Subtalar Joint Arthrodesis for Elective and Posttraumatic Foot and Ankle Deformities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
EM Cases Digest Vol. 1 MSK & Trauma
THE MAGAZINE SERIES FOR ENHANCED EM LEARNING Vol. 1: MSK & Trauma Copyright © 2015 by Medicine Cases Emergency Medicine Cases by Medicine Cases is copyrighted as “All Rights Reserved”. This eBook is Creative Commons Attribution-NonCommercial- NoDerivatives 3.0 Unsupported License. Upon written request, however, we may be able to share our content with you for free in exchange for analytic data. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Medicine Cases 216 Balmoral Ave Toronto, ON, M4V 1J9 www.emergencymedicinecases.com This book has been authored with care to reflect generally accepted practices. As medicine is a rapidly changing field, new diagnostic and treatment modalities are likely to arise. It is the responsibility of the treating physician, relying on his/her experience and the knowledge of the patient, to determine the best management plan for each patient. The author(s) and publisher of this book are not responsible for errors or omissions or for any consequences from the application of the information in this book and disclaim any liability in connection with the use of this information. This book makes no guarantee with respect to the completeness or accuracy of the contents within. OUR THANKS TO... EDITORS IN CHIEF Anton Helman Taryn Lloyd PRODUCTION EDITOR Michelle Yee PRODUCTION MANAGER Garron Helman CHAPTER EDITORS Niran Argintaru Michael Misch PODCAST SUMMARY EDITORS Lucas Chartier Keerat Grewal Claire Heslop Michael Kilian PODCAST GUEST EXPERTS Andrew Arcand Natalie Mamen Brian Steinhart Mike Brzozowski Hossein Mehdian Arun Sayal Ivy Cheng Sanjay Mehta Laura Tate Walter Himmel Jonathan Pirie Rahim Valani Dave MacKinnon Jennifer Riley University of Toronto, Faculty of Medicine EM Cases is a venture of the Schwartz/ Reisman Emergency Medicine Institute. -

Morphological Characteristics of the Lateral Talocalcaneal Ligament: a Large-Scale Anatomical Study
Surgical and Radiologic Anatomy (2019) 41:25–28 https://doi.org/10.1007/s00276-018-2128-8 ANATOMIC VARIATIONS Morphological characteristics of the lateral talocalcaneal ligament: a large-scale anatomical study Mutsuaki Edama1,2 · Ikuo Kageyama2 · Takaniri Kikumoto1 · Tomoya Takabayashi1 · Takuma Inai1 · Ryo Hirabayashi1 · Wataru Ito1 · Emi Nakamura1 · Masahiro Ikezu1 · Fumiya Kaneko1 · Akira Kumazaki3 · Hiromi Inaba4 · Go Omori3 Received: 9 August 2018 / Accepted: 4 September 2018 / Published online: 30 October 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract Purpose The purpose of this study is to clarify the morphological characteristics of the lateral talocalcaneal ligament (LTCL). Methods This study examined 100 legs from 54 Japanese cadavers. The LTCL was classified into three types: Type I, the LTCL branches from the calcaneofibular ligament (CFL); Type II, the LTCL is independent of the CFL and runs parallel to the calcaneus; and Type III, the LTCL is absent. The morphological features measured were fiber bundle length, fiber bundle width, and fiber bundle thickness. Results The LTCL was classified as Type I in 18 feet (18%), Type II in 24 feet (24%), and Type III in 58 feet (58%). All LTCLs were associated with the anterior talofibular ligament at the talus. There was no significant difference in morphologi- cal characteristics by Type for each ligament. Conclusions The LTCL was similar to the CFL in terms of fiber bundle width and fiber bundle thickness. Keywords Calcaneofibular · Ligament · Subtalar joint · Gross anatomy Introduction features, as well as complex three-dimensional mobility, making it a challenge to conduct quantitative evaluations. Of patients with chronic ankle instability, 42% [6] present Ligaments that are associated with the stability of the with mechanical instability of the talocrural joint, and 58% subtalar joint include the calcaneofibular ligament (CFL), have mechanical instability of the subtalar joint [3], each of the lateral talocalcaneal ligament (LTCL), the interosseous them at high percentages. -

