Dehydration/Oral Rehydration Clinical Practice Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CHALLENGING CASES: BIOPSYCHOSOCIAL PEDIATRICS Failure to Thrive in a 4-Month-Old Nursing Infant
CHALLENGING CASES: BIOPSYCHOSOCIAL PEDIATRICS Failure to Thrive in a 4-Month-Old Nursing Infant* CASE visits she was observed to respond quickly to visual Christine, a 4-month-old infant, is brought to the and auditory cues. There was no family history of office for a health-supervision visit by her mother, serious diseases. a 30-year-old emergency department nurse. The In that a comprehensive history and physical ex- mother, who is well known to the pediatrician to be amination did not indicate an organic cause, the a competent and attentive caregiver, appears unchar- pediatrician reasoned that the most likely cause of acteristically tired. They are accompanied by the 18- her failure to thrive was an unintentional caloric month-old and 4-year-old siblings because child care deprivation secondary to maternal stress and ex- was unavailable, and her husband has been out of haustion. Christine’s mother and the pediatrician town on business for the last 5 weeks. When the discussed how maternal stress, fatigue, and depres- pediatrician comments, “You look exhausted. It must sion could hinder the let-down reflex and reduce the be really tough to care for 3 young children,” the availability of an adequate milk supply, as well as mother appears relieved that attention was given to make it difficult to maintain regular feeding sessions. her needs. She reports that she has not been getting The pediatrician recommended obtaining help with much sleep because Christine wakes up for 2 or more child care and household responsibilities. The evening feedings and the toddler is now awakening mother was also encouraged to consume adequate at night. -

A Dose-Response Relationship Between Organic Mercury Exposure from Thimerosal-Containing Vaccines and Neurodevelopmental Disorders
Int. J. Environ. Res. Public Health 2014, 11, 9156-9170; doi:10.3390/ijerph110909156 OPEN ACCESS International Journal of Environmental Research and Public Health ISSN 1660-4601 www.mdpi.com/journal/ijerph Article A Dose-Response Relationship between Organic Mercury Exposure from Thimerosal-Containing Vaccines and Neurodevelopmental Disorders David A. Geier 1, Brian S. Hooker 2, Janet K. Kern 1,3, Paul G. King 4, Lisa K. Sykes 4 and Mark R. Geier 1,* 1 Institute of Chronic Illnesses, Inc., 14 Redgate Ct., Silver Spring, MD 20905, USA; E-Mails: [email protected] (D.A.G.); [email protected] (J.K.K.) 2 Department of Biology, Simpson University, 2211 College View Dr., Redding, CA 96003, USA; E-Mail: [email protected] 3 Department of Psychiatry, University of Texas Southwestern Medical Center at Dallas, 5353 Harry Hine Blvd., Dallas, TX 75390, USA 4 CoMeD, Inc., 14 Redgate Ct., Silver Spring, MD 20905, USA; E-Mails: [email protected] (P.G.K.); [email protected] (L.K.S.) * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-301-989-0548; Fax: +1-301-989-1543. Received: 12 July 2014; in revised form: 7 August 2014 / Accepted: 26 August 2014 / Published: 5 September 2014 Abstract: A hypothesis testing case-control study evaluated concerns about the toxic effects of organic-mercury (Hg) exposure from thimerosal-containing (49.55% Hg by weight) vaccines on the risk of neurodevelopmental disorders (NDs). Automated medical records were examined to identify cases and controls enrolled from their date-of-birth (1991–2000) in the Vaccine Safety Datalink (VSD) project. -

20Mg Spironolactone I.P…..50Mg
