to Dublin on Tuesday, 01st October Duration: 3 full days’ tour plus travel time A Voyage through from the Northerly tip of the Wild Atlantic Way through the scenic wilderness of Donegal and into Sligo known as ‘The Land of Heart’s Desire,’ Iconic cliffs, spectacular, heart-stopping coastline, rich Gaelic culture &’ craic’, surfers’ heaven and then ‘catch-cook’ your own supper (Seriously!) Picture it. A dazzling three-hundred kilometre indented coastline, mysterious stone forts, unspoiled, rugged countryside, miles and miles of beaches and quiet untravelled roads, Donegal, in the remote North West corner, has a different vibe to the rest of Ireland. People connect with its distinctive culture and gentle charm and savour its remote, unspoiled and off-the-beaten track location. A change in tempo and it’s off to Sligo for a full-on day of activity. W.B. Yeats calls Sligo ‘The Land of heart’s desire’ –and it certainly is full of surprises with its untamed beauty and wealth of archaeology. Are you up for a bracing hike to the top of Benbulben Mountain, then some seaweed therapy to re-energise, a seafood feast and a bit of gentle exercise to unwind? Great, let’s get going then… Travel day – Saturday, 28th September Pick-up in Dublin city at 12:30 and Dublin airport at 13:00 & Travel to Donegal: Late lunch in Tankardstown House in Slane, Co. and continue to Donegal Early evening Dinner and Overnight in An Grianan Hotel, Burt, Inishowen Day One – Sunday, 29th September Welcome to Spectacular Inishowen, the largest peninsula in Ireland. -

Inishowen Portfolio
Visiting Burt to Buncrana Page | 1 Contents Introduction - ......................................................................................................................................... 3 Geography & Key Physical Features ................................................................................................... 3 Geology/Soils ...................................................................................................................................... 4 Ecology/Wildlife ................................................................................................................................. 5 Flora and Fauna .................................................................................................................................. 6 Agriculture and Forestry .................................................................................................................... 6 Fishing/ Angling & Maritime Heritage................................................................................................ 7 Historical Sites .................................................................................................................................... 8 Folklore/Myths ................................................................................................................................. 12 Burt Castle Legend ........................................................................................................................ 12 Derivation of Irish Place Names & Locations .................................................................................. -

Inishowen Heritage Trail
HERITAGE TRAIL EXPLORE INISHOWEN Inishowen is exceptional in terms of the outstanding beauty of its geography and in the way that the traces of its history survive to this day, conveying an evocative picture of a vibrant past. We invite you to take this fascinating historical tour of Inishowen which will lead you on a journey through its historical past. Immerse yourself in fascinating cultural and heritage sites some of which date back to early settlements, including ancient forts, castle’s, stone circles and high crosses to name but a few. Make this trail your starting point as you begin your exploration of the rich historical tapestry of the Inishowen peninsula. However, there are still hundreds of additional heritage sites left for you to discover. For further reading and background information: Ancient Monuments of Inishowen, North Donegal; Séan Beattie. Inishowen, A Journey Through Its Past Revisited; Neil Mc Grory. www.inishowenheritage.ie www.curiousireland. ie Images supplied by: Adam Porter, Liam Rainey, Denise Henry, Brendan Diver, Ronan O’Doherty, Mark Willett, Donal Kearney. Please note that some of the monuments listed are on private land, fortunately the majority of land owners do not object to visitors. However please respect their property and follow the Country Code. For queries contact Explore Inishowen, Inishowen Tourist Office +353 (0)74 93 63451 / Email: [email protected] As you explore Inishowen’s spectacular Heritage Trail, you’ll discover one of Ireland’s most beautiful scenic regions. Take in the stunning coastline; try your hand at an exhilarating outdoor pursuit such as horse riding, kayaking or surfing. -
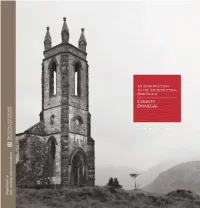
AN INTRODUCTION to the ARCHITECTURAL HERITAGE of COUNTY DONEGAL
AN INTRODUCTION TO THE ARCHITECTURAL HERITAGE of COUNTY DONEGAL AN INTRODUCTION TO THE ARCHITECTURAL HERITAGE of COUNTY DONEGAL COUNTY DONEGAL Mount Errigal viewed from Dunlewey. Foreword County Donegal has a rich architectural seventeenth-century Plantation of Ulster that heritage that covers a wide range of structures became a model of town planning throughout from country houses, churches and public the north of Ireland. Donegal’s legacy of buildings to vernacular houses and farm religious buildings is also of particular buildings. While impressive buildings are significance, which ranges from numerous readily appreciated for their architectural and early ecclesiastical sites, such as the important historical value, more modest structures are place of pilgrimage at Lough Derg, to the often overlooked and potentially lost without striking modern churches designed by Liam record. In the course of making the National McCormick. Inventory of Architectural Heritage (NIAH) The NIAH survey was carried out in phases survey of County Donegal, a large variety of between 2008 and 2011 and includes more building types has been identified and than 3,000 individual structures. The purpose recorded. In rural areas these include structures of the survey is to identify a representative as diverse as bridges, mills, thatched houses, selection of the architectural heritage of barns and outbuildings, gate piers and water Donegal, of which this Introduction highlights pumps; while in towns there are houses, only a small portion. The Inventory should not shopfronts and street furniture. be regarded as exhaustive and, over time, other A maritime county, Donegal also has a rich buildings and structures of merit may come to built heritage relating to the coast: piers, light. -