Comparison of Diagnostic Accuracy of Bedside Ultrasonography and Radiography for Calcaneal Fractures in the Emergency Department
Open Access http://jept.ir Publish Free doi 10.34172/jept.2020.36 Journal of Emergency Practice and Trauma Original Article Volume 7, Issue 1, 2021, 2020, p. 17-21 Comparison of diagnostic accuracy of bedside ultrasonography and radiography for calcaneal fractures in the emergency department Majid Zamani ID , Maliheh Mazaheri ID , Farhad Heydari* ID , Babak Masoumi ID Department of Emergency Medicine, Faculty of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran Received: 1 June 2020 Abstract Accepted: 14 September 2020 Objective: Ultrasonography (US) is not the method of choice for the diagnosis of calcaneal Published online: 24 September fractures. The aim of this study was to compare the diagnostic accuracy of US with plain 2020 radiography in the diagnosis of calcaneus fractures following blunt ankle and foot trauma. *Corresponding author: Methods: In this cross-sectional study, 214 patients (over 18 years) presenting to the Farhad heydari; Emergency emergency department (ED) with suspicion of traumatic calcaneus fracture following acute Medicine Specialist; Department of Emergency Medicine, Faculty blunt trauma, were enrolled. Bedside ultrasonography was performed and interpreted by of Medicine, Isfahan University of emergency physicians. After that, plain radiography was performed. Furthermore, all the Medical Sciences, Isfahan, Iran patients were assessed by computed tomography (CT) scan as the gold standard. Alzahra Hospital, Sofeh Ave, Keshvari Results: Finally, 193 patients were enrolled with a mean age of 29.4 ± 15.7 years (85.5% Blvd., Isfahan, Iran. male). Fractures in the calcaneus were detected in 49 patients. The sensitivity and specificity Tel: +989131367643; Email: [email protected] of ultrasonography in the detection of calcaneal fractures were 83.6%, (confidence interval (CI), 69.7 –92.2) and 100% (95% CI, 96.7 –100), while the sensitivity and specificity of X-ray Competing interests: None. -

Talo-Calcaneal Distraction Ilizarov Frame: an Ergonomic Method to Manage Intra-Articular Fractures of Calcaneum
ORIGINAL ARTICLE ASIAN JOURNAL OF MEDICAL SCIENCES Talo-calcaneal distraction Ilizarov frame: an ergonomic method to manage intra-articular fractures of calcaneum Anoop Raj Singh1, Javed Ahmad 2, Vivek Kumar Shrivastava3, Pavneesh Kumar4 1Assistant Professor, Department of Orthopedics, SMMH Medical College, Saharanpur, Uttar Pradesh, India, 2,3Assistant Professor, Department of Orthopedics, Mahamaya Rajkiya Allopathic Medical College, Ambedkar Nagar, Uttar Pradesh, India, SMMH Medical College, Saharanpur, Uttar Pradesh, India, 4Assistant Professor, Department of Orthopedics, Government Doon Medical College Dehradun, India Submission: 07-03-2021 Revision: 27-05-2021 Publication: 01-07-2021 ABSTRACT Background: Principle of distraction and an indirect reduction was used to promote healing of Access this article online fractures and adequate regeneration of cartilage at the subtalar joint. Aims and Objectives: The Website: study was aimed to elaborate and develop role of Ilizarov as an alternative biological method to manage intraarticular fracture calcaneum with minimal chances of infection. http://nepjol.info/index.php/AJMS Materials and Methods: Twenty-one patients were studied and the mean age of patients DOI: 10.3126/ajms.v12i7.35459 was 40.7 years (span: 20 to 65 years). Sanders CT classification was used to divide into E-ISSN: 2091-0576 type II, 11 (52.38%); type III, 7 (33.33%) and type IV, 3 (14.28%). The average follow-up P-ISSN: 2467-9100 was 17.2 months (range: 6 to 24 months). AOFAS scale for ankle and hindfoot was used for assessment of patients- 7 (33.33%) excellent, 7 (33.33%) good, 3 (14.28%) fair, and 4 Copyright (c) 2021 Asian Journal of (19.04%) poor results. -

