Synthetic Cannabinoids in Oral Fluid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cannabinoids in the Pathophysiology of Skin Inflammation
molecules Review Cannabinoids in the Pathophysiology of Skin Inflammation Cristian Scheau 1 , Ioana Anca Badarau 1, Livia-Gratiela Mihai 1, Andreea-Elena Scheau 2, Daniel Octavian Costache 3, Carolina Constantin 4,5, Daniela Calina 6 , Constantin Caruntu 1,7,*, Raluca Simona Costache 8,* and Ana Caruntu 9,10 1 Department of Physiology, “Carol Davila” University of Medicine and Pharmacy, 050474 Bucharest, Romania; [email protected] (C.S.); [email protected] (I.A.B.); [email protected] (L.-G.M.) 2 Department of Radiology and Medical Imaging, Fundeni Clinical Institute, 022328 Bucharest, Romania; [email protected] 3 Department of Dermatology, “Carol Davila” Central Military Emergency Hospital, 010825 Bucharest, Romania; [email protected] 4 Immunology Department, ”Victor Babes” National Institute of Pathology, 050096 Bucharest, Romania; [email protected] 5 Department of Pathology, Colentina University Hospital, 020125 Bucharest, Romania 6 Department of Clinical Pharmacy, University of Medicine and Pharmacy of Craiova, 200349 Craiova, Romania; [email protected] 7 Department of Dermatology, “Prof. N. Paulescu” National Institute of Diabetes, Nutrition and Metabolic Diseases, 011233 Bucharest, Romania 8 Gastroenterology and Internal Medicine Clinic, Carol Davila University Central Emergency Military Hospital, Carol Davila University of Medicine and Pharmacy, 050474 Bucharest, Romania 9 Department of Oral and Maxillofacial Surgery, “Carol Davila” Central Military Emergency Hospital, 010825 Bucharest, Romania; [email protected] 10 Faculty of Medicine, “Titu Maiorescu” University, 031593 Bucharest, Romania * Correspondence: [email protected] (C.C.); [email protected] (R.S.C.); Tel.: +40-745-086-978 (C.C.) Academic Editor: Eric J. Downer Received: 30 December 2019; Accepted: 2 February 2020; Published: 4 February 2020 Abstract: Cannabinoids are increasingly-used substances in the treatment of chronic pain, some neuropsychiatric disorders and more recently, skin disorders with an inflammatory component. -

) (51) International Patent Classification: Columbia V5G 1G3
) ( (51) International Patent Classification: Columbia V5G 1G3 (CA). PANDEY, Nihar R.; 10209 A 61K 31/4525 (2006.01) C07C 39/23 (2006.01) 128A St, Surrey, British Columbia V3T 3E7 (CA). A61K 31/05 (2006.01) C07D 405/06 (2006.01) (74) Agent: ZIESCHE, Sonia et al.; Gowling WLG (Canada) A61P25/22 (2006.01) LLP, 2300 - 550 Burrard Street, Vancouver, British Colum¬ (21) International Application Number: bia V6C 2B5 (CA). PCT/CA2020/050165 (81) Designated States (unless otherwise indicated, for every (22) International Filing Date: kind of national protection av ailable) . AE, AG, AL, AM, 07 February 2020 (07.02.2020) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, (25) Filing Language: English DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, (26) Publication Language: English HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (30) Priority Data: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, 16/270,389 07 February 2019 (07.02.2019) US OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (63) Related by continuation (CON) or continuation-in-part SC, SD, SE, SG, SK, SL, ST, SV, SY, TH, TJ, TM, TN, TR, (CIP) to earlier application: TT, TZ, UA, UG, US, UZ, VC, VN, WS, ZA, ZM, ZW. US 16/270,389 (CON) (84) Designated States (unless otherwise indicated, for every Filed on 07 Februaiy 2019 (07.02.2019) kind of regional protection available) . -

NIDA's Drug Facts on Synthetic Cannabinoids (K2/Spice)
Synthetic Cannabinoids (K2/Spice) Revised February 2018 What are synthetic cannabinoids? Synthetic cannabinoids are human-made mind-altering chemicals that are either sprayed on dried, shredded plant material so they can be smoked or sold as liquids to be vaporized and inhaled in e-cigarettes and other devices. These products are also known as herbal or liquid incense. These chemicals are called cannabinoids because they are similar to chemicals found in the marijuana plant. Because of this similarity, synthetic cannabinoids are sometimes misleadingly called "synthetic marijuana" (or "fake weed"), and they are often marketed as safe, legal alternatives to that drug. In fact, they are