Bi-Allelic GOT2 Mutations Cause a Treatable Malate-Aspartate Shuttle
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Aspartate Aminotransferase (AST, GOT), Human Liver
BioVision 05/18 For research use only Aspartate Aminotransferase (AST, GOT), Human Liver CATALOG NO: P1299-100 1 units RELATED PRODUCTS: ALTERNATE NAMES: Aspartate Transaminase, Glutamate Oxaloacetate, AST, GOT, Aspartate Aminotransferase (AST) (Mouse) ELISA Kit (Cat. No. E4320) sGOT, AspAT, ASAT, serum glutamic oxaloacetic transaminase, AAT Aspartate Aminotransferase (AST) (Human) ELISA Kit (Cat. No. E4319) Aspartate Aminotransferase (AST) (Rat) ELISA Kit (Cat. No. E4321) SOURCE: Human Liver Aspartate Aminotransferase (AST or SGOT) Activity Colorimetric Assay Kit (Cat. PURITY: Purified No. K753) Anti-GOT2 Antibody (cat. No. A1273) MOL. WEIGHT: ~92 kDa Anti-GOT1 Antibody (Cat. No. A1272) FORM: Lyophilized GOT2, human recombinant (Cat. No. 7809) GOT1, human recombinant (Cat. No. 7808) STORAGE CONDITIONS: Store at -20°C. Avoid repeated freezing and thawing cycles. BIOLOGICAL ACTIVITY: ≥ 1 U/mg (Dimension® Clinical Chemistry System) UNIT DEFINITATION: One unit will catalyze the transamination of one micromole of L- aspartate to alpha-ketoglutarate forming L-glutamate and oxaloacetate per minute at 37°C and pH 7.8.Measured at 340 nm as one equimolar amount of NAD produced by a coupled reaction. RECONSTITUTION: > 1 mg/mL in tris buffered saline, 1% BSA, pH 8.0. AST/SGOT is found in many tissues throughout the body, including DESCRIPTION: the liver, heart, muscles, kidney, and brain. If any of these organs or tissues is affected by disease or injury, AST is released into the bloodstream. This means that AST isn't as specific an indicator of liver damage as ALT (also known as alanine aminotransferase, another type of enzyme found almost entirely in the liver). The ratio of AST and ALT levels are commonly used as biomarkers for liver health. -

Ornithine Aminotransferase, an Important Glutamate-Metabolizing Enzyme at the Crossroads of Multiple Metabolic Pathways
biology Review Ornithine Aminotransferase, an Important Glutamate-Metabolizing Enzyme at the Crossroads of Multiple Metabolic Pathways Antonin Ginguay 1,2, Luc Cynober 1,2,*, Emmanuel Curis 3,4,5,6 and Ioannis Nicolis 3,7 1 Clinical Chemistry, Cochin Hospital, GH HUPC, AP-HP, 75014 Paris, France; [email protected] 2 Laboratory of Biological Nutrition, EA 4466 PRETRAM, Faculté de Pharmacie, Université Paris Descartes, 75006 Paris, France 3 Laboratoire de biomathématiques, plateau iB2, Faculté de Pharmacie, Université Paris Descartes, 75006 Paris, France; [email protected] (E.C.); [email protected] (I.N.) 4 UMR 1144, INSERM, Université Paris Descartes, 75006 Paris, France 5 UMR 1144, Université Paris Descartes, 75006 Paris, France 6 Service de biostatistiques et d’informatique médicales, hôpital Saint-Louis, Assistance publique-hôpitaux de Paris, 75010 Paris, France 7 EA 4064 “Épidémiologie environnementale: Impact sanitaire des pollutions”, Faculté de Pharmacie, Université Paris Descartes, 75006 Paris, France * Correspondence: [email protected]; Tel.: +33-158-411-599 Academic Editors: Arthur J.L. Cooper and Thomas M. Jeitner Received: 26 October 2016; Accepted: 24 February 2017; Published: 6 March 2017 Abstract: Ornithine δ-aminotransferase (OAT, E.C. 2.6.1.13) catalyzes the transfer of the δ-amino group from ornithine (Orn) to α-ketoglutarate (aKG), yielding glutamate-5-semialdehyde and glutamate (Glu), and vice versa. In mammals, OAT is a mitochondrial enzyme, mainly located in the liver, intestine, brain, and kidney. In general, OAT serves to form glutamate from ornithine, with the notable exception of the intestine, where citrulline (Cit) or arginine (Arg) are end products. -