Calcaneal Fracture and Rehabilitation
1 Calcaneal Fracture and Rehabilitation Surgical Indications and Considerations Anatomic Considerations: The calcaneus articulates with the talus superiorly at the subtalar joint. The three articulating surfaces of the subtalar joint are the: anterior, middle, and posterior facets, with the posterior facet representing the major weight-bearing surface. The subtalar joint is responsible for the majority of foot inversion/eversion (or pronation/supination). The interosseous ligament and medial, lateral, and posterior talocalcaneal ligaments provide additional support for the joint. The tibial artery, nerve, posterior tibial tendon, and flexor hallucis longus tendon are located medially to the calcaneus and are at risk for impingement with a calcaneal fracture, as are the peroneal tendons located on the lateral aspect of the calcaneus. The calcaneus serves three major functions: 1) acts as a foundation and support for the body’s weight, 2) supports the lateral column of the foot and acts as the main articulation for inversion/eversion, and 3) acts as a lever arm for the gastrocnemius muscle complex. Pathogenesis: Fractures of the calcaneal body, anterior process, sustentaculum tali, and superior tuberosity are known as extra-articular fractures and usually occur as a result of blunt force or sudden twisting. Fractures involving any of the three subtalar articulating surfaces are known as intra-articular fractures and are common results of: a fall from a height usually 6 feet or more, a motor vehicle accident (MVA), or an impact on a hard surface while running or jumping. Intra-articular fractures are commonly produced by axial loading; a combination of shearing and compression forces produce both the primary and secondary fracture lines. -
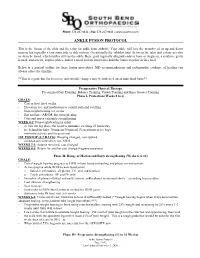
Ankle Fusion Protocol
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -

SUBTALAR JOINT RECONSTRUCTION by George E
SUBTALAR JOINT RECONSTRUCTION By George E. Quill, Jr., M.D. The single axis subtalar joint is a hinge joining the talus and calcaneus that allows adaptation of the foot on uneven ground. This joint modifies the forces of ambulation imposed on the rest of the skeleton and influences the performance of the more distal foot articulations as well. When the structure and function of this joint are altered by trauma, instability, arthritis, infection, or tarsal coalition, subtalar reconstruction, usually in the form of arthrodesis, may prove to be a very successful procedure in treating the patient's resultant disability. The subtalar joint is, in this author's opinion, a very under appreciated joint. Even though it is estimated that up to 3 percent of the general population may have an asymptomatic talocalcaneal coalition present from a very young age and function very well, patients with a stiffened subtalar joint secondary to post-traumatic subtalar osteoarthrosis have very poor biomechanical function. Many patients presenting with "ankle " pain or who have pain from an ankle sprain that "just won't go away", may actually have subtalar pathology as an etiology for their discomfort. It is the astute orthopaedic surgeon who can recognize and successfully treat this pathology. Subtalar arthrodesis performed for the appropriate indications has proven to be one of this author's most gratifying, time-tested procedures in alleviating pain and improving function in patients so affected. Therefore, it is prudent that we understand the anatomic and functional aspects of the subtalar joint. The subtalar joint consists of three separate facets for articulation between the talus and calcaneus (Figure 1). -