Conference Prog Sep 16
Tracing Your Irish and Scots-Irish Ancestors Welcome It is my great pleasure to welcome you to Belfast for our September 2016 conference. As the Foundation approaches its sixtieth anniversary I am sure our founders would be delighted to know that their original vision continues to be realised through the Foundation’s contribution to heritage and culture in the province of Ulster and by meeting the aspirations of the Irish diaspora as we help them reconnect with their ancestry. Thank you for helping to make the Foundation’s vision a reality. With delegates travelling from the United States of America, Canada, Australia, New Zealand, England, Northern Ireland and even Luxembourg to be here, we are encouraged that from across the globe you are joining us for what we hope will be a successful week in the archives searching for those elusive Irish and Scots-Irish ancestors. Rest assured that our expert and experienced genealogists will be on hand to assist you in the quest for your Irish roots. For those of you who will be devoting more of your time to taking part in the varied selection of outings to some of our most spectacular and historic locations, we trust you will enjoy the warm welcome, the gentle good humour of the people, and Ulster’s beautiful countryside – one of our best kept secrets. While I can give no guarantee we hope that the weather during the week of our conference will be kind. The summer has been a damp one, so fingers crossed! During your week with us, should you wish to learn more about the Foundation and our work, please do not hesitate to talk to any of our staff. -

Irish Landscape Names
Irish Landscape Names Preface to 2010 edition Stradbally on its own denotes a parish and village); there is usually no equivalent word in the Irish form, such as sliabh or cnoc; and the Ordnance The following document is extracted from the database used to prepare the list Survey forms have not gained currency locally or amongst hill-walkers. The of peaks included on the „Summits‟ section and other sections at second group of exceptions concerns hills for which there was substantial www.mountainviews.ie The document comprises the name data and key evidence from alternative authoritative sources for a name other than the one geographical data for each peak listed on the website as of May 2010, with shown on OS maps, e.g. Croaghonagh / Cruach Eoghanach in Co. Donegal, some minor changes and omissions. The geographical data on the website is marked on the Discovery map as Barnesmore, or Slievetrue in Co. Antrim, more comprehensive. marked on the Discoverer map as Carn Hill. In some of these cases, the evidence for overriding the map forms comes from other Ordnance Survey The data was collated over a number of years by a team of volunteer sources, such as the Ordnance Survey Memoirs. It should be emphasised that contributors to the website. The list in use started with the 2000ft list of Rev. these exceptions represent only a very small percentage of the names listed Vandeleur (1950s), the 600m list based on this by Joss Lynam (1970s) and the and that the forms used by the Placenames Branch and/or OSI/OSNI are 400 and 500m lists of Michael Dewey and Myrddyn Phillips. -

