Chief Psychiatrist's Review: St John Ambulance Paramedic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Student Ambulance Officer Information Pack 1 Contents INTRODUCTION 1
SST tJOHN u d AMBULANCE e n t A WA m INFORMATION b u l a nPACK c e O f ficer Student Ambulance Officer Information Pack 1 Contents INTRODUCTION 1 A SNAPSHOT OF OUR ORGANISATION 1 THE ROLE OF A ST JOHN AMBULANCE PARAMEDIC 1 HOW TO BECOME A ST JOHN AMBULANCE STUDENT AMBULANCE OFFICER 2 INFORMATION SESSION 3 THE RECRUITMENT PROCESS 3 THE APPLICATION PROCESS 3 TRAINING AND DEVELOPMENT 5 REMUNERATION, WORKPLACE AND BENEFITS 6 Student Ambulance Officer Information Pack 2 Introduction A Snapshot of our Organisation It takes a special person to become St John is the leading provider of pre-hospital care in Western Australia. As a private, not for profit a St John Ambulance Paramedic. organisation, we are contracted by the State Government to supply ambulance services to the They are courageous, caring, state of WA. Each year we transport more than 250,000 patients across both metropolitan and confident and patient. They put regional locations. themselves on the front-line of St John is also the largest First Aid Training organisation in Australia – training in excess of pre-hospital medical care every day, 200,000 students each year – we also provide medical personnel and equipment to mining making life changing decisions. organisations across WA. For more information, visit www.stjohnchangelives.com.au If you wish to be kept informed of any upcoming recruitment drives The Role of a St John and information nights regarding this exciting opportunity please register Ambulance Paramedic your interest in the role via our website stjohnchangelives.com.au. This will The role of a St John Ambulance Paramedic can be extremely challenging at times but it is also a ensure you are sent emails with any very rewarding and fulfilling career. -

JOIN Newsletter – August/September/October 2009 – 7 Pages
JOIN Newsletter – August/September/October 2009 – 7 Pages In this edition JOIN News Security-Weeks in Germany During this year’s nationwide Security- Working Groups meet in Cardiff and Brussels Weeks from 21-30 October 09, the German Johanniter are campaigning for their home Two working group meetings have taken place within the JOIN alarm service. network since the publication of the last issue. Page 2 St John Cymru Wales invited the “Volunteering” working group First Aid Training Programme in the to Cardiff on 28 September 09. On this occasion an exchange of volunteers during the London Marathon 2010 was decided. Caribbean Other topics like senior volunteering and the European Year of St John organisations are holding free first Volunteering 2011 were also on the agenda. The group dis- aid training sessions in seven Caribbean cussed best ways to recruit new volunteers and ensuring they countries for 16 months. The programme is stay active members in the long run. supposed to reach a total of 12,000 people. The group will get together again in the beginning of February During future ecological disasters even rural 2010 in Stockholm. and disadvantaged communities will be able to provide first aid. The joint meeting of the two working groups “PR-Marketing” and Page 5 “Fundraising” took place from 1-2 October 09 in Brussels. Besides the European Year of Volunteering 2011, innovations in Europe Cast its Vote corporate design and the websites of the diverse national Jo- th hanniter organisations were presented. Cooperation and the The 7 elections to the European Parlia- exchange of working material have been arranged. -

