The Elusive but Painful Subtalar Joint in Rheumatoid Arthritis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Morphological Characteristics of the Lateral Talocalcaneal Ligament: a Large-Scale Anatomical Study
Surgical and Radiologic Anatomy (2019) 41:25–28 https://doi.org/10.1007/s00276-018-2128-8 ANATOMIC VARIATIONS Morphological characteristics of the lateral talocalcaneal ligament: a large-scale anatomical study Mutsuaki Edama1,2 · Ikuo Kageyama2 · Takaniri Kikumoto1 · Tomoya Takabayashi1 · Takuma Inai1 · Ryo Hirabayashi1 · Wataru Ito1 · Emi Nakamura1 · Masahiro Ikezu1 · Fumiya Kaneko1 · Akira Kumazaki3 · Hiromi Inaba4 · Go Omori3 Received: 9 August 2018 / Accepted: 4 September 2018 / Published online: 30 October 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract Purpose The purpose of this study is to clarify the morphological characteristics of the lateral talocalcaneal ligament (LTCL). Methods This study examined 100 legs from 54 Japanese cadavers. The LTCL was classified into three types: Type I, the LTCL branches from the calcaneofibular ligament (CFL); Type II, the LTCL is independent of the CFL and runs parallel to the calcaneus; and Type III, the LTCL is absent. The morphological features measured were fiber bundle length, fiber bundle width, and fiber bundle thickness. Results The LTCL was classified as Type I in 18 feet (18%), Type II in 24 feet (24%), and Type III in 58 feet (58%). All LTCLs were associated with the anterior talofibular ligament at the talus. There was no significant difference in morphologi- cal characteristics by Type for each ligament. Conclusions The LTCL was similar to the CFL in terms of fiber bundle width and fiber bundle thickness. Keywords Calcaneofibular · Ligament · Subtalar joint · Gross anatomy Introduction features, as well as complex three-dimensional mobility, making it a challenge to conduct quantitative evaluations. Of patients with chronic ankle instability, 42% [6] present Ligaments that are associated with the stability of the with mechanical instability of the talocrural joint, and 58% subtalar joint include the calcaneofibular ligament (CFL), have mechanical instability of the subtalar joint [3], each of the lateral talocalcaneal ligament (LTCL), the interosseous them at high percentages. -

Ankle Fusion Protocol
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -

SUBTALAR JOINT RECONSTRUCTION by George E
SUBTALAR JOINT RECONSTRUCTION By George E. Quill, Jr., M.D. The single axis subtalar joint is a hinge joining the talus and calcaneus that allows adaptation of the foot on uneven ground. This joint modifies the forces of ambulation imposed on the rest of the skeleton and influences the performance of the more distal foot articulations as well. When the structure and function of this joint are altered by trauma, instability, arthritis, infection, or tarsal coalition, subtalar reconstruction, usually in the form of arthrodesis, may prove to be a very successful procedure in treating the patient's resultant disability. The subtalar joint is, in this author's opinion, a very under appreciated joint. Even though it is estimated that up to 3 percent of the general population may have an asymptomatic talocalcaneal coalition present from a very young age and function very well, patients with a stiffened subtalar joint secondary to post-traumatic subtalar osteoarthrosis have very poor biomechanical function. Many patients presenting with "ankle " pain or who have pain from an ankle sprain that "just won't go away", may actually have subtalar pathology as an etiology for their discomfort. It is the astute orthopaedic surgeon who can recognize and successfully treat this pathology. Subtalar arthrodesis performed for the appropriate indications has proven to be one of this author's most gratifying, time-tested procedures in alleviating pain and improving function in patients so affected. Therefore, it is prudent that we understand the anatomic and functional aspects of the subtalar joint. The subtalar joint consists of three separate facets for articulation between the talus and calcaneus (Figure 1). -

