Situational Awareness and Forecasting for Norway
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Regionalt Bygdeutviklingsprogram for Oslo Og Viken 2019-2022
Regionalt bygdeutviklingsprogram for Oslo og Viken 2019-2022 For næringsutvikling og målrettet miljø- og klimaarbeid i landbruket i Oslo og Viken Fylkesmannen i Oslo og Viken Regionalt bygdeutviklingsprogram (RBU) 2 Innholdsfortegnelse Innledning ...................................................................................................................................................... 3 1. Oversikt over produksjoner og verdiskaping i landbruket i Oslo og Viken ......................... 4 Landbruket i Oslo og Viken .............................................................................................................. 4 Tradisjonelt jordbruk ........................................................................................................................ 5 Førstehåndsverdi av jordbruksproduksjonen ............................................................................... 7 Skogbruk ............................................................................................................................................. 8 Tilleggsnæringer ................................................................................................................................ 8 Definisjoner fra SSB .......................................................................................................................... 9 2. Visjon og overordna mål for utvikling av landbruket i Oslo og Viken .................................. 9 3. Synergier mellom delprogrammene ..................................................................................... -

How Uniform Was the Old Norse Religion?
II. Old Norse Myth and Society HOW UNIFORM WAS THE OLD NORSE RELIGION? Stefan Brink ne often gets the impression from handbooks on Old Norse culture and religion that the pagan religion that was supposed to have been in Oexistence all over pre-Christian Scandinavia and Iceland was rather homogeneous. Due to the lack of written sources, it becomes difficult to say whether the ‘religion’ — or rather mythology, eschatology, and cult practice, which medieval sources refer to as forn siðr (‘ancient custom’) — changed over time. For obvious reasons, it is very difficult to identify a ‘pure’ Old Norse religion, uncorroded by Christianity since Scandinavia did not exist in a cultural vacuum.1 What we read in the handbooks is based almost entirely on Snorri Sturluson’s representation and interpretation in his Edda of the pre-Christian religion of Iceland, together with the ambiguous mythical and eschatological world we find represented in the Poetic Edda and in the filtered form Saxo Grammaticus presents in his Gesta Danorum. This stance is more or less presented without reflection in early scholarship, but the bias of the foundation is more readily acknowledged in more recent works.2 In the textual sources we find a considerable pantheon of gods and goddesses — Þórr, Óðinn, Freyr, Baldr, Loki, Njo3rðr, Týr, Heimdallr, Ullr, Bragi, Freyja, Frigg, Gefjon, Iðunn, et cetera — and euhemerized stories of how the gods acted and were characterized as individuals and as a collective. Since the sources are Old Icelandic (Saxo’s work appears to have been built on the same sources) one might assume that this religious world was purely Old 1 See the discussion in Gro Steinsland, Norrøn religion: Myter, riter, samfunn (Oslo: Pax, 2005). -

3Rd OECD Roundtable on Cities and Regions for Sdgs 16-17 November 2020 Virtual Conference List of Participants
3rd OECD Roundtable on Cities and Regions for SDGs 16-17 November 2020 Virtual Conference List of Participants # Name Institution 1 Abra Walsh Onavance 2 Adnane Founoun Université Hassan 2 3 Adriana Agrimi Puglia Regione 4 Adriana Domingos Tribunal de Contas do Estado do Paraná 5 Adriano Greco da Fonseca Adriano Greco da Fonseca 6 Afsane Moeeni DOE 7 Agnes Lüdicke DeLoG 8 Agnes Rivet City and Eurometropolis of Strasbourg 9 Agustín Castillo-Martínez Ayuntamiento de Granada 10 Aissata M.B. Camara City of New York 11 Aïssatou N'Diaye-Sydnei European Commission (DG DEVCO) 12 Akrem Haddad H-Corp 13 Alessandra Norcini Regione Lombardia 14 Alessandro