The Heritage Council Annual Report 2016
The Heritage Council Annual Report 2016 The Heritage Council | Annual Report 2016 1 © The Heritage Council 2017 All rights reserved. No part of this book may be printed or reproduced or utilised in any electronic, mechanical, or other means, now known or heretoafter invented, including photocopying or licence permitting restricted copying in Ireland issued by the Irish Copyright Licencing Agency Ltd., The Writers Centre, 19 Parnell Square, Dublin 1. Published by the Heritage Council The Heritage Council of Ireland Series ISBN 978-1-906304-35-5 Photo: Heritage Week 2016 - 'Hands on History 1916' with Jude Stynes, County Offaly. 2 The Heritage Council | Annual Report 2016 © The Heritage Council 2017 All rights reserved. No part of this book may be printed or reproduced or utilised in any electronic, mechanical, or other means, now known or heretoafter invented, including photocopying or licence permitting restricted copying in Ireland issued by the Irish Copyright Licencing Agency Ltd., The Writers Centre, 19 Parnell Square, Dublin 1. Published by the Heritage Council The Heritage Council of Ireland Series ISBN 978-1-906304-35-5 The Heritage Council | Annual Report 2016 3 Contents Chairman’s Message .......................................................................................................................6 Chief Executive’s Report ...................................................................................................................7 1. Introduction ..............................................................................................................................9 -

Irlanda Scozia Inghilterra Viaggi Su Misura
IRLANDA SCOZIA INGHILTERRA VIAGGI SU MISURA IRLANDA SCOZIA INGHILTERRA TOUR INDIVIDUALI E DI GRUPPO APRILE 2016 - MARZO 2017 1 IRLANDA SCOZIA INGHILTERRA IRLANDA DUBLINO 5 BELFAST 8 GIRARE IN IRLANDA NOLEGGIO AUTO 10 FATTORIE/PENSIONI 11 GUESTHOUSE 12 ALBERGHI 13 IRISH COUNTRY HOTELS 14 MANOR HOUSE 15 CASTELLI 16 TOUR IN AUTO 20 TOUR IN TRENO 34 TOUR IN PULLMAN 35 SCOZIA INGHILTERRA LONDRA 42 EDIMBURGO 44 GLASGOW 46 GIRARE IN GRAN BRETAGNA NOLEGGIO AUTO 48 BED & BREAKFAST/ HOTEL 49 CASTELLI E DIMORE 50 TOUR IN TRENO 54 TOUR IN AUTO 56 TOUR IN PULLMAN 69 INFORMAZIONI 78 ASSICURAZIONI 80 CONDIZIONI GENERALI 81 DOCUMENTI PER L’ESPATRIO informazioni relative alla documentazione necessaria Irlanda e Regno Unito fanno parte dell’UE. per l’espatrio prima di prenotare (vedasi art. 13 delle Per i cittadini italiani in visita per motivi di turismo i Condizioni Generali di Contratto) e a verificarne, prima documenti di viaggio e di riconoscimento accettati della partenza, l’aggiornamento presso le competenti sono il passaporto o la carta d’identità valida per autorità. l’espatrio. Anche i minori italiani dovranno essere muniti di documento di viaggio individuale valido per ORA LOCALE l’espatrio (passaporto individuale oppure di carta Un’ora in meno rispetto all’Italia. d’identità). Per le norme relative all’espatrio dei minori comunque si rimanda espressamente a quanto TELEFONO indicato nel sito della Polizia di Stato. Dall’Irlanda e dalla Gran Bretagna si chiama l’Italia con La maggior parte dei cittadini non-UE, anche se prefisso internazionale 0039 seguito dal codice della regolarmente residenti in Italia, necessitano invece città italiana con lo ø e dal numero dell’abbonato. -

