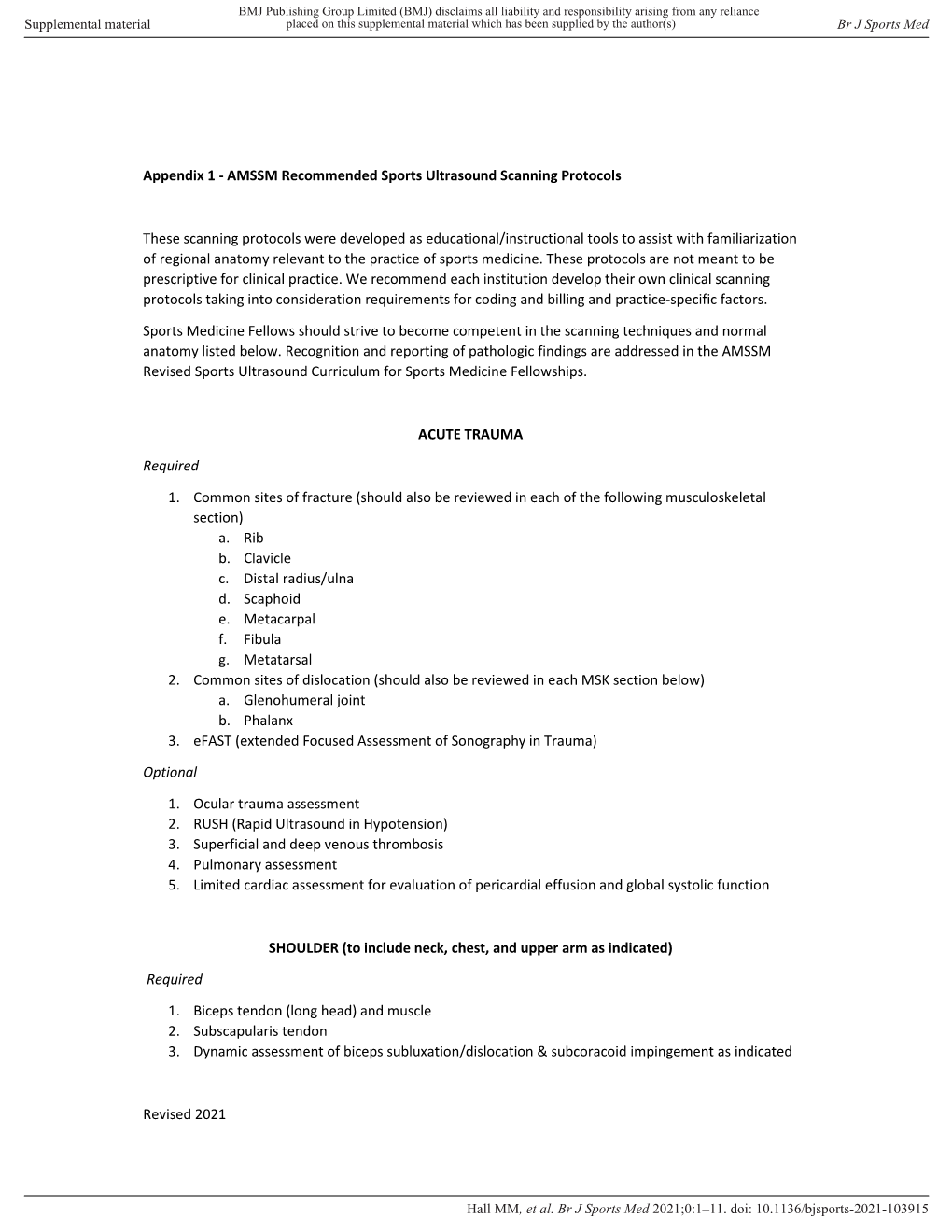
Revised 2021 Appendix 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plantar Fascia-Specific Stretching Program for Plantar Fasciitis
Plantar Fascia-Specific Stretching Program For Plantar Fasciitis Plantar Fascia Stretching Exercise 1. Cross your affected leg over your other leg. 2. Using the hand on your affected side, take hold of your affected foot and pull your toes back towards shin. This creates tension/stretch in the arch of the foot/plantar fascia. 3. Check for the appropriate stretch position by gently rubbing the thumb of your unaffected side left to right over the arch of the affected foot. The plantar fascia should feel firm, like a guitar string. 4. Hold the stretch for a count of 10. A set is 10 repetitions. 5. Perform at least 3 sets of stretches per day. You cannot perform the stretch too often. The most important times to stretch are before taking the first step in the morning and before standing after a period of prolonged sitting. Plantar Fascia Stretching Exercise 1 2 3 4 URMC Orthopaedics º 4901 Lac de Ville Boulevard º Building D º Rochester, NY 14618 º 585-275-5321 www.ortho.urmc.edu Over, Please Anti-inflammatory Medicine Anti-inflammatory medicine will help decrease the inflammation in the arch and heel of your foot. These include: Advil®, Motrin®, Ibuprofen, and Aleve®. 1. Use the medication as directed on the package. If you tolerate it well, take it daily for 2 weeks then discontinue for 1 week. If symptoms worsen or return, then resume medicine for 2 weeks, then stop. 2. You should eat when taking these medications, as they can be hard on your stomach. Arch Support 1. -