Santini Università IUAV di Venezia 15 Alessia Secci Università Iuav di Venezia 16 Alexander Hay University of Toronto 17 Alexander Trepelkov UN DESA 18 Alexandra Descôteaux #Meet4Impact 19 Alexandra Posypanková City of Bratislava 20 Alexandra Van Milink sciencespo 21 Alexandre Cesar Motta de Castro Procompetence Consultoria 22 Alexandre Gross 23 Alexandre Mohamedaly Ecorys 24 Ali Belgith 25 Alice Siragusa EC JRC 26 Alina Barysnikova Viken fylkeskommune Ministry of Public Works, Development and 27 Alina Huzui-Stoiculescu Administration 28 Aline Calefi Lima Fiep 29 Alys Solly Politecnico di Torino 30 Amalie Hilde Viken 31 Amie Figueiredo UNECE 32 Amit Yagur-Kroll Central Bureau of Statistics Israel 33 Ana Figueirôa Permanent Delegation of Portugal to the OECD 34 Ana Maria Mouro de Oliveira Gomes 1 Ana Rita Duarte Vacas Unidade Avaliação 35 Secretaria Ministério Ambiente - POSEUR e Monitorização 36 -
Kingdom of Sweden
Johan Maltesson A Visitor´s Factbook on the KINGDOM OF SWEDEN © Johan Maltesson Johan Maltesson A Visitor’s Factbook to the Kingdom of Sweden Helsingborg, Sweden 2017 Preface This little publication is a condensed facts guide to Sweden, foremost intended for visitors to Sweden, as well as for persons who are merely interested in learning more about this fascinating, multifacetted and sadly all too unknown country. This book’s main focus is thus on things that might interest a visitor. Included are: Basic facts about Sweden Society and politics Culture, sports and religion Languages Science and education Media Transportation Nature and geography, including an extensive taxonomic list of Swedish terrestrial vertebrate animals An overview of Sweden’s history Lists of Swedish monarchs, prime ministers and persons of interest The most common Swedish given names and surnames A small dictionary of common words and phrases, including a small pronounciation guide Brief individual overviews of all of the 21 administrative counties of Sweden … and more... Wishing You a pleasant journey! Some notes... National and county population numbers are as of December 31 2016. Political parties and government are as of April 2017. New elections are to be held in September 2018. City population number are as of December 31 2015, and denotes contiguous urban areas – without regard to administra- tive division. Sports teams listed are those participating in the highest league of their respective sport – for soccer as of the 2017 season and for ice hockey and handball as of the 2016-2017 season. The ”most common names” listed are as of December 31 2016. -

Regions and Counties in Norway
Regions and counties in Norway REGIONS AND COUNTIES IN NORWAY Northern Norway Northern Norway is located in the north and is also the most eastern region. This region comprises the two counties Troms og Finnmark and Nordland. If you visit Northern Norway in December or January, you can experience the polar night. The polar night is when the sun is under the horizon the whole day. In Northern Norway, you can see the northern lights in winter. Norway is divided into five regions. Northern Norway is located in the north of Northern lights. Photo: Pxhere.com the country. Trøndelag is located in the middle of the country. Western Norway is During summer, you can see the midnight in the west, and Eastern Norway is in the sun in Northern Norway. The midnight sun east. The region located in the south is is when the sun does not set, and a part of called Southern Norway. the sun is visible above the horizon all night. Every part of the country is divided into counties. There are 11 counties in Norway. Troms and Finnmark Troms og Finnmark is located furthest north and east and borders Russia, Finland 1 The National Centre of Multicultural Education, Native languages, morsmal.no Regions and counties in Norway and Sweden. Tromsø is the largest city in Troms og Finnmark. Norway's northernmost point, Knivskjellodden, is located in Troms og Finnmark. The North Cape (Nordkapp) is better known and is located almost as far north as Knivskjellodden. The North Cape is a famous tourist destination in Norway. Skrei cod hanging to dry on a rack. -
Preaspiration in the Nordic Languages Synchronic and Diachronic Aspects