not safe and may affect the brain much more powerfully than marijuana; their actual effects can be unpredictable and, in some cases, more dangerous or even life-threatening. Synthetic cannabinoids are part of a group of drugs called new psychoactive substances (NPS). NPS are unregulated mind-altering substances that have become newly available on the market and are intended to produce the same effects as illegal drugs. Some of these substances may have been around for years but have reentered the market in altered chemical forms, or due to renewed popularity. False Advertising Synthetic cannabinoid products are often labeled "not for human consumption." Labels also often claim that they contain "natural" material taken from a variety of plants. However, the only parts of these products that are natural are the dried plant materials. Chemical tests show that the active, mind-altering ingredients are cannabinoid compounds made in laboratories. Synthetic Cannabinoids • February 2018 • Page 1 Manufacturers sell these products in colorful foil packages and plastic bottles to attract consumers. -

Frequently Asked Questions About Synthetic Drugs
FREQUENTLY ASKED QUESTIONS ABOUT SYNTHETIC DRUGS WHAT ARE SYNTHETIC DRUGS? WHAT DOES THE PACKAGING OF SYNTHETIC CANNABINOIDS LOOK LIKE? A SYNTHETIC DRUG, ALSO REFERRED TO AS A Many of the products are sold in colorful packets with names DESIGNER DRUG, IS A CHEMICAL INTENDED TO that appeal to adolescents and young adults. Manufacturers IMITATE THE PROPERTIES AND EFFECTS OF A label the packages as “not for human consumption” and KNOWN HALLUCINOGEN OR NARCOTIC AND market the products as incense or potpourri to mask the MAY HAVE UNKNOWN SIDE EFFECTS OR CAUSE intended purpose and to avoid regulatory oversight of AN ADVERSE REACTION. THESE DRUGS ARE the manufacturing process. You can view examples of the packaging on page 3. CREATED IN ORDER TO EVADE RESTRICTIONS AGAINST ILLEGAL SUBSTANCES. ARE SYNTHETIC CANNABINOIDS ARE SYNTHETIC DRUGS LEGAL IN TEXAS? DANGEROUS? No. Under state law, it is a crime to manufacture, deliver or Synthetic cannabinoids possess a synthetic drug. are illegal, dangerous, highly addictive and WHAT ARE SYNTHETIC CANNABINOIDS? potentially deadly. One Synthetic cannabinoids are commonly referred to as K2, of the original chemists Kush, Spice, synthetic marijuana and fake weed. They are who designed synthetic a mix of plant matter sprayed with chemicals in sometimes cannabis for research purposes, John Huffman, Ph.D., likened dangerously high proportions, falsely marketed as “legal recreational use of synthetic drugs to playing Russian highs” and smoked like marijuana. roulette. The contents and effects of synthetic cannabinoids WHERE ARE SYNTHETIC CANNABINOIDS SOLD? are unpredictable due to a constantly changing variety of Synthetic cannabinoids are relatively inexpensive and sold chemicals used in manufacturing processes devoid of quality in convenience stores, smoke shops, novelty stores, on the controls and government regulatory oversight. -
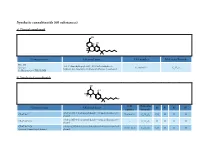
Synthetic Cannabinoids (60 Substances) A) Classical Cannabinoid
Synthetic cannabinoids (60 substances) a) Classical cannabinoid OH H OH H O Common name Chemical name CAS number Molecular Formula HU-210 3-(1,1’-dimethylheptyl)-6aR,7,10,10aR-tetrahydro-1- Synonym: 112830-95-2 C H O hydroxy-6,6-dimethyl-6H-dibenzo[b,d]pyran-9-methanol 25 38 3 11-Hydroxy-Δ-8-THC-DMH b) Nonclassical cannabinoids OH OH R2 R3 R4 R1 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyloctan- 2- yl) CP-47,497 70434-82-1 C H O CH H H H phenol 21 34 2 3 rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylheptan- 2- yl) CP-47,497-C6 - C H O H H H H phenol 20 32 2 CP-47,497-C8 rel-2- [(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylnonan- 2- yl) 70434-92-3 C H O C H H H H Synonym: Cannabicyclohexanol phenol 22 36 2 2 5 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyldecan- 2- yl) CP-47,497-C9 - C H O C H H H H phenol 23 38 2 3 7 rel-2- ((1 R,2 R,5 R)-5- hydroxy- 2- (3- hydroxypropyl)cyclohexyl)- 3-hydroxy CP-55,940 83003-12-7 C H O CH H H 5-(2- methyloctan- 2- yl)phenol 24 40 3 3 propyl rel-2- [(1 S,3 R)-3- hydroxy-5,5-dimethylcyclohexyl]- 5- (2- Dimethyl CP-47,497-C8 - C H O C H CH CH H methylnonan-2- yl)phenol 24 40 2 2 5 3 3 c) Aminoalkylindoles i) Naphthoylindoles 1' R R3' R2' O N CAS Molecular Common name Chemical name R1’ R2’ R3’ number Formula [1-[(1- methyl- 2- piperidinyl)methyl]- 1 H-indol- 3- yl]- 1- 1-methyl-2- AM-1220 137642-54-7 C H N O H H naphthalenyl-methanone 26 26 2 piperidinyl -