For the use only of a Registered Medical Practitioner or Hospital or a Laboratory. This package insert is continually updated: Please read carefully before using a new pack Frusemide and Spironolactone Tablets Lasilactone® 50 COMPOSITION Each film coated tablet contains Frusemide I.P. …….. 20mg Spironolactone I.P…..50mg THERAPEUTIC INDICATIONS Lasilactone® contains a short-acting diuretic and a long-acting aldosterone antagonist. It is indicated in the treatment of resistant oedema where this is associated with secondary hyperaldosteronism; conditions include chronic congestive cardiac failure and hepatic cirrhosis. Treatment with Lasilactone® should be reserved for cases refractory to a diuretic alone at conventional doses. This fixed ratio combination should only be used if titration with the component drugs separately indicates that this product is appropriate. The use of Lasilactone® in the management of essential hypertension should be restricted to patients with demonstrated hyperaldosteronism. It is recommended that in these patients also, this combination should only be used if titration with the component drugs separately indicates that this product is appropriate. POSOLOGY AND METHOD OF ADMINISTRATION For oral administration. The dose must be the lowest that is sufficient to achieve the desired effect. Adults: 1-4 tablets daily. Children: The product is not suitable for use in children. Elderly: Frusemide and Spironolactone may both be excreted more slowly in the elderly. Tablets are best taken at breakfast and/or lunch with a generous amount of liquid (approx. 1 glass). An evening dose is not recommended, especially during initial treatment, because of the increased nocturnal output of urine to be expected in such cases. -

Medications That Are Safe During Pregnancy
Medications that Are Safe during Pregnancy Women who are between four and 12 weeks pregnant may safely take the following over-the-counter medications. Follow all directions on the container for adult dosage/use. ~r---------~ I Problem Over the Counter ICall Your Care Provider for: c __ ; Morning sickness Vitamin 86: take 50 mg/day to start; if not Persistent vomiting; weight loss or helpful, increase by 50 mg 2 to 4 times/day inability to tolerate fluids for 24 hours until you reach a total of 200 mg/day. Do not take more than 200 mg each day. I Increase fluids. i I Mild headaches / general Try comfort measures. Severe and/or persistent headaches I aches & pains Acetominophen (Tylenol) - ~ ~""~'" I Nasal congestion due to a IOcean Mist nasal spray I cold, sinusitis or allergies I I -, Women who are more than 12 weeks pregnant may safely take the following over-the-counter medications. Follow all directions on the container for adult dosage/use. I Problem lover the Counter 1Call Your Care Provider for: '" '''''Moo "0'''"0'''''''''''" , Nasal congestion due to a Sudafed, Afrin nasal spray, Ocean Mist cold, sinusitis or allergies nasal spray I I i Cough due to minor throat Robitussin (or other brand of Guaifenesin), Persistent cough i irritation Robitussin DM or non-alcohol cough syrup (not to exceed 1 ! week's use) i I Nasal congestion and coUgh Triaminic DM (or other brand of alcohol- free and antihistamine-free decongestant I and antitussive) I I I Sore throat Alcohol-free lozenges, such as Severe or persistent sore throat Chloraseptic -
Preventing Dehydration
State of New Jersey Department of Human Services Division of Developmental Disabilities DDDDDD PREVENTIONPREVENTION BULLETINBULLETIN Dehydration Dehydration is a loss of too much fluid from the body. The body needs water in order to maintain normal functioning. If your body loses too much fluid - more than you are getting from your food and liquids - your body loses electrolytes. Electrolytes include important nutrients like sodium and potassium which your body needs to work normally. A person can be at risk for dehydration in any season, not just the summer months. It is also important to know that elderly individuals are at heightened risk for dehydration because their bodies have a lower water content than younger people. Why people with Common Causes and a developmental Risk Factors for disability may be Dehydration: at a higher risk for dehydration. v Diarrhea v Vomiting v People with physical limitations may v Excessive sweating not be able to get something to drink on their own and will need the assistance of v Fever others. v Burns v People who cannot speak or whose v Diabetes when blood sugar is too high speech is hard to understand may have a v hard time telling their support staff that Increased urination (undiagnosed diabetes) they are thirsty. v Not drinking enough water, especially on warm and hot days v Some people may have difficulty swal- lowing their food or drinks and may v Not drinking enough during or after exercise refuse to eat or drink. This can make v Some medications (diuretics, blood pressure them more susceptible to becoming meds, certain psychotropic and anticonvul- dehydrated. -