Radiographic Evaluation of Calcaneal Fractures; to Measure Or Not to Measure T
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Erasmus University Digital Repository Radiographic evaluation of calcaneal fractures; To measure or not to measure T. Schepers, A.Z. Ginai, P.G.H. Mulder, P. Patka Skeletal Radiol 2007;36(9):847-852 Abstract Objective The aim of this study was to correlate the functional outcome after treatment for displaced intra-articular calcaneal fracture with plain radiography. Design Prognostic study of a retrospective cohort with concurrent follow-up. Patients A total of 33 patients with a unilateral calcaneal fracture and a minimum follow-up of 13 months participated. Patients filled in three disease-specific questionnaires, graded their satisfaction and the indication for an arthrodesis was noted. Standardised radiographs were made of the previously injured side and the normal (control) side. Different angles and distances were measured on these radiographs and compared with values described in the literature. The differences in values in angles and distances between the injured and uninjured (control) foot were correlated with the outcome of the questionnaires, and the indication for an arthrodesis. Results None of the angles correlated with the disease-specific outcome scores. Of the angles only the tibiotalar angle correlated with the VAS (r=0.35, p=0.045) and only the absolute foot height correlated with the indication for an arthrodesis (odds=0.70, CI=0.50–0.99). Conclusions In this study the radiographic evaluation correlated poorly with the final outcome. Measurements on plain radiographs seem not to be useful in determining outcome after intra-articular calcaneal fractures. -

ISOLATED SUBTALAR JOINT ARTHRODESIS: Indications, Evaluation, and Surgical Technique
CHAPTER 22 ISOLATED SUBTALAR JOINT ARTHRODESIS: Indications, Evaluation, and Surgical Technique Thomas A. Brosky, II, DPM Michael C. McGlamry, DPM Marie-Christine Bergeron, DPM Isolated subtalar joint (STJ) fusions are performed routinely as described by Sarraffi an. The talus and calcaneus move by many foot and ankle surgeons for various hindfoot in opposite directions: as the calcaneus abducts, everts and pathologies, but were historically avoided due to their extends, the talus will adduct, invert and plantarfl ex (9). potential complications on the adjacent joints (1). Since the inception of this isolated arthrodesis, multiple studies INDICATIONS have been undertaken to demonstrate the effects on the surrounding joints. Jouveniaux et al concluded with their Isolated STJ arthrodesis is indicated for the following: retrospective study of 37 isolated fusions that radiographic Stage II fl exible fl atfoot deformity, isolated arthritis, both changes suggesting arthritis in the adjacent joints were traumatic and non-traumatic, coalition, and neuromuscular common, but were moderate and asymptomatic in the disease affecting hindfoot motion (10). The literature majority of cases (2). Additionally, this technique is preferred has reported good results for stage II posterior tendon instead of a triple arthrodesis in cases where the calcaneal- dysfunction, but patient selection is the key to success (11). cuboid joint and talo-navicular joints are intact without Forefoot varus can be a contra-indication for this isolated arthritic changes. This preserves the overall function of the procedure unless it is addressed surgically (12). Taylor and hindfoot with the perceived joint stiffness that the triple Sammarco recommend isolated STJ arthrodesis in patients arthrodesis offers (3,4). -

Paget's Disease of Bone Affecting Peripheral Limb
J Bone Metab 2020;27(1):71-75 https://doi.org/10.11005/jbm.2020.27.1.71 pISSN 2287-6375 eISSN 2287-7029 Case Report Paget’s Disease of Bone Affecting Peripheral Limb: Difficulties in Diagnosis: A Case Report Jun-Ku Lee1, Yun Kyung Kang2, Pei Wei Wang1, Soo Min Hong3 1Department of Orthopaedic Surgery, Seoul Paik Hospital, Inje University College of Medicine, Seoul; 2Department of Pathology, Seoul Paik Hospital, Inje University College of Medicine, Seoul; 3Department of Internal Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea Corresponding author In terms of management of Paget’s disease of bone (PDB), early diagnosis and proper Soo Min Hong management achieving remission is essential with lifelong specialist follow-up. We pres- Department of Internal Medicine, Seoul Paik ent the case of a 40-year-old woman with PDB affecting mainly the distal extremities Hospital, Inje University College of Medicine, (ankle and wrist). The patient visited our hospital in 2012 with heel pain. Plain radiogra- Mareunnae-ro 9, Jung-gu, Seoul 04551, Korea phy revealed osteoporosis, and a bone scan revealed hot uptake. Initial laboratory inves- Tel: +82-2-2270-0001 tigations showed normal serum calcium, 25-hydroxy-vitamin D, and parathyroid hor- Fax: +82-2-2270-5289 mone levels; however, osteocalcin, C-terminal telopeptide of type I collagen, and bone E-mail: [email protected] alkaline phosphatase levels were elevated. A bone mineral density scan showed T- and Z-scores of -2.5 and -2.7, respectively, and bisphosphonate treatment was initiated. Bi- Received: December 25, 2019 opsy performed on the calcaneal lateral wall revealed inconclusive findings. -