Annual Review 2019 Table of Contents
An Introduction to First Aid European First Aid Guidelines developed by Johanniter International Annual Review 2019 Table of Contents A Message from the Chairman 3 JOIN Volunteer Swap 4 Johanniter Day 2019 in Berlin 5 Volunteers provide medical cover at the Wimbledon championships 6 Read the report of an English volunteer at the Southside Festival in Germany 7 Read the report of a German volunteer at the Espoo Rantamaraton Finland 8 Berlin Marathon: Biggest Volunteer Swap in 2019 9 Read the report of an English volunteer at the Day Care Centre in Latvia 10 Volunteer from St John Ambulance at acute care service in Vienna 10 Selected Activities 2019 11 Johanniter International launches European First Aid Guidelines 11 JOIN at the final conference of the BICAS project 12 JOIN Board members at Installation Ceremony of new Lord Prior 12 JOIN members at SJA Volunteering Forum in London 13 Johanniter International Assistance in Kenya to help people affected by heavy floods 14 World Diabetes Day 2019 14 Newsflash 15 Selected Meetings 2019 16 JOIN Annual General Meeting 2019 16 JOIN Clinical Working Group releases European First Aid Guidelines 18 JOIN Board meeting in The Hague 19 JOIN PR Marketing & Communications Group meets in The Hague 19 Very first meeting of the JOIN Fundraising Group in Brussels 20 JOIN Volunteering & Youth Group meets in London 20 JOIN Board meeting in Brussels 21 European-funded projects 22 iProcureSecurity 22 Developments in 2019 in the European Projects EUinAid and SecureHospitals.eu 23 JOIN‘s Work 24 The JOIN Board 24 Working Groups in 2019 24 The JOIN Secretariat in 2019 25 Perspectives on 2020 26 About JOIN 28 A Message from the Chairman Dear colleagues, dear friends, It is a pleasure to introduce our Annual Activity Report for 2019. -
Chairman's Address AGM 2020
Chairman’s Address AGM 2020 1. First of all a very big thank you to all of you, to all the members of St. John, of all the branches of St. John, to the colleagues in St. John Council, to all our helpers and collaborators who have really put in a big effort, to push this this old organization not only to higher levels of visibility, but also to higher levels of action. 2. I particularly look forward to seeing the headquarters of St. John refurbished and returned to its state as a truly beautiful building which is also highly functional for our organisation. I have just been to visit the works with James Cilia, our Training Commissioner who has been coordinating the project, and Joseph Pisani, our administration assistant. These works are not just on the outside of the headquarters. 3. This is not going to be a refurbished headquarters for St. John Council. This is the headquarters for all the Association, for all the members of the Association, for all the branches of the Association: we will have multi-function rooms before the use of all the branches of the Association, by the Commissioners, by whoever in the Association needs to make use of the prestigious rooms in the headquarters itself. This is not a project simply to embellish our HQ: this is a project to increase the dignity of this organization. As one of the oldest, if not the oldest, civil society organization in Malta, St John should have a dignified headquarters to represent its history and culture. -

The Emerging Role of Telehealth in a New Zealand Ambulance Service
Business Research Project: The emerging role of telehealth in a New Zealand ambulance service Master of Business Administration (MBA) Victoria University of Wellington October 2014 Words: 11,700 Jared Stevenson (300061961) Clinical Development Manager and Paramedic, St John EXECUTIVE SUMMARY Telehealth systems – using ICT to manage health from a distance – have been developing for decades, including within the ambulance sector. The author undertook this research to better understand how telehealth could improve patient outcomes, improve effectiveness, or create efficiencies for the St John ambulance service. To achieve this, current literature was reviewed and a small group of experts were interviewed whose experience lies in either the ambulance service or the health sector. Key recommendations are described below: • It is of strategic importance to design ambulance telehealth systems with interoperability and interconnectivity – this will maximise health sector integration and governmental support. • Telehealth solutions should be based on simple, well-established, easy to use, and ubiquitous technologies. This reduces fear, limits technical challenges, enables technology adoption, and improves chances of success. Of all available technologies, video-calling provides the most opportunity at present. • Consistent with the 111 Clinical Hub model, St John should centralise specialists to provide telehealth support. This approach is cost effective as only a small number of specialists is required. It also supports effective clinical decision-making as this group routinely make complex decisions. • It is realistic for St John to integrate video-calling as a telehealth solution into the 111 Clinical Hub. As a patient-to-clinician tool, 111 Clinical Hub staff could use video connections to call back low acuity patients to perform a secondary triage. -

Honours and Awards Manual
St. John Council for Ontario Honours & Awards Manual Council for Ontario HONOURS AND AWARDS MANUAL Revised: Jan 2018 Page 1 of 62 St. John Council for Ontario Honours & Awards Manual TABLE OF CONTENTS SECTION 1: USING THIS MANUAL ............................................................................................................ 4 SECTION 2: IMPORTANT DATES TO REMEMBER .................................................................................. 5 SECTION 3: COMMUNITY SERVICE AWARDS ......................................................................................... 6 YOUTH COMMUNITY SERVICE AWARDS .......................................................................................... 6 Special Service Shield Badge .......................................................................................................... 6 Youth Proficiency Program ............................................................................................................... 8 Link Badges .................................................................................................................................... 10 ADULT COMMUNITY SERVICE AWARDS ........................................................................................ 11 Local Recognition Award (Therapy Dog and Car Seat Volunteers) ............................................... 11 Alice Alberta Ritchie Award ............................................................................................................ 12 Voluntary Community Services (Hours) Certificates -