The Effect of Dehydration, Hyperthermia, and Fatigue on Landing Error Scoring System Scores
ABSTRACT THE EFFECT OF DEHYDRATION, HYPERTHERMIA, AND FATIGUE ON LANDING ERROR SCORING SYSTEM SCORES Purpose: To examine the effects of exercise-induced dehydration, hyperthermia, and fatigue on Landing Error Scoring System (LESS) scores during a jump-landing task, and the effectiveness of a personalized hydration plan. Methods: Five recreationally active heat-acclimatized males 25.4 y (SD=5.7) completed two trials: with fluid replacement, (EXP) and without fluid (CON), in a counterbalanced, randomized, cross-over fashion. Exercise was terminated when gastrointestinal temperature (Tgi) = 39.5°C and fatigue ≥ 7/10, or 90 min of exercise. Percent dehydration was determined by body mass change from pre- exercise (PRE) and post-exercise (POST). Tgi, heart rate (HR), and perceived fatigue were measured PRE, during exercise, and POST. Three jump-landing tasks were filmed in the frontal and sagittal planes. An experienced grader evaluated jump-landing tasks using the LESS. Statistical Analysis: Repeated measures ANOVA assessed primary dependent and independent variables while a priori dependent t-tests evaluated pairwise comparisons. Results: No interaction, group, or time main effects were observed for LESS scores (p=0.437). POST dehydration (%) was greater in CON (M=2.59, SD=0.52) vs. EXP (M=0.92, SD=0.41; p<0.001), whereas hyperthermia (°C) (CON, M=39.29, SD=0.31, EXP, M=39.03, SD=0.61; p=0.425), and fatigue (CON, M=9, SD=1, EXP, M=9, SD=2; p=0.424) were similar. Conclusion: LESS scores were not affected by exercise-induced dehydration, hyperthermia, and fatigue, nor by a personal hydration plan. -

General Instructions for Infant and Child Care
Name _______________________________________________ Birth Date ____________________________________________ GENERAL INSTRUCTIONS FOR INFANT AND CHILD CARE GUIDELINES FOR HEALTH EVALUATION VISITS Richmond Pediatrics Pediatric & Adolescent Medicine . for over 50 years 357 N.W. Richmond Beach Road Shoreline, Washington 98177 (206) 546-2421 (206) 546-8436 – Fax www.Richmond-Pediatrics.com Age Immunization Date Given Immunizations >9 Years Old Birth Hepatitis B Immunization Date Given Hepatitis B MCV4 (Meningitis) #1 DtaP MCV4 (Meningitis) #2 IPV (Polio) 2 Months TdaP Hib (Meningitis) HPV #1 PCV13 (Pneumonia) Rotavirus HPV #2 DtaP HPV #3 IPV (Polio) 4 Months Hib (Meningitis) We also recommend a yearly influenza immunization. PCV13 (Pneumonia) Rotavirus Hepatitis B DtaP IPV (Polio) 6 Months Hib (Meningitis) PCV13 (Pneumonia) Rotavirus MMR VZV (Chickenpox) DtaP 12 -18 Hib (Meningitis) Months PCV13 (Pneumonia) Hepatitis A #1 Hepatitis A #2 18mos-4yrs PCV13 booster DtaP IPV 5 Years MMR VZV (Chickenpox) Influenza #1 6mos-5 yrs Influenza #2 TABLE OF CONTENTS Infant Care Page Breast Feeding ..............................................................6 Diarrhea .......................................................................20 Formula .........................................................................8 Dehydration .................................................................20 Feeding Schedule .........................................................9 Fever ...........................................................................22 -

Intervention Ideas for Infants, Toddlers, Children, and Youth Impacted by Opioids