Cannabis, the Endocannabinoid System and Immunity—The Journey from the Bedside to the Bench and Back
International Journal of Molecular Sciences Review Cannabis, the Endocannabinoid System and Immunity—The Journey from the Bedside to the Bench and Back Osnat Almogi-Hazan * and Reuven Or Laboratory of Immunotherapy and Bone Marrow Transplantation, Hadassah Medical Center, The Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem 91120, Israel; [email protected] * Correspondence: [email protected] Received: 21 May 2020; Accepted: 19 June 2020; Published: 23 June 2020 Abstract: The Cannabis plant contains numerous components, including cannabinoids and other active molecules. The phyto-cannabinoid activity is mediated by the endocannabinoid system. Cannabinoids affect the nervous system and play significant roles in the regulation of the immune system. While Cannabis is not yet registered as a drug, the potential of cannabinoid-based medicines for the treatment of various conditions has led many countries to authorize their clinical use. However, the data from basic and medical research dedicated to medical Cannabis is currently limited. A variety of pathological conditions involve dysregulation of the immune system. For example, in cancer, immune surveillance and cancer immuno-editing result in immune tolerance. On the other hand, in autoimmune diseases increased immune activity causes tissue damage. Immuno-modulating therapies can regulate the immune system and therefore the immune-regulatory properties of cannabinoids, suggest their use in the therapy of immune related disorders. In this contemporary review, we discuss the roles of the endocannabinoid system in immunity and explore the emerging data about the effects of cannabinoids on the immune response in different pathologies. In addition, we discuss the complexities of using cannabinoid-based treatments in each of these conditions. -
Marinol Cannabidiol C21H30O2 Trade Name
Cannabinoids are a group of terpenophenolic compounds secreted by Cannabis flowers that provide relief from a wide array of symptoms including, pain, nausea, and inflammation. They operate by imitating the body’s natural endocannabinoids, which activate to maintain internal stability and overall health. When consumed, cannabinoids bind to receptor sites throughout the brain (CB1 receptors) and body (CB2 receptors). Different cannabinoids have different effects based on their binding affinity for each receptor. By targeting specific cannabinoids at these receptors, different types of relief can be achieved. Presently, there are at least 113 different cannabinoids isolated from Cannabis—each exhibiting varied effects. THC Tetrahydrocannabinol C21H30O2 Trade name: Marinol Legal Status: US – Schedule I, Schedule II (as Cesamet), Schedule III (as Marinol) OH CA – Schedule II UK – Class B AU – S8 (controlled) H Psychoactive Tetrahydrocannabinol (THC) is typically the most abundant cannabinoid present in cannabis products on the market today. THC has very high psychoactive characteristics and is associated with the ‘high’ and euphoria experienced when using cannabis products. When smoked or ingested, THC binds to cannabinoid receptors throughout the body and affects memory, O coordination, concentration, pleasure, and time perception. H Medicinal Benefits Analgesic • Anti-nauseant • Appetite Stimulant Reduces Glaucoma Symptoms Sleep Aid • Reduces Anxiety and PTSD Symptoms CBD Cannabidiol C21H30O2 Trade name: Epidiolex OH Legal Status: US – Schedule I CA – Schedule II UK – POM (Perscription only) H AU – S4 (Perscription only) non-psychoactive Cannabidiol (CBD) is a major phytocannabinoid and accounts for up to 40% of the plant’s extract. Due to its lack of psychoactivity and HO non-interference with motor and psychological functions, it is a leading candidate for a wide variety of medical applications. -

Recent Developments in Cannabis Chemistry