ISOLATED SUBTALAR JOINT ARTHRODESIS: Indications, Evaluation, and Surgical Technique
CHAPTER 22 ISOLATED SUBTALAR JOINT ARTHRODESIS: Indications, Evaluation, and Surgical Technique Thomas A. Brosky, II, DPM Michael C. McGlamry, DPM Marie-Christine Bergeron, DPM Isolated subtalar joint (STJ) fusions are performed routinely as described by Sarraffi an. The talus and calcaneus move by many foot and ankle surgeons for various hindfoot in opposite directions: as the calcaneus abducts, everts and pathologies, but were historically avoided due to their extends, the talus will adduct, invert and plantarfl ex (9). potential complications on the adjacent joints (1). Since the inception of this isolated arthrodesis, multiple studies INDICATIONS have been undertaken to demonstrate the effects on the surrounding joints. Jouveniaux et al concluded with their Isolated STJ arthrodesis is indicated for the following: retrospective study of 37 isolated fusions that radiographic Stage II fl exible fl atfoot deformity, isolated arthritis, both changes suggesting arthritis in the adjacent joints were traumatic and non-traumatic, coalition, and neuromuscular common, but were moderate and asymptomatic in the disease affecting hindfoot motion (10). The literature majority of cases (2). Additionally, this technique is preferred has reported good results for stage II posterior tendon instead of a triple arthrodesis in cases where the calcaneal- dysfunction, but patient selection is the key to success (11). cuboid joint and talo-navicular joints are intact without Forefoot varus can be a contra-indication for this isolated arthritic changes. This preserves the overall function of the procedure unless it is addressed surgically (12). Taylor and hindfoot with the perceived joint stiffness that the triple Sammarco recommend isolated STJ arthrodesis in patients arthrodesis offers (3,4). -

The Subtalar Joint Sprain Occurs Some- Stabilizing Force to the Subtalar Joint
CHAPTER 26 THE SUBTAIARJOINT SPRAIN Gerard. V. Yu, D.P.M, Inversion injuries to the lateral ligamentous Rubin and \X/itten are credited as being the first complex of the ankle joint have been studied authors to suggest a clinical significance to subtalar extensively, and are readily recognized by joint instabiliry and propose a method to study the physicians treating disorders of the foot and ankle. instability.' They calculated the tibiocalcaneal angle Subtalar joint sprains, on the other hand, have been using a foot stabilizing device and stress the subject of few studies, and are a little-known tomograms. None of the 27 patients studied, and frequently undiagnosed clinical entity. It is (including 17 with symptoms of "excessive turning only over the last ten years that there has been any over") had obvious subtalar instability. serious interest in instability of the subtalar ioint as Christman and Snook, in a 1969 article a result of the "inversion ankle sprain." Some describing a modified Elmslie procedure for lateral orthopaedic literature has suggested the diagnosis ankle instability, recognized subtalar joint of subtalar joint instability as a distinct clinical instability at the time of surgery in three of their entity only after failure to achieve a "stable ankle" seven patients.'? Morbidity of the Christman-Snook following surgical reconstruction of the Lateral Procedure has been studied critically by Horstman ligamentous complex for ankle instability. Subtalar et al. as well as Snook et alj'a It has led some joint instability is estimated to occur in 1,0o/o to 25Vo authors to seek other procedures which are more percent of all patients exhibiting lateral ankle biomechanically and anatomically sound for instability. -