TOPICAL ISSUE BRIEF Intervention IDEAs for Infants, Toddlers, Children, and Youth Impacted by Opioids Overview Prevalence The abuse of opioids—such as heroin and various prescription drugs commonly prescribed for pain (e.g., oxycodone, hydrocodone, and fentanyl)—has rapidly gained attention across the United States as a public health crisis. Youth may be exposed to opioids in a variety of ways, including but not limited to infants born to mothers who took opioids during pregnancy; children mistakenly consuming opioids (perhaps thinking they are candy); teenagers taking opioids from an illicit street supply; or, more commonly, teenagers being given opiates for free by a friend or relative.1,2 Even appropriate opioid use among adolescents and young adults to treat pain may slightly increase their risk of later opioid misuse.3 The Centers for Disease Control and Prevention (CDC) have identified opioid abuse as an epidemic, noting that opioids impact and affect all communities and age groups.4 Between 1997 and 2012, 13,052 children were hospitalized for poisonings caused by oxycodone, Percocet (a combination of acetaminophen and oxycodone), codeine, and other prescription opioids.5 Every 25 minutes, an infant is born suffering from opioid withdrawal, and an estimated 21,732 infants were born in 2012 with neonatal abstinence syndrome (NAS), a drug withdrawal syndrome.6 According to data from 2014, approximately 28,000 adolescents had used heroin within the past year, 16,000 were current heroin users, and 18,000 had a heroin use disorder.7 At the same time, relatively few data are available about the effects of opiates on the U.S. -

Child and Adolescent Needs and Strengths: Early Childhood
Child and Adolescent Needs and Strengths: Early Childhood CANS: EC Supplemental Guide A Support for the CANS (Early Childhood) Information Integration Tool for Young Children Ages Birth to Five SET is part of the System of Care Initiative, within the Allegheny County Department of Human Services, Office of Behavioral Health Stacey Cornett, Copyright 2007. Child and Adolescent Needs and Strengths: Early Childhood (CANS:EC) Section One: Child Strengths This section focuses on the attributes, traits, talents and skills of the child that can be useful in developing a strength-based treatment plan. Within a systems of care approach identifying strengths is considered an essential part of the process (Miles, P., Burns, E.J., Osher, T.W., Walker, J.S., 2006). A focus on strengths that both the child and the family have to offer allows for a climate of hope and optimism and has been proven to engage families at a higher level. Strength-based assessment has been defined as, “the measurement of those emotional and behavioral skills, competencies, and characteristics that create a sense of personal accomplishment; contribute to satisfying relationships with family members, peers, and adults; enhance one’s ability to deal with adversity and stress; and promote one’s personal, social, and academic development” (Epstein & Sharma, 1998, p.3). The benefits of a strength- based assessment include involving parents and children in a service planning experience that builds on what a child and family are doing well, facilitates positive expectations for the child, and empowers family members to take responsibility for the decisions that will affect their child (Johnson & Friedman, 1991; Saleebey, 1992). -
The Child with Failure to Thrive
The Child with Failure to Thrive Bonnie Proulx, MSN, APRN, PNP Pediatric Gastroenterology Children’s Hospital at Dartmouth Manchester, NH DISCLOSURES None of the planners or presenters of this session have disclosed any conflict or commercial interest The Child with Failure to Thrive OBJECTIVES: 1. Review assessment and appropriate diagnostic testing for children who fail meet expected growth 2. Discuss various causes of failure to thrive. 3. Identify appropriate referrals for children with failure to thrive. Definition • Inadequate physical growth diagnosed by observation of growth over time on a standard growth chart Definition • More than 2 standard deviations below mean for age • Downward trend in growth crossing 2 major percentiles in a short time • Comparison of height and weight • Not a diagnosis but a finding Pitfalls • Some children are just tiny • Familial short stature children may cross percentiles to follow genetic predisposition • Normal small children may be diagnosed later given already tiny Frequency • Affects 5-10% of children under 5 in developing countries • Peak incidence between 9 and 24 months of age • Uncommon after the age of 5 What is normal growth • Birth to 6 months, a baby may grow 1/2 to 1 inch (about 1.5 to 2.5 centimeters) a month • 6 to 12 months, a baby may grow 3/8 inch (about 1 centimeter) a month • 2nd year of life 4-6 inches • 3rd year 3-4 inches • Annual growth until pre-puberty 2-3 inches per year Normal weight gain • Birth to 6 months-gain 5 to 7 ounces a week. • 6 to 12 months -gain 3 to 5 ounces (about 85 to 140 grams) a week. -