Musculoskeletal Ultrasound Technical Guidelines II. Elbow
European Society of MusculoSkeletal Radiology Musculoskeletal Ultrasound Technical Guidelines II. Elbow Ian Beggs, UK Stefano Bianchi, Switzerland Angel Bueno, Spain Michel Cohen, France Michel Court-Payen, Denmark Andrew Grainger, UK Franz Kainberger, Austria Andrea Klauser, Austria Carlo Martinoli, Italy Eugene McNally, UK Philip J. O’Connor, UK Philippe Peetrons, Belgium Monique Reijnierse, The Netherlands Philipp Remplik, Germany Enzo Silvestri, Italy Elbow Note The systematic scanning technique described below is only theoretical, considering the fact that the examination of the elbow is, for the most, focused to one quadrant only of the joint based on clinical findings. 1 ANTERIOR ELBOW For examination of the anterior elbow, the patient is seated facing the examiner with the elbow in an extension position over the table. The patient is asked to extend the elbow and supinate the fore- arm. A slight bending of the patient’s body toward the examined side makes full supination and as- sessment of the anterior compartment easier. Full elbow extension can be obtained by placing a pillow under the joint. Transverse US images are first obtained by sweeping the probe from approximately 5cm above to 5cm below the trochlea-ulna joint, a Pr perpendicular to the humeral shaft. Cranial US images of the supracondylar region reveal the superficial biceps and the deep brachialis mu- Br scles. Alongside and medial to these muscles, follow the brachial artery and the median nerve: * the nerve lies medially to the artery. * Legend: a, brachial artery; arrow, median nerve; arrowheads, distal biceps tendon; asterisks, articular cartilage of the Humerus humeral trochlea; Br, brachialis muscle; Pr, pronator muscle 2 distal biceps tendon: technique The distal biceps tendon is examined while keeping the patient’s forearm in maximal supination to bring the tendon insertion on the radial tuberosity into view. -

The Influence of Altered Lower-Extremity Kinematics on Patellofemoral Joint Dysfunction: a Theoretical Perspective
The Influence of Altered Lower-Extremity Kinematics on Patellofemoral Joint Dysfunction: A Theoretical Perspective Christopher M. Powers, PT, PhD 1 Although patellofemoral pain (PFP) is recognized as being one of the most common disorders of It has been recognized by sev- the lower extremity, treatment guidelines and underlying rationales remain vague and controver- eral authors that the patel- sial. The premise behind most treatment approaches is that PFP is the result of abnormal patellar lofemoral joint may be influenced CLINICAL COMMENTARY tracking and/or patellar malalignment. Given as such, interventions typically focus on the joint by the segmental interactions of itself and have traditionally included strengthening the vastus medialis oblique, taping, bracing, the lower extremity.6,7,21,27,34,45 Ab- soft tissue mobilization, and patellar mobilization. More recently, it has been recognized that the normal motion(s) of the tibia and patellofemoral joint and, therefore, PFP may be influenced by the interaction of the segments and femur in the transverse and frontal joints of the lower extremity. In particular, abnormal motion of the tibia and femur in the transverse and frontal planes may have an effect on patellofemoral joint mechanics. With this in planes are believed to have an mind, interventions aimed at controlling hip and pelvic motion (proximal stability) and ankle/foot effect on patellofemoral joint me- motion (distal stability) may be warranted and should be considered when treating persons with chanics and therefore PFP. An un- patellofemoral joint dysfunction. The purpose of this paper is to provide a biomechanical derstanding of how lower- overview of how altered lower-extremity mechanics may influence the patellofemoral joint. -
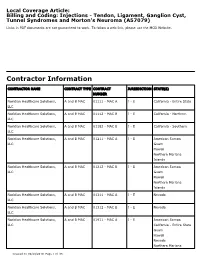
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