Preaspiration in the Nordic Languages Synchronic and diachronic aspects Pétur Helgason PhD dissertation Department of Linguistics Stockholm University November 2002 Preaspiration in the Nordic Languages Synchronic and diachronic aspects Pétur Helgason PhD dissertation Stockholm University Department of Linguistics November 2002 PhD dissertation November 2002 Department of Linguistics Stockholm University 106 91 Stockholm Sweden © Pétur Helgason ISBN 91–7265–535–6 Cover Design: Christine Ericsdotter and Pétur Helgason. Front cover map: Evropa Recens Descripta by Guiliemo (Willem) Blaeu, 1649. Back cover map: Nova Totius Terrarum Orbis, by Frederik De Wit, 1660. Printed by Akademitryck AB, Edsbruk 2002 Abstract Preaspiration—the production of glottal friction at the juncture of a vowel and a consonant—appears to be typologically rare but is an areal lin- guistic feature of Northwestern Europe. This study contains a survey of the known geographical spread of preaspirated stops, their phonological distribution and phonetic expressions in some Nordic dialects. The study also suggests a reconstruction of the phonetics of the Proto-Nordic stop contrasts based on synchronic data as well as a more general framework of historical sound change. Following an introduction (Chapter 1), Chapter 2 deals with the definition and typology of preaspiration presenting a global overview of the known geographical spread of preaspiration. The apparent rarity of preaspiration is considered. Proposed, perceptually based explanations of this rarity are evaluated. Chapter 3 offers a fairly detailed account of the known areal spread of pre- aspiration in Europe. Stop systems of several dialects in which preaspira- tion occurs are analysed in terms of voicing conditions. These analyses are based mainly on descriptions provided in the dialectological literature. -

Integration Through Language Learning
Integration through language learning How do participants experience the Red Cross language practice program in terms of integration? Farnaz Nazir Chauhdry Masters of Philosophy in Psychology Psychology Department UNIVERSITY OF OSLO August 2016 I II How do participants experience the Red Cross language practice program in terms of integration? III Copyright Farnaz Nazir Chauhdry 2016 How do participants experience the Red Cross language practice program in terms of integration? Farnaz Nazir Chauhdry http://www.duo.uio.no Trykk: Reprosentralen, Universitetet i Oslo IV V VI Abstract Author: Farnaz Nazir Chauhdry Title: How do participants experience the Red Cross language practice program in terms of integration? Supervisor 1: Nora Sveaass Supervisor 2: Sigrun Marie Moss The study has explored the experiences of the participants while attending the Red Cross Norwegian Training Program with a specific focus on how this program has provided opportunities to the participants to adapt into the Norwegian society. The current study is based on qualitative data collected from twelve individual interviews and two focus group interviews with immigrants who currently attend the Red Cross Norwegian Training Program. The thesis is based on framework of Diaz’s Model of Integration and Nelson & Prilleltensky’s Prevention of psychological and social problems and Promotion of well-being. I have also used Urie Bronfenbrenner’s ecological model of human developement to present three types of prevention and promotion. The study adopts a thematic analysis and the experiences of the participants will be discussed with regards to previous challenges, their own sense of improvements in language and what this means for their integration as well as remaining challenges faced by the informants. -

Anbefaling Om Nedjustering Av Tiltak Etter Covid-19-Forskriften Til Kapittel