Recent Developments in Cannabis Chemistry BY ALEXANDER T. SHULGIN, Ph.D. The marijuana plant Cannabis sativa contains a bewildering Introduction array of organic chemicals. As is true with other botanic species, there are representatives of almost all chemical classes present, including mono- and sesquiterpenes, carbohy- drates, aromatics, and a variety of nitrogenous compounds. Interest in the study of this plant has centered primarily on the resinous fraction, as it is this material that is invested with the pharmacological activity that is peculiar to the plant. This resin is secreted by the female plant as a protective agent during seed ripening, although it can be found as a microscopic exudate through the aerial portions of plants of either sex. The pure resin, hashish or charas, is the most potent fraction of the plant, and has served as the source material for most of the chemical studies. The family of chemicals that has been isolated from this source has been referred to as the cannabinoid group. It is unique amongst psychotropic materials from plants in that there are no alkaloids present. The fraction is totally nitro- gen-free. Rather, the set of compounds can be considered as analogs of the parent compound cannabinol (I), a fusion product of terpene and a substituted resorcinol. Beyond the scope of this present review are such questions as the distribution of these compounds within the plant, the bo- tanic variability resulting from geographic distribution, the diversity of pharmacological action assignable to the several Reprinted from Journal of Psychedelic Drugs, vol. II, no. 1, 197 1. 397 398 Marijuana: Medical Papers distinct compounds present, and the various preparations and customs of administration. -
Synthetic Cannabinoids, Forensic & Legal Aspects
Synthetic Cannabinoids, Forensic & Legal Aspects Marilyn A. Huestis, PhD Chief, Chemistry & Drug Metabolism National Institute on Drug Abuse, National Institutes of Health Council of Forensic Medicine Istanbul, Turkey August 18, 2011 Synthetic Cannabinoid Overview Cannabinoid pharmacology Chemistry of synthetic cannabinoids Metabolism of synthetic cannabinoids Controlled drug administration studies Analytical methods for the identification of synthetic cannabinoids in biological & non-biological matrices Current legal status of synthetic cannabinoids Cannabis Mechanisms of Action THC binds to cannabinoid receptors & modulates endogenous cannabinoid & other neurotransmitter systems CB-1 receptors primarily in central nervous & cardiovascular systems CB-2 receptors primarily in immune system Non-CB1, non-CB2 receptors G-protein receptors discovered & cloned in late 1980’s Endogenous cannabinoids include anandamide, 2-AG, virodhamine, N-arachidonyl dopamine (NADA), oleamide, 2-arachidonyl glyceryl ether (noladin ether) & others High CB1 Receptor Density Hypothalamus Appetite, Hormones & Sexual behavior Neocortex High cognitive function & Sensory data Basal Ganglia integration Motor control & planning Hippocampus Memory & Learning Amygdala Anxiety, Emotion & Fear Cerebellum Brain Stem Motor control & Spinal Cord & coordination Vomiting reflex & Pain sensation Cannabinoid Mechanisms of Action Receptor distribution in brain correlates with areas involved in physiological, psychomotor & cognitive effects High density in caudate -

Synthetic Cannabis
Global emergence of synthetic cannabinoids Source: https://www.unodc.org/LSS/SubstanceGroup/Details/ae45ce06-6d33-4f5f-916a- e873f07bde02 Source: UNODC questionnaire on NPS, 2012 Background The appearance of ‘herbal highs’ in the market is not a new phenomenon. Such products usually consisted of plant mixtures with little psychoactive effects. Since 2004, however, the composition of these herbal products seems to have substantially changed to include potent new psychoactive compounds known as synthetic cannabinoids. Research on the mechanism of cannabis activity dates back several decades when molecules with similar behaviour to Δ9-tetrahydrocannabinol (THC) were first examined. A synthetic analogue of THC , ‘HU-210’, was first synthesized in Israel in 1988[1]and is considered to have a potency of at least 100 times more than THC. Due to its similar chemical structure to THC, ‘HU-210’ is regarded as a ‘classical cannabinoid’ and has been found in synthetic cannabinoids sold in the United States and other countries. Non-classical cannabinoids include cyclohexylphenols or 3-arylcyclohexanols (‘CP’compounds). ‘CP’ compounds were developed as potential analgesics by a pharmaceutical company in the 1980s. Respondents to the UNODC questionnaire on NPS have reported the emergence of CP-47,497 and CP-47,497-C8 in numerous countries in all regions except Africa since 2009. Other structurally dissimilar varieties of synthetic cannabinoids unrelated to THC have also emerged on the market. These include aminoalkylindoles, such as naphthoylindoles (e.g. JWH-018), phenylacetylindoles (e.g. JWH-250), and benzoylindoles (e.g. AM-2233).[2] JWH-018, arguably the most widely known synthetic cannabinoid, belongs to the group of aminoalkylindoles and is considered to be three times as potent as THC. -