Site Name 2018 2019 Altamont # 67,423 73,821 Áras 4,610 5,440 Ardfert Cathedral 11,289 11,815 Athenry Castle 10,993 10,595 Augh
Site Name 2018 2019 Altamont # 67,423 73,821 Áras 4,610 5,440 Ardfert Cathedral 11,289 11,815 Athenry Castle 10,993 10,595 Aughnanure Castle 30,842 31,519 Ballyhack Castle 2,086 2,155 Battle of the Boyne/Oldbridge Est # 355,608 427,148 Blasket Island N# 10,816 8,854 Blasket Visitor Centre 53,115 50,331 Boyle Abbey 6,799 7,935 Bru na Boinne Visitor Centre 60,656 13,730 Newgrange 154,195 162,429 Knowth 46,489 53,179 Dowth N# 17,549 17,093 Cahir Castle 89,715 87,333 Carrowmore 46,766 44,011 Casino Marino Closed 4,941 Castletown House & Parklands # 642,278 965,632 Céide Fields 31,854 30,391 Charles Fort 99,706 97,990 Clonmacnoise 154,330 141,969 Corlea Trackway Visitor Centre 7,750 8,549 Derrynane House and Parklands # 194,794 226,664 Desmond Hall (Desmond Castle Newcastle West) 15,845 12,356 Doe Castle # 29,379 31,439 Doneraile Park # 490,000 490,000 Donegal Castle 56,459 55,310 Dublin Castle 431,340 430,692 Dún Aonghasa 136,042 131,273 Dungarvan Castle 17,434 13,430 Dunmore Cave 36,963 36,199 Durrow Abbey # 4,736 4,776 Emo Court - Parklands and House # 315,204 390,481 Ennis Friary 13,637 14,040 Famine Warhouse # 1,800 1,300 Farmleigh Estate # 389,932 428,925 Ferns Castle 7,132 8,249 Fota Arboretum & Gardens N# 92,750 113,695 Gallarus Castle 49,852 44,470 Garinish Island 69,716 64,919 Glebe House and Gallery 32,169 32,257 Glendalough Visitor Centre & Monument # 732,824 732,362 Grianan of Aileach # 90,435 96,154 Hill of Tara - VC and Gardens # 166,468 208,000 Hore Abbey N# 60,593 75,380 J F Kennedy Arboretum 118,006 128,451 Jerpoint Abbey -

Copyrighted Material
Index A Arklow Golf Club, 212–213 Bar Bacca/La Lea (Belfast), 592 Abbey Tavern (Dublin), 186 Armagh, County, 604–607 Barkers (Wexford), 253 Abbey Theatre (Dublin), 188 Armagh Astronomy Centre and Barleycove Beach, 330 Accommodations, 660–665. See Planetarium, 605 Barnesmore Gap, 559 also Accommodations Index Armagh City, 605 Battle of Aughrim Interpretative best, 16–20 Armagh County Museum, 605 Centre (near Ballinasloe), Achill Island (An Caol), 498 Armagh Public Library, 605–606 488 GENERAL INDEX Active vacations, best, 15–16 Arnotts (Dublin), 172 Battle of the Boyne Adare, 412 Arnotts Project (Dublin), 175 Commemoration (Belfast Adare Heritage Centre, 412 Arthur's Quay Centre and other cities), 54 Adventure trips, 57 (Limerick), 409 Beaches. See also specifi c Aer Arann Islands, 472 Arthur Young's Walk, 364 beaches Ahenny High Crosses, 394 Arts and Crafts Market County Wexford, 254 Aille Cross Equestrian Centre (Limerick), 409 Dingle Peninsula, 379 (Loughrea), 464 Athassel Priory, 394, 396 Donegal Bay, 542, 552 Aillwee Cave (Ballyvaughan), Athlone Castle, 487 Dublin area, 167–168 433–434 Athlone Golf Club, 490 Glencolumbkille, 546 AirCoach (Dublin), 101 The Atlantic Highlands, 548–557 Inishowen Peninsula, 560 Airlink Express Coach Atlantic Sea Kayaking Sligo Bay, 519 (Dublin), 101 (Skibbereen), 332 West Cork, 330 Air travel, 292, 655, 660 Attic @ Liquid (Galway Beaghmore Stone Circles, Alias Tom (Dublin), 175 City), 467 640–641 All-Ireland Hurling & Gaelic Aughnanure Castle Beara Peninsula, 330, 332 Football Finals (Dublin), 55 (Oughterard), -