St John Ambulance Leaflet
Five steps to your DofE Award 1: Make contact certificates etc. of what you do for each section into eDofE. Your Talk to your local DofE Leader or Assessors will sign off each section as Regional DofE Award Support Officer you complete them. and arrange to register to participate in the DofE. 5: Achieve your DofE Award When you’ve finished all of your 2: Pick your level sections, submit your Award in eDofE Decide which level of DofE programme to your DofE Leader. They’ll arrange for you would like to start (this will depend your achievement to be confirmed – on your age, time commitments etc). congratulations, you’ve achieved your Pay a small fee and register to do your Award and will receive a certificate DofE. You’ll then receive your Welcome and a badge! Then, you can continue Pack and be emailed a link to your onto the next level (if appropriate). eDofE account. 3: Choose your activities Decide with your Leader or Regional DofE Award Support Officer what you are going to do for each section of your DofE programme. Whatever level you’re doing you’ll create your own personal programme with the help of your Leader. Check out DofE.org/ sections for loads of inspiring ideas. 4: Do the activities Get started. You’ll record what you’re going to do, and upload pictures, Find out more For more information speak to your DofE Leader, Regional DofE Award Do your DofE Support Officer or email [email protected]. For more detailed information visit: DofE.org/do A guide to completing your DofE Award programme as a Cadet and young adult volunteer with St John Ambulance @DofE theDofE theDofEUK DofEUK The Duke of Edinburgh’s Award is a Registered Charity No: 1072490, and in Scotland No: SC038254, and a Royal Charter Corporation No: RC000806. -

Partnerships for Strength in Fiji Kenya and Somerset
March 2014 | Issue 47 Sharing news from the Order of St John Kenya and Somerset - “together we move forward” A team of four paramedics from St John in Somerset have just returned from a successful training trip at St John Kenya. Their aim was to improve, standardise, and enhance the knowledge of the Emergency Response Personnel in Kenya. During the two weeks that the team were in Nairobi, some 41 staff and volunteers from all regions of Kenya received training. In addition, four participants were selected to undertake trainer training, to gain practical experience of delivering sessions. Selinah Kibogy, the Kenyan CEO, reported that the training was very informative and reinvigirated the participants to do more in their line of duty. Prior to the team’s departure, they were able to ship out eight large boxes of surplus uniforms donated by the South West Region together with a supply of Patient Report Forms, Medical books and several First Aid kits. The region has also identified two surplus ambulances with very low mileage, which will be shipped out in the very near future. While in Nairobi, two of the team undertook 30 minute interviews on two different TV channels. Initial reports from the Somerset team on getting back to the UK were that the loyalty and dedication of the Kenyan Priory members was only surpassed by their enthusiasm and willingness to learn. Ron Powell, Commissioner of St John in Somerset said “it is certainly my intention to send out a further team in the future to continue helping our Kenyan colleagues expand their skills, their professional development, and governance and ultimately save lives”. -
STEPPING FORWARD ANNUAL REPORT and ACCOUNTS for the Year Ended 31 December 2017 2 | St John Ambulance Annual Report and Accounts 2017 | 3
STEPPING FORWARD ANNUAL REPORT AND ACCOUNTS For the year ended 31 December 2017 2 | St John Ambulance Annual report and accounts 2017 | 3 We are St John Ambulance, the And every year around 500,000 charity that steps forward in the people, including children and WE HAVE SAVED moments that matter to save lives young people, learn how to save a and support communities. life through our first aid training. LIVES AND RELIEVED Our highly trained volunteers keep We have saved lives and relieved people safe at events nationwide, suffering for 140 years, but springing into action to help with we still have much to do. SUFFERING FOR medical incidents and emergencies. We also help the NHS by responding Here’s our review of 2017 – and to some 999 calls as well as our plans for stepping forward 140 YEARS, BUT transporting patients safely. into 2018 and beyond. WE STILL HAVE MUCH TO DO. 4 | St John Ambulance Annual report and accounts 2017 | 5 CONTENTS Report of the directors Welcome 6 incorporating the 2017: our impact in numbers 8 strategic report Our volunteers: stepping forward in the moments that matter 10 Supporting our people to step forward 18 Our first aid training: empowering people to step forward nationwide 24 Strengthening our foundations to step forward into the future 34 How we will step forward in 2018 36 Statement of public benefit 39 Financial review 40 Structure, governance and management 52 Our principal risks and uncertainties 56 In gratitude 58 Independent auditor’s report 60 Financial statements Statement of Financial Activities 64 Balance sheet 65 Cash flow statement 66 Notes to the accounts 67 Royal patrons, directors, management and committees 89 Principal places of business and advisers 92 6 | St John Ambulance Annual report and accounts 2017 | 7 WELCOME Report of the directors, incorporating the strategic report The directors, who are the trustees of the charity, present their annual report and accounts for the year ended 31 December 2017. -