The Cannabinoid WIN 55,212-2 Prevents Neuroendocrine Differentiation of Lncap Prostate Cancer Cells
OPEN Prostate Cancer and Prostatic Diseases (2016) 19, 248–257 www.nature.com/pcan ORIGINAL ARTICLE The cannabinoid WIN 55,212-2 prevents neuroendocrine differentiation of LNCaP prostate cancer cells C Morell1, A Bort1, D Vara2, A Ramos-Torres1, N Rodríguez-Henche1 and I Díaz-Laviada1 BACKGROUND: Neuroendocrine (NE) differentiation represents a common feature of prostate cancer and is associated with accelerated disease progression and poor clinical outcome. Nowadays, there is no treatment for this aggressive form of prostate cancer. The aim of this study was to determine the influence of the cannabinoid WIN 55,212-2 (WIN, a non-selective cannabinoid CB1 and CB2 receptor agonist) on the NE differentiation of prostate cancer cells. METHODS: NE differentiation of prostate cancer LNCaP cells was induced by serum deprivation or by incubation with interleukin-6, for 6 days. Levels of NE markers and signaling proteins were determined by western blotting. Levels of cannabinoid receptors were determined by quantitative PCR. The involvement of signaling cascades was investigated by pharmacological inhibition and small interfering RNA. RESULTS: The differentiated LNCaP cells exhibited neurite outgrowth, and increased the expression of the typical NE markers neuron-specific enolase and βIII tubulin (βIII Tub). Treatment with 3 μM WIN inhibited NK differentiation of LNCaP cells. The cannabinoid WIN downregulated the PI3K/Akt/mTOR signaling pathway, resulting in NE differentiation inhibition. In addition, an activation of AMP-activated protein kinase (AMPK) was observed in WIN-treated cells, which correlated with a decrease in the NE markers expression. Our results also show that during NE differentiation the expression of cannabinoid receptors CB1 and CB2 dramatically decreases. -

INTRODUCTION One of the Tasks of a Pharmacologist Is the Classification of Drugs
NEUROPSYCHOPHARMACOLOGIC STUDIES OF MARIJUANA: SOME SYNTHETIC AND NATURAL THC DERIVATIVES IN ANIMALS AND MAN* Edward F. Domino Department of Pharmacology, University of Michigan, Ann Arbor 48104 and Lafayette Clinic, Detroit, Mich. 48207 INTRODUCTION One of the tasks of a pharmacologist is the classification of drugs. Marijuana and its derivatives pose some problems. Legally marijuana has been classified as a narcotic, yet pharmacologically it is quite different. Mankind has known about the Cannabis plant from which marijuana and other products are obtained for more than 4,708 years. A considerable body of data is available to describe its gross effects. Over the centuries it has been called a depressant, euphoriant, ine- briant, intoxicant, hallucinogen, psychotomimetic, sedative-hypnotic-anesthetic, and stimulant. Perhaps more than any other drug it is a social irritant that elicits rather remarkable behavior reactions in both users and nonusers. Moreau’ in 1845, employed it to produce a model psychosis, thus initiating the fashion to study hallucinogens as a means of gaining insights into mental illness. Lewin2 classified Cannabis as one of the “phantastica: hallucinating substances.” One text on hallucinogens3 does not even refer to Cannabis, but another does? There are some aspects of the subjective effects of both LSD-25 and Cannabis that are similar, yet the latter produces sedative effects, no significant sympatho- mimetic actions, and no cross-tolerance to LSD-25. Hollister5 reviewed the re- cent findings on the effects in man of marijuana and its putative active ingredient Ag-THC, stressing that current investigators have, for the most part, confirmed the Cannabis-induced clinical syndromes long known to occur.