Elagh Castle CAF Data Structure Report No
Centre for Archaeological Fieldwork School of Geography, Archaeology and Palaeoecology Queen's University Belfast Excavations at Elagh Castle CAF Data Structure Report No. 99 Data Structure Report: Elagh Castle Cormac McSparron Grid Reference: C4158021650 CAF DSR: 99 Contents 1.0 Introduction, summary and acknowledgements 1 2.0 Location and Physical Description of the Site 2 3.0 Historical Background 3 3.1 Introduction 3 3.2 Where is Aileach? 3 3.3 Aileach in Medieval irish Sources 6 Aileach in the Annals Aileach in the Metrical Dindshenchas Aileach in Late Medieval Gaelic praise poetry Other Irish references to Aileach Discussion of the Medieval historical references to Aileach 3.4 References in English sources to Elagh Castle in the 16th 13 and 17th Centuries Map evidence Discussion of the Post-Medieval evidence for Elagh Castle 3.5 Previous Archaeological Investigations at Elagh Castle 17 4.0 Description of the Excavations 4.1 Excavation of Trench 3 Artefacts from Trench 3 4.2 Description of the excavation of Trench 4 Artefacts from Trench 4 4.3 Description of the excavation of Trench 5 Artefacts from trench 5 5.0 Discussion 24 6.0 Conclusion 26 7.0 Recommendations for Further Work 27 8.0 Bibliography 28 1.0 Introduction and summary Elagh Castle survives as a partially collapsed masonry tower constructed upon a rocky outcrop overlooking the city of Derry / Londonderry and the Pennyburn depression to its west. It was in the later middle ages the main castle and residence of the O'Docherty's, although it is uncertain if they were the, original, builders of the castle, it seeming more likely that the existing remains were built in the 14th century before the O'Docherty's held the surrounding territory. -

Uniquely Ireland – a New Irish Experience Every Day
Uniquely Ireland – A New Irish Experience Every Day Jenny O’Neill, Luxury Travel Advisor Email: [email protected] Direct: 858-217-4348 | Mobile 949-290-5944 WWW.IRELANDTRAVELPRO.COM CST # 2131820-40 Crafted Ireland is a luxury leisure division of Custom Ireland www.craftedireland.com Registered Offices: G5 The Steelworks, Foley Street 1, Dublin 1, Ireland| Managing Director: Crothúr Murphy This Tour Features: • Slane Distillery • Boyne Valley • Saint Patricks Centre • Mount Stewart Gardens • Titanic Belfast • Black Cab Tour • Giants Causeway • Derry Walls Walking tour • Glenveagh National Park • Fanad Head light house • Glencolmcille Folk Village • Donegal Castle • Sheep Dog Demo • Sligo Food Trail • Lissadell House • Clonmacnoise • Birr Castle • Kilbeggan Distillery Tour includes: • Sightseeing by luxury coach with professional Driver/guide • All local taxes, hotel service charges & porterage for one suitcase per person Meals Included: • Full daily breakfasts (except Day 1) • 4 Lunches • 3 Dinners Hotels: • Dunboyne Castle, Dublin (1 night) or similar • Europa Hotel, Belfast (1 night) or similar • Maldron Hotel, Derry (1 night) or similar • Lough Eske Castle, Donegal (2 night) or similar • The Glass House, Sligo (1 night) or similar • The K Club, Kildare (1 night) or similar Crafted Ireland is a luxury leisure division of Custom Ireland www.craftedireland.com Registered Offices: G5 The Steelworks, Foley Street 1, Dublin 1, Ireland| Managing Director: Crothúr Murphy Crafted Ireland is a luxury leisure division of Custom Ireland www.craftedireland.com Registered Offices: G5 The Steelworks, Foley Street 1, Dublin 1, Ireland| Managing Director: Crothúr Murphy DAY 1 -Friday - Dublin Arrival, Newgrange (D, L, B&B) Arrive into Dublin – transfer directly to Dunboyne Castle 11.00am Today enjoy a half day touring with your local guide and private Coach, first visit Slane Distillery followed by the Boyne Valley 11.45am First you will visit Slane Distillery which is housed within the 250-year-old stables of the iconic Slane Castle estate.