At the Seashore 299 300 MRI of the Ankle: Trauma and Overuse Disclosure
William J. Weadock, M.D. of the Presents The 18 th atRadiology the Seashore Friday, March 17, 2017 South Seas Island Resort Captiva Island, Florida Educational Symposia TABLE OF CONTENTS Friday, March 17, 2017 Ankle MRI: Trauma and Overuse (Corrie M. Yablon, M.D.) ............................................................................................ 299 Challenging Abdominal CT and MR Cases (William J. Weadock, M.D., FACR) ............................................................... 315 Knee MRI: A Pattern-Based Approach to Interpretation (Corrie M. Yablon, M.D.) ......................................................... 319 Complications of Aortic Endografts (William J. Weadock, M.D., FACR) ........................................................................... 339 SAVE THE DATE - 19 th Annual Radiology at the Seashore 299 300 MRI of the Ankle: Trauma and Overuse Disclosure Corrie M. Yablon, M.D. None Associate Professor Learning Objectives Introduction • Identify key anatomy on ankle MRI focusing on ligaments • MR protocol of the ankle • Discuss common injury patterns seen on ankle MRI • Ankle anatomy on MRI • Explain causes of ankle impingement • Case-based tutorial of pathology • Describe sites of nerve compression Protocol Planes Best to Evaluate… • Sag T1, STIR Axial Coronal • Ax T1, T2FS • Ankle tendons • Deltoid ligaments • Tibiofibular ligaments • Talar dome/ankle joint • Cor PDFS • Anterior, posterior talofibular • Plantar fascia • Optional coronal GRE for talar dome ligaments • Sinus tarsi cartilage -

Gross Anatomy of the Lower Limb. Knee and Ankle Joint. Walking
Gross anatomy of the lower limb. Knee and ankle joint. Walking. Sándor Katz M.D.,Ph.D. Knee joint type: trochoginglimus (hinge and pivot) Intracapsular ligaments: • Anterior cruciate lig. • Posterior cruciate lig. • Transverse lig. • Posterior meniscofemoral .lig. Medial meniscus: C- shaped. Lateral meniscus: almost a complete ring. Knee joint Extracapsular ligaments. Tibial collateral lig. is broader and fuses with the articular capsule and medial meniscus. Fibular collateral lig. is cord-like and separates from the articular capsule. Knee joint - extracapsular ligaments Knee joint - bursae Knee joint - movements • Flexion: 120-130° • Hyperextension: 5° • Voluntary rotation: 50-60° • Terminal rotation: 10° Ankle (talocrural) joint type: hinge Talocrural joint - medial collateral ligament Medial collateral = deltoid ligament Tibionavicular part (1) (partly covers the anterior tibiotalar part) Tibiocalcaneal part (2-3) Posterior tibiotalar part (4) Medial process (6) Sustentaculum tali (7) Tendon of tibialis posterior muscles (9) Talocrural joint - lateral collateral ligament Lateral collateral ligament Anterior talofibular ligament (5, 6) Calcaneofibular ligament (10) Lateral malleolus (1) Tibia (2) Syndesmosis tibiofibularis (3, 4) Talus (7) Collum tali (8) Caput tali (9) Interosseous talocalcaneal ligament (11) Cervical ligament (12) Talonavicular ligament (13) Navicular bone (14) Lateral collateral ligament Posterior talofibular ligament (5) Fibula (1) Tibia (2) Proc. tali, tuberculum laterale (3) Proc. tali, tuberculum mediale (11) Tendo, musculus felxor hallucis longus (8) Lig. calcaneofibulare (12) Tendo, musculus peroneus brevis (13) Tendo, musculus peroneus longus (14) Art. subtalaris (15) Talocrural joint - movements Dorsiflexion: 15° Plantarfelxion: 40° Talotarsal joint (lower ankle joint): talocalcaneonavicular joint and subtalar joint Bony surfaces: anterior and middle talar articular surfaces and head of the talus + anterior and middle calcaneal articular surfaces, navicular. -
Anatomical Reconstruction of the Spring Ligament Complex “Internal Brace” Augmentation
FASXXX10.1177/1938640013499404Foot & Ankle SpecialistFoot & Ankle Specialist 499404research-articleXXXX vol. 6 / no. 6 Foot & Ankle Specialist 441 〈 Evolving Techniques 〉 Anatomical Reconstruction of Jorge Acevedo, MD, and the Spring Ligament Complex Anand Vora, MD “Internal Brace” Augmentation Abstract: The calcaneonavicular the foot.1-5 Its anatomy has been well conjunction with other more commonly (spring) ligament complex is a critical defined, serving as a “hammock” to the applied procedures for extra-articular static support of the medial arch of talar head to maintain the reduced reconstructions. Furthermore, the use of the foot. Compromise of this structure position of the talus in its normal this procedure may decrease dependency has been implicated as a primary anatomical relationships with the on other nonanatomic reconstructive causative factor of talar derotation calcaneus and transverse tarsal procedures. leading to the clinical deformity of articulations.2 peritalar subluxation. Few procedures Many commonly performed extra- Preoperative Planning have been described to address articular reconstructive procedures this deficiency. The technique we attempt to correct adult flatfoot deformity Standard clinical and radiographic describe here is a simple yet effective using methods to realign bony or soft criteria are used to establish the method to reconstruct the spring tissue elements of the ligament complex that can easily foot to achieve talar be used in conjunction with other realignment.5-13 The calcaneonavicular (spring) ligament more commonly used procedures However, few for extra-articular reconstructions methods are able to complex has been well recognized as one of this deformity. We believe this directly address the “of the most critical static supporters of the procedure allows for a more powerful primary causative deformity correction and may decrease factor of talar medial arch of the foot.” dependency on other nonanatomic derotation. -