v4-29.07.2015 Returadresse: Helsedirektoratet, Postboks 220 Skøyen, 0213 Oslo, Norge HDIR Innland 41549129 HELSE- OG OMSORGSDEPARTEMENTET Deres ref.: Krisestab HOD Vår ref.: 21/7460-23 Postboks 8011 Dep Saksbehandler: Ingebjørg Skrindo 0030 OSLO Dato: 09.04.2021 Anbefaling om nedjustering av nasjonale tiltak etter covid-19 forskriften til kapittel 5B for kommunene Holmestrand, Horten, Tønsberg, Færder, Sandefjord og Larvik fra 12.04.2021 kl. 00.00 Se vedlagte anbefaling. OPPSUMMERING Helsedirektoratet anbefaler at den nasjonale reguleringen av tiltak i samsvar med covid-19- forskriften kapittel 5A nedjusteres til 5B for kommunene Holmestrand, Horten, Tønsberg, Færder, Sandefjord og Larvik. Tiltakene anbefales iverksatt fra 12.04.2021 kl. 00.00, med varighet til 22.04.2021 kl. 24.00. Kommunene har alle gjennomført lokale situasjonsvurderinger, og ønsker tiltak i tråd med det ovenstående. Kommunene må til enhver tid i tillegg konkret vurdere behovet for lokale råd og tiltak, og for samordning av tiltak for å redusere mobiliteten på tvers av kommunene. Anbefalingen er i samsvar med FHIs vurdering, Statsforvalters anmodning og kommunenes egne ønsker og vurderinger. Vennlig hilsen Johan Georg Røstad Torgersen e.f. direktør Ingebjørg Skrindo seniorrådgiver Dokumentet er godkjent elektronisk Kopi: STATSFORVALTEREN I VESTFOLD OG TELEMARK;FOLKEHELSEINSTITUTTET, Utbrudd @fhi.no Helsedirektoratet Avdeling kommunale helse- og omsorgstjenester Ingebjørg Skrindo Postboks 220 Skøyen, 0213 OSLO • Besøksadresse: Vitaminveien 4, Oslo • Tlf.: (+47) 47 47 20 20 Org.nr.: 983 544 622 • [email protected] • www.helsedirektoratet.no - 2 - 09.04.2021 Anbefaling om nedjustering av nasjonale tiltak etter covid-19 forskriften til kapittel 5B for kommunene Holmestrand, Horten, Tønsberg, Færder, Sandefjord og Larvik fra 12.04.2021 kl. -
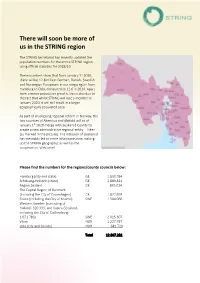
There Will Soon Be More of Us in the STRING Region
There will soon be more of us in the STRING region The STRING Secretariat has recently updated the population numbers for the entire STRING region using official statistics for 2018/19. These numbers show that from January 1st 2020, there will be 12.8 million German, Danish, Swedish and Norwegian Europeans in our megaregion from Hamburg to Oslo, compared to 12.6 in 2014. Apart from a minor population growth, this is also due to the fact that whilst STRING will lose a member in January 2020, it will still result in a larger geographically populated area. As part of an ongoing regional reform in Norway, the two counties of Akershus and Østfold will as of January 1st 2020 merge with Buskerud County to create a new administrative regional entity – Viken (as marked in the picture). The inclusion of Buskerud has inevitably led to more inhabitants now making up the STRING geography; as well as the cooperation. Welcome! Please find the numbers for the regions/county councils below: Hamburg (city and state) GE 1.830.584 Schleswig-Holstein (state) GE 2.889.821 Region Zealand DK 835.024 The Capital Region of Denmark (including the City of Copenhagen) DK 1.822.659 Skåne (including the City of Malmö) SWE 1.504.060 Western Sweden (consisting of Halland: 320.333; and Västra Götaland, including the City of Gothenburg: 1.671.783) SWE 2.015.607 Viken NOR 1.227.797 Oslo (city and county) NOR 681 729 Total 12.807.281 Sources: Cities: https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=urb_cpop1&lang=en Regions: https://ec.europa.eu/eurostat/cache/RCI/#?vis=nuts2.population&lang=en -

Northern Lights: Even Hammer and the Norwegian Enlightenment
Northern Lights: Even Hammer and the Norwegian Enlightenment Sophus A. Reinert Working Paper 17-054 Northern Lights: Even Hammer and the Norwegian Enlightenment Sophus A. Reinert Harvard Business School Working Paper 17-054 Copyright © 2016 by Sophus A. Reinert Working papers are in draft form. This working paper is distributed for purposes of comment and discussion only. It may not be reproduced without permission of the copyright holder. Copies of working papers are available from the author. Northern Lights: Even Hammer and the Norwegian Enlightenment Sophus A. Reinert1 Harvard Business School On 27 May 1776, the Scottish immigrant John Robertson Brand, sometimes known as John Brandt, was awarded a silver medal by the Royal Norwegian Scientific Society in the church of the fishing village of Hustad, south of the Trondheim Fjord in central Norway. Though below the Arctic Circle, Hustad lays slightly off the 63rd parallel north, which otherwise runs through Canada’s Nunavut and Yukon Territories, the Davis Strait, and the deep Russian tundra, far, far north of the traditional latitudes of Enlightenment. And yet, stepping into the small wooden church’s aisle on that spring day to deliver a speech marking the occasion, District Governor Even Hammer of Romsdal (1732-1800) summoned a