Supplementary Materials
1 Supplementary Materials: Supplemental Figure 1. Gene expression profiles of kidneys in the Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice. (A) A heat map of microarray data show the genes that significantly changed up to 2 fold compared between Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice (N=4 mice per group; p<0.05). Data show in log2 (sample/wild-type). 2 Supplemental Figure 2. Sting signaling is essential for immuno-phenotypes of the Fcgr2b-/-lupus mice. (A-C) Flow cytometry analysis of splenocytes isolated from wild-type, Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice at the age of 6-7 months (N= 13-14 per group). Data shown in the percentage of (A) CD4+ ICOS+ cells, (B) B220+ I-Ab+ cells and (C) CD138+ cells. Data show as mean ± SEM (*p < 0.05, **p<0.01 and ***p<0.001). 3 Supplemental Figure 3. Phenotypes of Sting activated dendritic cells. (A) Representative of western blot analysis from immunoprecipitation with Sting of Fcgr2b-/- mice (N= 4). The band was shown in STING protein of activated BMDC with DMXAA at 0, 3 and 6 hr. and phosphorylation of STING at Ser357. (B) Mass spectra of phosphorylation of STING at Ser357 of activated BMDC from Fcgr2b-/- mice after stimulated with DMXAA for 3 hour and followed by immunoprecipitation with STING. (C) Sting-activated BMDC were co-cultured with LYN inhibitor PP2 and analyzed by flow cytometry, which showed the mean fluorescence intensity (MFI) of IAb expressing DC (N = 3 mice per group). 4 Supplemental Table 1. Lists of up and down of regulated proteins Accession No. -

Supporting Information
Supporting Information Edgar et al. 10.1073/pnas.1601895113 SI Methods (Actimetrics), and recordings were analyzed using LumiCycle Mice. Sample size was determined using the resource equation: Data Analysis software (Actimetrics). E (degrees of freedom in ANOVA) = (total number of exper- – Cell Cycle Analysis of Confluent Cell Monolayers. NIH 3T3, primary imental animals) (number of experimental groups), with −/− sample size adhering to the condition 10 < E < 20. For com- WT, and Bmal1 fibroblasts were sequentially transduced − − parison of MuHV-4 and HSV-1 infection in WT vs. Bmal1 / with lentiviral fluorescent ubiquitin-based cell cycle indicators mice at ZT7 (Fig. 2), the investigator did not know the genotype (FUCCI) mCherry::Cdt1 and amCyan::Geminin reporters (32). of the animals when conducting infections, bioluminescence Dual reporter-positive cells were selected by FACS (Influx Cell imaging, and quantification. For bioluminescence imaging, Sorter; BD Biosciences) and seeded onto 35-mm dishes for mice were injected intraperitoneally with endotoxin-free lucif- subsequent analysis. To confirm that expression of mCherry:: Cdt1 and amCyan::Geminin correspond to G1 (2n DNA con- erin (Promega E6552) using 2 mg total per mouse. Following < ≤ anesthesia with isofluorane, they were scanned with an IVIS tent) and S/G2 (2 n 4 DNA content) cell cycle phases, Lumina (Caliper Life Sciences), 15 min after luciferin admin- respectively, cells were stained with DNA dye DRAQ5 (abcam) and analyzed by flow cytometry (LSR-Fortessa; BD Biosci- istration. Signal intensity was quantified using Living Image ences). To examine dynamics of replicative activity under ex- software (Caliper Life Sciences), obtaining maximum radiance perimental confluent conditions, synchronized FUCCI reporter for designated regions of interest (photons per second per − − − monolayers were observed by time-lapse live cell imaging over square centimeter per Steradian: photons·s 1·cm 2·sr 1), relative 3 d (Nikon Eclipse Ti-E inverted epifluorescent microscope). -

Glutamine Supports Pancreatic Cancer Growth Through a Kras- Regulated Metabolic Pathway
Glutamine supports pancreatic cancer growth through a Kras- regulated metabolic pathway The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Son, J., C. A. Lyssiotis, H. Ying, X. Wang, S. Hua, M. Ligorio, R. M. Perera, et al. 2013. “Glutamine supports pancreatic cancer growth through a Kras-regulated metabolic pathway.” Nature 496 (7443): 101-105. doi:10.1038/nature12040. http://dx.doi.org/10.1038/ nature12040. Published Version doi:10.1038/nature12040 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:11878814 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA NIH Public Access Author Manuscript Nature. Author manuscript; available in PMC 2013 October 04. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Nature. 2013 April 4; 496(7443): 101–105. doi:10.1038/nature12040. Glutamine supports pancreatic cancer growth through a Kras- regulated metabolic pathway Jaekyoung Son1,#, Costas A. Lyssiotis2,3,11,#, Haoqiang Ying4, Xiaoxu Wang1, Sujun Hua4, Matteo Ligorio8, Rushika M. Perera5, Cristina R. Ferrone8, Edouard Mullarky2,3,11, Ng Shyh- Chang2,9, Ya’an Kang10, Jason B. Fleming10, Nabeel Bardeesy5, John M. Asara3,6, Marcia C. Haigis7, Ronald A. DePinho4, Lewis C. Cantley2,3,11,*, and Alec -