Musculoskeletal Joint Injection Order Improvement
Musculoskeletal Joint Injection Order Improvement Jonelle Petscavage-Thomas MD MPH Eric Walker MD Denny Duryea DO Victor Longo DO BACKGROUND • Fluoroscopic image guided therapeutic joint injections are performed daily by musculoskeletal radiologists at our institution • Injection sites range from large joints, such as the hip and shoulder, to smaller joints such as the hands, ankle, and feet • Procedure related risks include infection, bleeding, and contrast allergy 1 INCIDENT CASE 62 year-old man was referred for therapeutic fluoroscopic guided injection of the right ankle Figure: Order requisition sent for injection and scanned into PACS for radiologist INCIDENT CASE • Patient consented to procedure • Attending and fellow radiologist injected the right tibiotalar joint • Patient experienced immediate pain relief Figure: AP Fluoroscopic image confirms tibiotalar joint injection 2 INCIDENT CASE (continued) • Referring surgeon contacted attending radiologist 1 day later stating the intended injection site was the subtalar joint, not the tibiotalar joint • Patient returns for subtalar joint injection • Patient experiences pain relief with no complication Figure A. Subtalar joint injection PROBLEM IDENTIFIED: UNCLEAR SITE • When performing the procedure, the radiologists assumed that ankle referred to “tibiotalar” joint • However, “ankle” could also represent subtalar, calcaneocuboid, or talonavicular joint 3 INCIDENT CASE – FURTHER INVESTIGATION Electronic order in the medical record system consisted of a generic selection of: – Hip – Shoulder -

Subtalar Dislocation in an 8-Year-Old Boy: a Rare Clinical Presentation
A Case Report & Literature Review Subtalar Dislocation in an 8-Year-Old Boy: A Rare Clinical Presentation CPT Jeffrey R. Giuliani, MC; CPT Brett A. Freedman, MC; MAJ Scott B. Shawen, MC; and LTC Gerald L. Farber, MC ubtalar dislocation is a rare condition in adults, but it dorsolateral prominence. Ankle range of motion was gross- is rarer yet in patients less than 18 years old. In the ly normal, as was that of the hip and knee. Neurovascular few reports of pediatric subtalar dislocations, both examination was normal. adolescents and young adults have been included in Radiographs demonstrated a medial subtalar dislocation Sthe patient series.1-5 The youngest patient with a true dis- with talonavicular incongruency and widening of the sub- location reported to this point has been a 13-year-old girl. talar joint (Figure 1). With the boy under conscious seda- All the previously reported cases were secondary to trauma, tion in the emergency room, the subtalar joint was reduced and many had associated peritalar or ankle fractures. In the using axial traction, eversion, and digital pressure on the majority of the cases reported, the distal tibial and fibular talar head. The patient was then placed into a bulky Jones physes would likely have been closed. As a result, hyper- splint, and postreduction x-rays and a computed tomogra- inversion forces were prevented from dissipating through phy (CT) scan were completed (Figures 2 and 3). The CT the physis and instead were concentrated at the subtalar scan demonstrated concentric reduction with no evidence joint. In younger patients, the open physes about the ankle of associated fractures. -

