The Impact of Chromosomal Translocation Locus and Fusion Oncogene Coding Sequence in Synovial Sarcomagenesis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Expression of ALK1 and P80 in Inflammatory Myofibroblastic Tumor and Its Mesenchymal Mimics: a Study of 135 Cases Melissa H
Expression of ALK1 and p80 in Inflammatory Myofibroblastic Tumor and Its Mesenchymal Mimics: A Study of 135 Cases Melissa H. Cessna, M.D., Holly Zhou, M.D., Warren G. Sanger, Ph.D., Sherrie L. Perkins, M.D., Ph.D., Sheryl Tripp, M.T., Diane Pickering, M.S., Clark Daines, M.D., Cheryl M. Coffin, M.D. Department of Pathology, Primary Children’s Medical Center and University of Utah School of Medicine, Salt Lake City, Utah (MHC, HZ, SLP, ST, CD, CMC); and Department of Pediatrics, University of Nebraska Medical Center, Omaha, Nebraska (WGS, DP) between structural abnormalities involving 2p23 or Abnormalities of chromosome 2p23 with expres- additional copies of 2p23, it supports the concept of sion of ALK1 and p80 occur in both inflammatory ALK involvement in a larger group of neoplasms, myofibroblastic tumor (IMT) and anaplastic large some of which have other documented clonal ab- cell lymphoma. This immunohistochemical study normalities. In IMT, immunohistochemistry for investigates whether the ALK family of neoplasms ALK1 and p80 is useful as an indicator of a 2p23 includes fibroblastic–myofibroblastic, myogenic, abnormality, but it must be interpreted in the con- and spindle cell tumors. Formalin-fixed paraffin- text of histologic and other clinicopathologic data if embedded archival tissues from 10 IMTs and 125 used as an adjunct to differential diagnosis. other soft tissue tumors were stained for ALK1 and p80 with standard immunohistochemistry. ALK1 KEY WORDS: ALK gene rearrangements, ALK im- and/or p80 reactivity was observed in a cytoplasmic munohistochemistry, Anaplastic large cell lym- pattern in IMT (4/10; 40%), malignant peripheral phoma, Inflammatory myofibroblastic tumor. -

SSX2IP Antibody Cat
SSX2IP Antibody Cat. No.: 46-435 SSX2IP Antibody Specifications HOST SPECIES: Goat SPECIES REACTIVITY: Human HOMOLOGY: Expected Species Reactivity based on sequence homology: Dog IMMUNOGEN: The immunogen for this antibody is: C-SYTNSHVEKDDLP TESTED APPLICATIONS: ELISA, ICC, IF Peptide ELISA: antibody detection limit dilution 1:16000.Western Blot:We find no specific signal but low background (at antibody concentration up to 1ug/ml) in lysates of cell line APPLICATIONS: K562.Immunocytochemsitry/Immunofluorescence: This product has been successfully used in ICC/IF on K562 cell line. Properties Purified from goat serum by ammonium sulphate precipitation followed by antigen PURIFICATION: affinity chromatography using the immunizing peptide. CLONALITY: Polyclonal CONJUGATE: Unconjugated PHYSICAL STATE: Liquid September 30, 2021 1 https://www.prosci-inc.com/ssx2ip-antibody-46-435.html Supplied at 0.5 mg/ml in Tris saline, 0.02% sodium azide, pH7.3 with 0.5% bovine serum BUFFER: albumin. Aliquot and store at -20°C. Minimize freezing and thawing. CONCENTRATION: 500 ug/mL STORAGE CONDITIONS: Aliquot and store at -20˚C. Minimize freezing and thawing. Additional Info OFFICIAL SYMBOL: SSX2IP SSX2IP, ADIP, KIAA0923, synovial sarcoma, X breakpoint 2 interacting protein, afadin- and ALTERNATE NAMES: alpha-actinin-binding protein, FLJ10848, MGC75026 ACCESSION NO.: NP_054740.2 PROTEIN GI NO.: 41281571 GENE ID: 117178 Background and References 1) de Bruijn DR, dos Santos NR, Kater-Baats E, Thijssen J, van den Berk L, Stap J, Balemans M, Schepens M, Merkx G, van Kessel AG. The cancer-related protein SSX2 interacts with REFERENCES: the human homologue of a Ras-like GTPase interactor, RAB3IP, and a novel nuclear protein, SSX2IP. -