language of reform, improvement, industriousness, civic virtue, public happiness, jealousy of trade, and political economy, that would have resonated deeply and widely across the European world, a language indebted to wider international currents but resolutely inflected by local conditions in what he appropriately called ‘our cold North’.2 Few cases better justify the great Turinese historian Franco Venturi’s admonition, a few 1 Rolv Petter Amdam first introduced me to Even Hammer, and I would like to express my gratitude to him, to Mads Langnes at Romsdalsmuseet in Molde for going well beyond the call of duty in facilitating my work on this intriguing figure, and, particularly, to Marit Sjelmo for jovial research assistance and Robert Fredona for invaluable suggestions. -

Reported Language Attitudes Among Norwegian Speaking In-Migrants in Tromsø
Acta Borealia A Nordic Journal of Circumpolar Societies ISSN: (Print) (Online) Journal homepage: https://www.tandfonline.com/loi/sabo20 Reported language attitudes among Norwegian speaking in-migrants in Tromsø Monica Sætermo & Hilde Sollid To cite this article: Monica Sætermo & Hilde Sollid (2021): Reported language attitudes among Norwegian speaking in-migrants in Tromsø, Acta Borealia, DOI: 10.1080/08003831.2021.1911209 To link to this article: https://doi.org/10.1080/08003831.2021.1911209 © 2021 The Author(s). Published by Informa UK Limited, trading as Taylor & Francis Group Published online: 03 May 2021. Submit your article to this journal Article views: 102 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=sabo20 ACTA BOREALIA https://doi.org/10.1080/08003831.2021.1911209 Reported language attitudes among Norwegian speaking in-migrants in Tromsø Monica Sætermoa and Hilde Sollidb aDepartment of Education, UiT The Arctic University of Norway, Tromsø, Norway; bDepartment of Language and Culture, UiT The Arctic University of Norway, Tromsø, Norway ABSTRACT ARTICLE HISTORY Today, in an era of increased mobility and migration, there is also Received 18 November 2020 increased in-migration within regions and countries. In the case Accepted 11 March 2021 of Norway, there is high tolerance for dialect use, and in this KEYWORDS context, it is interesting to ask which kinds of sociolinguistic Language attitudes; strategies in-migrants consider to be available given their current language ideologies; situation. This article explores the reported language attitudes sociolinguistic strategies; in- from the point of view of people who have moved to Tromsø migration; Norwegian from other parts of Norway. -

2021.01.27 National and Regional Corona Report (Engelsk).Pdf
Situational awareness and forecasting for Norway FHI COVID-19 modelling team Week 4, 27 January 2021 Highlights: • National epidemiological situation: Our models evaluate the present situation still as stable, though possibly with a start of a slightly growing trend. The effective reproduction number R acting in our changepoint model from 4 January is estimated to be 0.62 (median, 95% CI 0.37- 0.81). The estimated probability that R is larger than 1 is zero. The SMC model estimates the 7-days averaged effective reproduction number one week ago to be 0.78 (mean, 95% CI 0.61-0-97). There is accordance between the two models. In the SMC model, the estimated probability that the daily reproduction number one week ago was above 1 is 2.1%. The SMC model indicated a tendency to a decline of the averaged effective reproduction number starting in the days after Christmas. This negative trend appears to have reached its minimum, and the averaged effective reproduction number started to increase about ten days ago. Since the start of the epidemic, we estimate that in total 110.000 (95% CI 97.0000- 125.000) persons in Norway have been infected. The current estimate of the detection probability is around ∼65%. • National forecasting: In one week, we estimate ca 230 new cases per day (median; 95%CI 68- 450), and a prevalence (total number of infected people in Norway) of 1.730 (median; 95% CI 700-3.200). Hospitalisations in one week are estimated to be 110 (median 95% CI 75-140) and patients on ventilator treatment are estimated to be 22 (median 95% CI 12-31); the corresponding three-week projections are (95% CI 40 - 110) and (95% CI 5 - 23).