Closure of Patellar Tendon Defect in ACL Reconstruction
Systematic Review Closure of Patellar Tendon Defect in Anterior Cruciate Ligament Reconstruction With BoneePatellar TendoneBone Autograft: Systematic Review of Randomized Controlled Trials Rachel M. Frank, M.D., Randy Mascarenhas, M.D., Marc Haro, M.D., Nikhil N. Verma, M.D., Brian J. Cole, M.D., M.B.A., Charles A. Bush-Joseph, M.D., and Bernard R. Bach Jr., M.D. Purpose: This study aimed to systematically review the highest level of evidence on anterior cruciate ligament (ACL) reconstruction with boneepatellar tendonebone (BPTB) autografts with patellar tendon defect closure versus no closure after surgery. Methods: We performed a systematic review of multiple medical databases using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Level I and Level II randomized controlled trials comparing patellar tendon defect closure to no closure during ACL reconstruction with BPTB autografts were included. Two inde- pendent reviewers analyzed all studies. Descriptive statistics were calculated. Study methodological quality was analyzed using the Modified Coleman Methodology Score (MCMS) and Jadad scale. Results: Four studies with a combined 221 patients (154 male patients and 67 female patients) with an average age of 26.6 Æ 2.4 years (range, 17 to 54 years) were included. All studies randomized patients before surgery into ACLR with BPTB autografts either with patellar tendon defect closure or without closure. There were no differences in clinical outcomes (Lysholm score, Tegner scale, International Knee Documentation Committee [IKDC] classification, modified Larsen score, and Lauridsen rating) between groups. There were no significant differences in knee pain between groups. All studies reported imaging findings of the patellar tendon defect, with 2 studies showing no difference in appearance between groups, one study showing excessive scar formation with defect repair, and one study showing improved restoration of normal tendon appearance with defect repair. -

Morphological Characteristics of the Lateral Talocalcaneal Ligament: a Large-Scale Anatomical Study
Surgical and Radiologic Anatomy (2019) 41:25–28 https://doi.org/10.1007/s00276-018-2128-8 ANATOMIC VARIATIONS Morphological characteristics of the lateral talocalcaneal ligament: a large-scale anatomical study Mutsuaki Edama1,2 · Ikuo Kageyama2 · Takaniri Kikumoto1 · Tomoya Takabayashi1 · Takuma Inai1 · Ryo Hirabayashi1 · Wataru Ito1 · Emi Nakamura1 · Masahiro Ikezu1 · Fumiya Kaneko1 · Akira Kumazaki3 · Hiromi Inaba4 · Go Omori3 Received: 9 August 2018 / Accepted: 4 September 2018 / Published online: 30 October 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract Purpose The purpose of this study is to clarify the morphological characteristics of the lateral talocalcaneal ligament (LTCL). Methods This study examined 100 legs from 54 Japanese cadavers. The LTCL was classified into three types: Type I, the LTCL branches from the calcaneofibular ligament (CFL); Type II, the LTCL is independent of the CFL and runs parallel to the calcaneus; and Type III, the LTCL is absent. The morphological features measured were fiber bundle length, fiber bundle width, and fiber bundle thickness. Results The LTCL was classified as Type I in 18 feet (18%), Type II in 24 feet (24%), and Type III in 58 feet (58%). All LTCLs were associated with the anterior talofibular ligament at the talus. There was no significant difference in morphologi- cal characteristics by Type for each ligament. Conclusions The LTCL was similar to the CFL in terms of fiber bundle width and fiber bundle thickness. Keywords Calcaneofibular · Ligament · Subtalar joint · Gross anatomy Introduction features, as well as complex three-dimensional mobility, making it a challenge to conduct quantitative evaluations. Of patients with chronic ankle instability, 42% [6] present Ligaments that are associated with the stability of the with mechanical instability of the talocrural joint, and 58% subtalar joint include the calcaneofibular ligament (CFL), have mechanical instability of the subtalar joint [3], each of the lateral talocalcaneal ligament (LTCL), the interosseous them at high percentages. -