Water Requirements, Impinging Factors, and Recommended Intakes
Rolling Revision of the WHO Guidelines for Drinking-Water Quality Draft for review and comments (Not for citation) Water Requirements, Impinging Factors, and Recommended Intakes By A. Grandjean World Health Organization August 2004 2 Introduction Water is an essential nutrient for all known forms of life and the mechanisms by which fluid and electrolyte homeostasis is maintained in humans are well understood. Until recently, our exploration of water requirements has been guided by the need to avoid adverse events such as dehydration. Our increasing appreciation for the impinging factors that must be considered when attempting to establish recommendations of water intake presents us with new and challenging questions. This paper, for the most part, will concentrate on water requirements, adverse consequences of inadequate intakes, and factors that affect fluid requirements. Other pertinent issues will also be mentioned. For example, what are the common sources of dietary water and how do they vary by culture, geography, personal preference, and availability, and is there an optimal fluid intake beyond that needed for water balance? Adverse consequences of inadequate water intake, requirements for water, and factors that affect requirements Adverse Consequences Dehydration is the adverse consequence of inadequate water intake. The symptoms of acute dehydration vary with the degree of water deficit (1). For example, fluid loss at 1% of body weight impairs thermoregulation and, thirst occurs at this level of dehydration. Thirst increases at 2%, with dry mouth appearing at approximately 3%. Vague discomfort and loss of appetite appear at 2%. The threshold for impaired exercise thermoregulation is 1% dehydration, and at 4% decrements of 20-30% is seen in work capacity. -
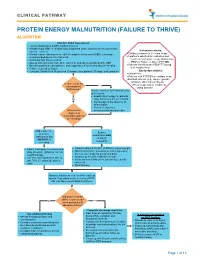
Protein Energy Malnutrition (Failure to Thrive) Algorithm
CLINICAL PATHWAY PROTEIN ENERGY MALNUTRITION (FAILURE TO THRIVE) ALGORITHM Conduct Initial Assessment • History and physical (H&P), nutrition focused • Weight height, BMI, % of ideal body weight and exam: assess severity (symmetric edema = severe) Inclusion criteria: • • Consider basic labs based on H&P; A complete blood count (CBC) is strongly Children newborn to 21 years of age • recommended due to risk of anemia Inpatients admitted for evaluation and • Additional labs based on H&P treatment of Protein Energy Malnutrition • Assess micronutrients: iron, zinc, vitamin D, and others as indicated by H&P (PEM) or Failure to thrive (FTT) OR • • Baseline potassium, phosphorus, and magnesium if concerned about re-feeding Patients identified with PEM/FTT during • Calorie count up to 3 days their hospital stay. • Consults: Social Work, Registered Dietician, Occupational Therapy, and Lactation Exclusion criteria: • Outpatients • Patients with FTT/PEM secondary to an identified concern (e.g., cancer, genetic condition, other chronic illness). Is there a risk for •Pts w/ suspected or confirmed micronutrient Yes eating disorder deficiencies? Initiate treatment for micronutrients deficiencies: • Empiric zinc therapy for patients No older than 6 months for 1 month • Iron therapy in the absence of inflammation • Vitamin D and other What are the micronutrients based on labs degrees of malnutrition and risk of refeeding? Mild, moderate, Severe or severe malnutrition AND malnutrition but at risk of NO RISK of refeeding refeeding • • Initiate feeding per recommended Initiate feeding at 30-50% of RDA for current weight • daily allowance (RDA) for current Monitor potassium, phosphorus, and magnesium weight and age once to twice a day for a total of 4 days • • Use PO route if patient is able to Advance by 10-20% if labs are normal • take 70% of estimated calories If labs abnormal hold off on advancing feed until orally corrected • Start thiamine Advance calories to meet level for catch up growth.