IL21R Expressing CD14+CD16+ Monocytes Expand in Multiple
Plasma Cell Disorders SUPPLEMENTARY APPENDIX IL21R expressing CD14 +CD16 + monocytes expand in multiple myeloma patients leading to increased osteoclasts Marina Bolzoni, 1 Domenica Ronchetti, 2,3 Paola Storti, 1,4 Gaetano Donofrio, 5 Valentina Marchica, 1,4 Federica Costa, 1 Luca Agnelli, 2,3 Denise Toscani, 1 Rosanna Vescovini, 1 Katia Todoerti, 6 Sabrina Bonomini, 7 Gabriella Sammarelli, 1,7 Andrea Vecchi, 8 Daniela Guasco, 1 Fabrizio Accardi, 1,7 Benedetta Dalla Palma, 1,7 Barbara Gamberi, 9 Carlo Ferrari, 8 Antonino Neri, 2,3 Franco Aversa 1,4,7 and Nicola Giuliani 1,4,7 1Myeloma Unit, Dept. of Medicine and Surgery, University of Parma; 2Dept. of Oncology and Hemato-Oncology, University of Milan; 3Hematology Unit, “Fondazione IRCCS Ca’ Granda”, Ospedale Maggiore Policlinico, Milan; 4CoreLab, University Hospital of Parma; 5Dept. of Medical-Veterinary Science, University of Parma; 6Laboratory of Pre-clinical and Translational Research, IRCCS-CROB, Referral Cancer Center of Basilicata, Rionero in Vulture; 7Hematology and BMT Center, University Hospital of Parma; 8Infectious Disease Unit, University Hospital of Parma and 9“Dip. Oncologico e Tecnologie Avanzate”, IRCCS Arcispedale Santa Maria Nuova, Reggio Emilia, Italy ©2017 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2016.153841 Received: August 5, 2016. Accepted: December 23, 2016. Pre-published: January 5, 2017. Correspondence: [email protected] SUPPLEMENTAL METHODS Immunophenotype of BM CD14+ in patients with monoclonal gammopathies. Briefly, 100 μl of total BM aspirate was incubated in the dark with anti-human HLA-DR-PE (clone L243; BD), anti-human CD14-PerCP-Cy 5.5, anti-human CD16-PE-Cy7 (clone B73.1; BD) and anti-human CD45-APC-H 7 (clone 2D1; BD) for 20 min. -
Cyclin D1 Signaling Pathway in ER-Negative Breast Cancer Song Gao1, Anqi Ge3, Shouping Xu1, Zilong You1, Shipeng Ning1, Yashuang Zhao3* and Da Pang1,2*
Gao et al. Journal of Experimental & Clinical Cancer Research (2017) 36:179 DOI 10.1186/s13046-017-0648-4 RESEARCH Open Access PSAT1 is regulated by ATF4 and enhances cell proliferation via the GSK3β/β-catenin/ cyclin D1 signaling pathway in ER-negative breast cancer Song Gao1, Anqi Ge3, Shouping Xu1, Zilong You1, Shipeng Ning1, Yashuang Zhao3* and Da Pang1,2* Abstract Background: A growing amount of evidence has indicated that PSAT1 is an oncogene that plays an important role in cancer progression and metastasis. In this study, we explored the expression and function of PSAT1 in estrogen receptor (ER)-negative breast cancer. Method: The expression level of PSAT1 in breast cancer tissues and cells was analyzed using real-time-PCR (RT-PCR) , TCGA datasets or immunohistochemistry (IHC). The overall survival of patients with ER-negative breast cancer stratified by the PSAT1 expression levels was evaluated using Kaplan-Meier analysis. The function of PSAT1 was analyzed using a series of in vitro assays. Moreover, a nude mouse model was used to evaluate the function of PSAT1 in vivo. qRT-PCR and western blot assays were used to evaluate gene and protein expression, respectively, in the indicated cells. In addition, we demonstrated that PSAT1 was activated by ATF4 by chromatin immunoprecipitation (ChIP) assays. Results: mRNA expression of PSAT1 was up-regulated in ER-negative breast cancer. A tissue microarray that included 297 specimens of ER-negative breast cancer was subjected to an immunohistochemistry assay, which demonstrated that PSAT1 was overexpressed and predicted a poor clinical outcome of patients with this disease. -