Hind Foot Arthritis
PATIENT INFORMATION Hindfoot Arthritis Talonavicular joint Ankle joint Calcaneocuboid joint Subtalar or Talocalcaneal joint The hindfoot The hindfoot consists of three joints which lie around and below the ankle – These three joints include: • The talonavicular joint, where the talus connects to the inner midfoot bone (navicular) • The calcaneocuboid joint, where the heel bone connects to the outer midfoot bone (cuboid). • The subtalar or talocalcaneal joint, where the bottom of the talus connects to the heel bone (calcaneus); The hindfoot enables the foot to make the most of its sideways movements and provides flexibility to the foot particularly on uneven ground. These joints are separate to the ankle joint where most of the up and down movements occur. Source: Trauma & Orthopaedics Reference No: 5721-1 Issue date: 01/03/2021 Review date: 01/03/2024 Page: 1 of 7 A- Talonavicular joint B- Calcaneocuboid joint C- Subtalar or Talocalcaneal joint Figure 1 joints of the hindfoot What is hindfoot/ankle arthritis? Hindfoot arthritis can be caused by degeneration (osteoarthritis) or inflammation (e.g. rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis). In both cases the cartilage, which is the shiny white gristle that lines and articulates the joint, becomes damaged. This causes bone to rub on bone, which is painful. Osteoarthritis is usually secondary to damage to the joint, for example as a result of previous fracture, repeated sprains of the ankle, malalignment of the joint or infection. Excess body weight can overload a joint and worsen the symptoms of arthritis. Every extra kilogram of body weight is multiplied by 5 to 7 times when it is carried by the ankle. -
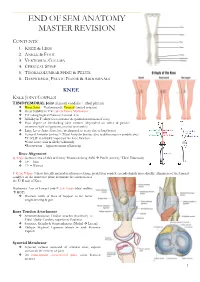
End of Sem Anatomy Master Revision
END OF SEM ANATOMY MASTER REVISION CONTENTS: 1. KNEE & LEGS 2. ANKLE & FOOT 3. VERTEBRAL COLUMN 4. CERVICAL SPINE 5. THORACOLUMBAR SPINE & PELVIS 6. DIAPHRAGM, PELVIC FLOOR & ABDOMINALS KNEE KNEE JOINT COMPLEX TIBIOFEMORAL Joint (femoral condyles + tibial plateau) ❖ Hinge Joint = Predominantly Uniaxial (limited rotation) ❖ Great Stability in E w/ Screw Home Mechanism ❖ F/E along Sagittal Plane on Coronal Axis ❖ Mobility in F (allow foot clearance & optimal orientation of foot) ❖ Poor degree of interlocking joint surfaces (dependent on active & passive structures such as ligaments, menisci & muscles) ❖ Large Lever Arms (therefore, predisposed to injury due to long bones) ❖ Femoral Articular Surface > Tibial Articular Surface (due to differences in condyle size) *5o of HE is critically important for knee function *Can’t rotate tibia & fibula voluntarily *Recurvatum = hyperextension of kneecap Knee Alignment Q Angle (between axis of tibia & femur): Measured along ASIS Patella (centre)/ Tibial Tuberosity ❖ 14o = Men ❖ 17o = Women 5o Genu Valgus: Tibia is laterally inclined in relation to femur; medial fem condyle extends slightly more distally. Alignment of the femoral condyles on the transverse plane determine the orientation of the F/ E axis of Knee Mechanical Axis of Lower Limb = 2-3o Varus (tibial midline HOF) ❖ Shortens width of Base of Support to for better weight-bearing & gait Knee Tendon Attachment ❖ Semimembranosus Tendon attaches posteriorly to Tibial Medial Condyle, superior to Popliteus ❖ Sartorius, Gracilis & Semitendinosus