Calcaneal Fracture Management Extensile Lateral Approach Versus Small Incision Technique
Calcaneal Fracture Management Extensile Lateral Approach Versus Small Incision Technique a, b Nathan J. Kiewiet, MD *, Bruce J. Sangeorzan, MD KEYWORDS Calcaneus fracture Extensile lateral approach Percutaneous fixation calcaneus KEY POINTS Calcaneal fracture management continues to be an area of sustained interest. Extensile lateral approach to the calcaneus carries significant risks of wound complica- tions and infection. Small incision techniques may reduce risks and improve recovery. Less invasive techniques have been shown to reduce risk of wound-healing complications. INTRODUCTION Intra-articular calcaneus fractures have long been a vexing problem for the treating or- thopedic surgeon. First described by Malgaigne in 1843, calcaneus fractures were not consistently diagnosed until the development of radiography in the late 1890s. The most common tarsal bone fracture, calcaneal fractures currently account for approx- imately 2% of all fractures; displaced intra-articular fractures represent 60% to 75% of all calcaneal fractures. Historically these fractures were treated nonoperatively; but over the past few de- cades, surgical fixation has become more prevalent. Cotton1 identified the poor outcome associated with treatment without reduction and favored closed manipulation using a hammer to reduce the lateral wall and reimpact the fracture and suggested that open reduction is contraindicated. By the 1920s, Cotton2 reported on his treatment of Disclosures: The authors have nothing to disclose. a Drisko, Fee, and Parkins Orthopedic Surgery, 19550 East 39th Street, Suite 410, Independence, MO 64057, USA; b Department of Orthopedics and Sports Medicine, Harborview Medical Cen- ter, University of Washington, 325 9th Avenue, Seattle, WA 98104, USA * Corresponding author. E-mail address: [email protected] Foot Ankle Clin N Am 22 (2017) 77–91 http://dx.doi.org/10.1016/j.fcl.2016.09.013 foot.theclinics.com 1083-7515/17/ª 2016 Elsevier Inc. -

The Subtalar Joint Sprain Occurs Some- Stabilizing Force to the Subtalar Joint
CHAPTER 26 THE SUBTAIARJOINT SPRAIN Gerard. V. Yu, D.P.M, Inversion injuries to the lateral ligamentous Rubin and \X/itten are credited as being the first complex of the ankle joint have been studied authors to suggest a clinical significance to subtalar extensively, and are readily recognized by joint instabiliry and propose a method to study the physicians treating disorders of the foot and ankle. instability.' They calculated the tibiocalcaneal angle Subtalar joint sprains, on the other hand, have been using a foot stabilizing device and stress the subject of few studies, and are a little-known tomograms. None of the 27 patients studied, and frequently undiagnosed clinical entity. It is (including 17 with symptoms of "excessive turning only over the last ten years that there has been any over") had obvious subtalar instability. serious interest in instability of the subtalar ioint as Christman and Snook, in a 1969 article a result of the "inversion ankle sprain." Some describing a modified Elmslie procedure for lateral orthopaedic literature has suggested the diagnosis ankle instability, recognized subtalar joint of subtalar joint instability as a distinct clinical instability at the time of surgery in three of their entity only after failure to achieve a "stable ankle" seven patients.'? Morbidity of the Christman-Snook following surgical reconstruction of the Lateral Procedure has been studied critically by Horstman ligamentous complex for ankle instability. Subtalar et al. as well as Snook et alj'a It has led some joint instability is estimated to occur in 1,0o/o to 25Vo authors to seek other procedures which are more percent of all patients exhibiting lateral ankle biomechanically and anatomically sound for instability.