Physical Examination of the Knee: Meniscus, Cartilage, and Patellofemoral Conditions
Review Article Physical Examination of the Knee: Meniscus, Cartilage, and Patellofemoral Conditions Abstract Robert D. Bronstein, MD The knee is one of the most commonly injured joints in the body. Its Joseph C. Schaffer, MD superficial anatomy enables diagnosis of the injury through a thorough history and physical examination. Examination techniques for the knee described decades ago are still useful, as are more recently developed tests. Proper use of these techniques requires understanding of the anatomy and biomechanical principles of the knee as well as the pathophysiology of the injuries, including tears to the menisci and extensor mechanism, patellofemoral conditions, and osteochondritis dissecans. Nevertheless, the clinical validity and accuracy of the diagnostic tests vary. Advanced imaging studies may be useful adjuncts. ecause of its location and func- We have previously described the Btion, the knee is one of the most ligamentous examination.1 frequently injured joints in the body. Diagnosis of an injury General Examination requires a thorough knowledge of the anatomy and biomechanics of When a patient reports a knee injury, the joint. Many of the tests cur- the clinician should first obtain a rently used to help diagnose the good history. The location of the pain injured structures of the knee and any mechanical symptoms were developed before the avail- should be elicited, along with the ability of advanced imaging. How- mechanism of injury. From these From the Division of Sports Medicine, ever, several of these examinations descriptions, the structures that may Department of Orthopaedics, are as accurate or, in some cases, University of Rochester School of have been stressed or compressed can Medicine and Dentistry, Rochester, more accurate than state-of-the-art be determined and a differential NY. -

Patellar Tendinopathy: Some Aspects of Basic Science and Clinical Management
346 Br J Sports Med 1998;32:346–355 Br J Sports Med: first published as 10.1136/bjsm.32.4.346 on 1 December 1998. Downloaded from OCCASIONAL PIECE Patellar tendinopathy: some aspects of basic science and clinical management School of Human Kinetics, University of K M Khan, N MaVulli, B D Coleman, J L Cook, J E Taunton British Columbia, Vancouver, Canada K M Khan J E Taunton Tendon injuries account for a substantial tendinopathy, and the remainder to tendon or Victorian Institute of proportion of overuse injuries in sports.1–6 tendon structure in general. Sport Tendon Study Despite the morbidity associated with patellar Group, Melbourne, tendinopathy in athletes, management is far Victoria, Australia 7 Anatomy K M Khan from scientifically based. After highlighting The patellar tendon, the extension of the com- J L Cook some aspects of clinically relevant basic sci- mon tendon of insertion of the quadriceps ence, we aim to (a) review studies of patellar femoris muscle, extends from the inferior pole Department of tendon pathology that explain why the condi- of the patella to the tibial tuberosity. It is about Orthopaedic Surgery, tion can become chronic, (b) summarise the University of Aberdeen 3 cm wide in the coronal plane and 4 to 5 mm Medical School, clinical features and describe recent advances deep in the sagittal plane. Macroscopically it Aberdeen, Scotland, in the investigation of this condition, and (c) appears glistening, stringy, and white. United Kingdom outline conservative and surgical treatment NMaVulli options. BLOOD SUPPLY Department of The blood supply has been postulated to con- 89 Medicine, University tribute to patellar tendinopathy. -