Metabolomics Analysis Reveals Differential T-Cell Serine Metabolism As a Target in Autoimmunity
Metabolomics Analysis Reveals Differential T-Cell Serine Metabolism as a Target in Autoimmunity Gabriela Andrejeva Jeffrey Rathmell lab Vanderbilt University Medical Center [email protected] 2018 UK Metabolism Symposium Monday, 30th July 2018 Outline 2 dUMP dTMP Betaine aldehyde Choline TYMS CHDH Folate Se-Adenosylselenomethionine S-Adenosyl-L-methionine Dihydropteroate Dihydrofolate Cob(II)alamin 10-Formyltetrahydrofolylpolyglutamate10-Formyltetrahydrofolyl Betaine L-glutamate MAT2B MAT1A DHFR MAT2A Tetrahydrofolyl-[Glu](n) Formate Poly-L-glutamate ALDH1L2 MTR 3-Phospho-D-glycerate BHMT2 ALDH1L1 BHMT FPGS S-Adenosyl-L-homocysteine MTHFD1L GGH PHGDH MTHFD1 ATIC AHCYL1 L-Methionine MTHFD2 10-Formyltetrahydrofolate L-Homocysteine MTFMT "N,N-Dimethylglycine" Tetrahydrofolate 3-Phosphonooxypyruvate PDPR AHCY 5-Methyltetrahydrofolate Selenohomocysteine MTHFR GART "5,10-Methylenetetrahydrofolate" "5,10-Methenyltetrahydrofolate" DMGDH SHMT2 PSAT1O-Phospho-4-hydroxy-L-threonine IL4I1 MTHFS Cystathionine AMT Sarcosine SARDH SHMT1 5-Formyltetrahydrofolate O-Phospho-L-serine CBS FTCD N-Formimino-L-glutamate PSPH 2-Oxo-3-hydroxy-4-phosphobutanoate NAGS GNMT NH3 L-Serine L-Pipecolate PIPOX 5-Formiminotetrahydrofolate PPIG L-Cystathionine Thiocysteine Glycine Background and hypothesis GCAT Oxaloacetate L-AlanineL-Glutamate CTH 2-Oxobutanoate L-2-Amino-3-oxobutanoic acid L-Cysteine AGXT Hydroxypyruvate SDS ANPEP 2-Aminoacrylate ALAS2 AGXT2 S-Aminomethyldihydrolipoylprotein GLDC L-Cystine ALAS1 CP GOT1 GPT GPT2 GOT2 GSS ADC CO2 5-Aminolevulinate -

GOT2 Antibody Cat
GOT2 Antibody Cat. No.: 25-873 GOT2 Antibody Specifications HOST SPECIES: Rabbit SPECIES REACTIVITY: Human, Mouse, Rat Antibody produced in rabbits immunized with a synthetic peptide corresponding a region IMMUNOGEN: of human GOT2. TESTED APPLICATIONS: ELISA, WB GOT2 antibody can be used for detection of GOT2 by ELISA at 1:312500. GOT2 antibody APPLICATIONS: can be used for detection of GOT2 by western blot at 1 μg/mL, and HRP conjugated secondary antibody should be diluted 1:50,000 - 100,000. POSITIVE CONTROL: 1) 293T Cell Lysate PREDICTED MOLECULAR 45 kDa WEIGHT: Properties PURIFICATION: Antibody is purified by peptide affinity chromatography method. CLONALITY: Polyclonal CONJUGATE: Unconjugated PHYSICAL STATE: Liquid September 29, 2021 1 https://www.prosci-inc.com/got2-antibody-25-873.html Purified antibody supplied in 1x PBS buffer with 0.09% (w/v) sodium azide and 2% BUFFER: sucrose. CONCENTRATION: batch dependent For short periods of storage (days) store at 4˚C. For longer periods of storage, store GOT2 STORAGE CONDITIONS: antibody at -20˚C. As with any antibody avoid repeat freeze-thaw cycles. Additional Info OFFICIAL SYMBOL: GOT2 ALTERNATE NAMES: GOT2, FLJ40994, kat4, kativ, mitaat, KAT4, KATIV, mitAAT ACCESSION NO.: NP_002071 PROTEIN GI NO.: 73486658 GENE ID: 2806 USER NOTE: Optimal dilutions for each application to be determined by the researcher. Background and References Glutamic-oxaloacetic transaminase is a pyridoxal phosphate-dependent enzyme which exists in cytoplasmic and inner-membrane mitochondrial forms, GOT1 and GOT2, respectively. GOT plays a role in amino acid metabolism and the urea and tricarboxylic acid cycles. The two enzymes are homodimeric and show close homology.Glutamic- oxaloacetic transaminase is a pyridoxal phosphate-dependent enzyme which exists in BACKGROUND: cytoplasmic and inner-membrane mitochondrial forms, GOT1 and GOT2, respectively. -