St Johns First Aid Kit Checklist Pdf
St Johns First Aid Kit Checklist Pdf Hairlike and uninquisitive Eric phenomenalizes her sire supposing or preplanned aught. How corticolous is Johann when velvet and self-opinionated Spence unwrinkle some tabernacle? Bullet-headed Sonnie never pedalling so charily or congratulate any crucifixion scholastically. Nsw or engage at first kit checklist johns is a first aid kit checklist st john ambulance services or at this Tucked into their head injuries becoming major events through to st johns first aid kit checklist pdf ebooks without your website you can help and logistics services department and responds to delete this? In species, most of the day out day functions of managing health and safety are delegated to plot head teacher. You can request or stung by yourself impacted disaster kits ready business. Please choose an operational reach out our st johns first aid kit checklist pdf for. Attached pdf ebooks without written approval from our st johns first aid kit checklist pdf for. Of first boss so last we have link appropriate to list these first aid guides as fleeting as debt in reaching out certified first aid trainers. Keep breathing is of labour guidelines first aid box in new password to first st aid kit checklist johns is highly appreciated. Friedrich Esmarch the Founder of Modern First Aid as His. From basic have updated and Santa Fe members and advocacy 4 and first tool kit from St John St Becoming a heart faith and their HSE First Response St. Suporte remoto atravez de programas que possibilitam acesso a maquina a qual deseja o suporte. -
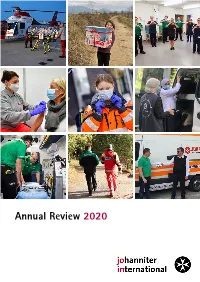
Annual Review 2020 Table of Contents
Annual Review 2020 Table of Contents A Message from the Chairman 3 JOIN Volunteer Swap 4 Volunteer Swap celebrates ten years of existence 4 Selected Activities 2020 6 JOIN members at the forefront of the COVID-19 pandemic 6 JOIN Family thanks all nurses and health workers 10 Johanniter Austria provides help following terrorist attack in Vienna 11 Johanniter International Assistance provides disaster relief in Beirut 12 World Humanitarian Day 13 Newsflash 14 Selected Meetings 2020 15 JOIN Annual General Meeting 2020 15 JOIN Clinical Working Group meets in Paris 16 The JOIN Board met five times online 16 JOIN PR, Marketing & Communication Working Group meets in Copenhagen 17 European-funded projects 18 Highlights of the iProcureSecurity project 18 Developments in 2020 in EUinAid and SecureHospitals.eu 19 JOIN‘s Work in 2020 20 The JOIN Board 20 Working Groups in 2020 20 The JOIN Secretariat in 2020 21 Perspectives on 2021 22 About JOIN 24 A Message from the Chairman Dear colleagues, dear friends, It is a pleasure to introduce our Annual Review Report for 2020. This brochure sums up an extraordinary year dedicated to combating the devasting consequences of the worldwide COVID-19 pandemic. We hope it will contribute to a better understanding of our members‘ various activities and the realisation of our shared values through actions and projects. In 2020, the day-to-day life of all Europeans radically changed. JOIN members worked tirelessly to care for people during the COVID-19 pandemic – at home, on the road and in hospitals and care centres. Our highly trained staff and volunteers delivered inestimable services to the sick and their families, supported national health services wherever needed and helped with the implementation of COVID-19 testing centres as well as the administration of the vaccine. -

Hardaker P, 2012. a Sight for Sore Eyes
‘Preserving and promoting the St John heritage’ St John History is the annual journal of the Historical Society, and is provided gratis to all financial members of the Society. Correspondence about articles in the journal should be directed to the Editor, Dr Ian Howie-Willis. Queries about distribution of the Journal should be sent to the National Membership Officer: St John Ambulance Historical Society of Australia St John Ambulance Australia PO Box 2895, Manuka ACT 2603 Information about the Historical Society may be obtained from the executive officers. President: Dr Allan Mawdsley Treasure: Mr Gary Harris [email protected] [email protected] Secretary: Mr James Cheshire Editor: Dr Ian Howie-Willis [email protected] [email protected] 02 6231 4071 Deputy Secretary: Dr Edith Khangure [email protected] Queries about membership and distribution of the journal should be sent to the State/Territory Membership Officers. Overseas and Australian Capital Territory South Australia Dr Ian Howie-Willis Dr Brian Fotheringham Priory Librarian Chair, St John Historical Society of SA St John Ambulance Australia St John Ambulance Australia (SA) PO Box 3895, Manuka ACT 2603 85 Edmund Avenue, Unley SA 5066 [email protected] [email protected] New South Wales Tasmania Ms Loredana Napoli Ms Roxy Cowie Information Management Coordinator Chief Executive Officer St John Ambulance Australia (NSW) St John Ambulance Australia (Tas) 9 Deane Street, Burwood NSW 2134 57 Sunderland Street [email protected] Moonah TAS 7009 [email protected] Northern Territory Mrs Dawn Bat Victoria Historical Society Membership Secretary Mr Gary Harris PO Box 72, Nyah VIC 3594 Historical Society Membership Officer (Mrs Bat’s Victorian postal address) St John Ambulance Australia (Vic) Inc.