Advice and Exercises for Patients with Plantar Fasciitis
Advice and exercises for patients with plantar fasciitis This leaflet provides management advice and exercises for people diagnosed with plantar fasciitis, a condition causing pain in the heel, sole and /or arch of the foot. Structures of the foot The plantar fascia is a sheet or broad band of fibrous tissue that runs along the bottom of the foot. This tissue connects the heel to the base of the toes. Under normal circumstances, the plantar fascia supports the arch of the foot and acts as a shock absorbing “bow string” within the arch of the foot. With weight bearing, the foot flattens and the plantar fascia stretches, then springing you forward ready for the next step. While walking, the stresses placed on the foot can be one and a quarter times your body weight (this increases to two and three quarter times your body weight when running). Unsurprisingly then, that heel pain is common. If tension on this “bowstring” becomes too great, irritation or inflammation can occur causing pain. What is plantar fasciitis? Plantar fasciitis is a relatively common foot problem affecting up to 10-15% of the population. It can occur at any age. It is sometimes known as “policeman’s heel”. When placed under too much stress due to abnormal loading, the plantar fascia stretches causing micro tearing and degeneration of the tissue. It can lead to pain in the heel, across the sole of the foot and sometimes into the arch area of the foot too. These micro tears repair with scar tissue, which is less flexible than the fascia and can cause the problem to persist for many months. -

Plantar Fasciitis Exercises
Accurate Clinic 2401 Veterans Memorial Blvd. Suite16 Kenner, LA 70062 - 4799 Phone: 504.472.6130 Fax: 504.472.6128 www.AccurateClinic.com Plantar Fasciitis Exercise Getting the right plantar fasciitis exercise is imperative to ensure the injury doesn’t continue to affect performance. If not given the attention it needs, plantar fasciitis can flair up long after an athlete thinks they’ve recovered and badly damage training plans and competition aspirations. What is plantar fascia? Plantar fascia is a thick, fibrous band of connective tissue which originates at the heel bone and runs along the bottom of the foot in a fan-like manner, attaching to the base of each of the toes. A rather tough, resilient structure, the plantar fascia takes on a number of critical functions during running and walking. Although the fascia is invested with countless sturdy 'cables' of connective tissue called collagen fibres, it is certainly not immune to injury. In fact, about 5 to 10 per cent of all running injuries are inflammations of the fascia, an incidence rate which in the United States would produce about a million cases of plantar fasciitis per year, just among runners and joggers. Basketball players, tennis players, volleyballers, step-aerobics participants, and dancers are also prone to plantar problems, as are non-athletic people who spend a lot of time on their feet or suddenly become active after a long period of lethargy. Why does the fascia flare up? Although it is a fairly rugged structure, the plantar fascia is not very receptive to stretching, and yet stretching occurs in the fascia nearly every time the foot hits the ground. -

Ankle Fusion Protocol
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -

SUBTALAR JOINT RECONSTRUCTION by George E
SUBTALAR JOINT RECONSTRUCTION By George E. Quill, Jr., M.D. The single axis subtalar joint is a hinge joining the talus and calcaneus that allows adaptation of the foot on uneven ground. This joint modifies the forces of ambulation imposed on the rest of the skeleton and influences the performance of the more distal foot articulations as well. When the structure and function of this joint are altered by trauma, instability, arthritis, infection, or tarsal coalition, subtalar reconstruction, usually in the form of arthrodesis, may prove to be a very successful procedure in treating the patient's resultant disability. The subtalar joint is, in this author's opinion, a very under appreciated joint. Even though it is estimated that up to 3 percent of the general population may have an asymptomatic talocalcaneal coalition present from a very young age and function very well, patients with a stiffened subtalar joint secondary to post-traumatic subtalar osteoarthrosis have very poor biomechanical function. Many patients presenting with "ankle " pain or who have pain from an ankle sprain that "just won't go away", may actually have subtalar pathology as an etiology for their discomfort. It is the astute orthopaedic surgeon who can recognize and successfully treat this pathology. Subtalar arthrodesis performed for the appropriate indications has proven to be one of this author's most gratifying, time-tested procedures in alleviating pain and improving function in patients so affected. Therefore, it is prudent that we understand the anatomic and functional aspects of the subtalar joint. The subtalar joint consists of three separate facets for articulation between the talus and calcaneus (Figure 1).