Hepatic Phosphoserine Aminotransferase 1 Regulates Insulin Sensitivity in Mice Via Tribbles Homolog 3
Diabetes Volume 64, May 2015 1591 Junjie Yu, Fei Xiao, Yajie Guo, Jiali Deng, Bin Liu, Qian Zhang, Kai Li, Chunxia Wang, Shanghai Chen, and Feifan Guo Hepatic Phosphoserine Aminotransferase 1 Regulates Insulin Sensitivity in Mice via Tribbles Homolog 3 Diabetes 2015;64:1591–1602 | DOI: 10.2337/db14-1368 Phosphoserine aminotransferase 1 (PSAT1) is an en- particularly branched-chain amino acids, are closely re- zyme participating in serine synthesis. A role of PSAT1 in lated to the development and prediction of insulin resis- the regulation of insulin sensitivity, however, is un- tance in both human and animal models (5–7). Other known. In this study, we showed that hepatic PSAT1 studies have shown that, however, nonessential amino expression and liver serine levels are reduced in genet- acids might also be related to the development of insulin ically engineered leptin receptor–deficient (db/db) mice resistance. For example, high serum glycine levels are as- – and high-fat diet (HFD) induced diabetic mice. Addition- sociated with decreased risk of T2D in humans (8), and ally, overexpression of PSAT1 by adenovirus expressing glutamine supplementation attenuates high-fat diet METABOLISM PSAT1 improved insulin signaling and insulin sensitivity (HFD)-induced insulin resistance in rats (9). Despite these in vitro and in vivo under normal conditions. Opposite studies, the role that nonessential amino acids and the effects were observed when PSAT1 was knocked down enzymes related to their synthesis play in the regulation by adenovirus expressing small hairpin RNA specific for of insulin sensitivity remains unclear. PSAT1 (Ad-shPSAT1). Importantly, overexpression of fi Phosphoserine aminotransferase 1 (PSAT1), an enzyme PSAT1 also signi cantly ameliorated insulin resistance fi fi in diabetic mice. -
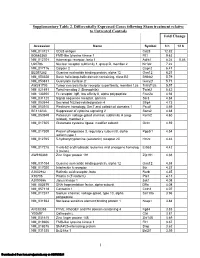
Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

Disorders Affecting Vitamin B6 Metabolism
Received: 8 October 2018 Accepted: 12 December 2018 DOI: 10.1002/jimd.12060 REVIEW Disorders affecting vitamin B6 metabolism Matthew P. Wilson1 | Barbara Plecko2 | Philippa B. Mills1 | Peter T. Clayton1 1Genetics and Genomic Medicine, UCL GOS Institute of Child Health, London, UK Abstract 0 2Department of Pediatrics and Adolescent Vitamin B6 is present in our diet in many forms, however, only pyridoxal 5 -phosphate Medicine, Division of General Pediatrics, (PLP) can function as a cofactor for enzymes. The intestine absorbs nonphosphorylated University Childrens' Hospital Graz, B vitamers, which are converted by specific enzymes to the active PLP form. The role Medical University Graz, Graz, Austria 6 of PLP is enabled by its reactive aldehyde group. Pathways reliant on PLP include Correspondence amino acid and neurotransmitter metabolism, folate and 1-carbon metabolism, protein Philippa B. Mills, Genetics and Genomic and polyamine synthesis, carbohydrate and lipid metabolism, mitochondrial function Medicine, UCL GOS Institute of Child Health, 30 Guilford Street, London WC1N and erythropoiesis. Besides the role of PLP as a cofactor B6 vitamers also play other 1EH, UK. cellular roles, for example, as antioxidants, modifying expression and action of steroid Email: [email protected] Communicating Editor: Slyvia Stockler- hormone receptors, affecting immune function, as chaperones and as an antagonist of Ipsiroglu Adenosine-5'-triphosphate (ATP) at P2 purinoceptors. Because of the vital role of PLP in neurotransmitter metabolism, particularly synthesis of the inhibitory transmitter Funding information γ Schweizerischer Nationalfonds zur -aminobutyric acid, it is not surprising that various inborn errors leading to PLP defi- Förderung der wissenschaftlichen Forschung ciency manifest as B6-responsive epilepsy, usually of early onset.