SS18 (SYT) (18Q11) Gene Rearrangement by FISH Indications for Ordering Genetics
SS18 (SYT) (18q11) Gene Rearrangement by FISH Indications for Ordering Genetics Diagnosis of synovial sarcoma in conjunction with histologic Translocations – SS18-SSX1, SS18-SSX2 and clinical information Structure/function Test Description • SS18 is located on chromosome 18 • SSX1 and SSX2 are located on the X-chromosome Fluorescence in situ hybridization • Each gene in the translocation codes for proteins that have opposite transcriptional functions Tests to Consider o SS18 – activator of oncogenes Primary test o SSX1, SSX2 – tumor suppression SS18 (SYT) (18q11) Gene Rearrangement by FISH 3001303 Test Interpretation • Molecular diagnosis of synovial sarcoma Results Related test • Positive – SS18 rearrangement is detected Chromosome FISH, Interphase 2002298 o SSX translocation partner is not identified with this • Specific probe for SS18 (SYT) rearrangement must be testing methodology requested o Synovial sarcoma likely • Fresh tissue specimens only • Negative – no SS18 rearrangement detected Disease Overview o Does not entirely exclude the presence of an SS18 rearrangement as some translocations are cryptic and Incidence – rare not evaluable by this testing methodology • Synovial sarcomas account for 8-10% of all soft tissue o Does not entirely exclude diagnosis of synovial sarcoma sarcomas Limitations Diagnostic/prognostic issues • Testing using tissue fixed in alcohol-based or non-formalin • Synovial sarcomas may resemble other neoplasms, fixatives has not been validated using this method particularly those displaying an epithelioid, spindle cell, or • SS18 fusion partners are not detected with this test combined morphology • t(X;18)(p11.2;q11.2) translocation serves as a specific marker for synovial sarcoma o SS18 (SYT) gene fuses with SSX gene . Fusion with SSX1 in ~65% of synovial sarcomas . -
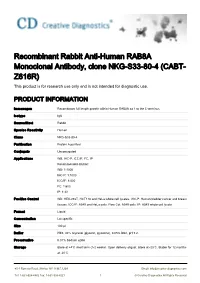
Recombinant Rabbit Anti-Human RAB8A Monoclonal Antibody, Clone NKG-S33-80-4 (CABT- Z616R) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Recombinant Rabbit Anti-Human RAB8A Monoclonal Antibody, clone NKG-S33-80-4 (CABT- Z616R) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Immunogen Recombinant full length protein within Human RAB8A aa 1 to the C-terminus. Isotype IgG Source/Host Rabbit Species Reactivity Human Clone NKG-S33-80-4 Purification Protein A purified Conjugate Unconjugated Applications WB, IHC-P, ICC/IF, FC, IP Recommended dilution: WB: 1:1000 IHC-P: 1:1000 ICC/IF: 1:500 FC: 1:600 IP: 1:30 Positive Control WB: HEK-293T, HCT116 and HeLa whole cell lysates. IHC-P: Human bladder cancer and breast tissues. ICC/IF: A549 and HeLa cells. Flow Cyt: A549 cells. IP: A549 whole cell lysate. Format Liquid Concentration Lot specific Size 100 μl Buffer PBS, 40% Glycerol (glycerin, glycerine), 0.05% BSA, pH 7.2. Preservative 0.01% Sodium azide Storage Store at +4℃ short term (1-2 weeks). Upon delivery aliquot. Store at -20℃. Stable for 12 months at -20℃. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Ship Wet ice Warnings This product is for research use only and is not intended for diagnostic use. BACKGROUND Introduction RAB8A may be involved in vesicular trafficking and neurotransmitter release. Together with RAB11A, RAB3IP, the exocyst complex, PARD3, PRKCI, ANXA2, CDC42 and DNMBP promotes transcytosis of PODXL to the apical membrane initiation sites (AMIS), apical surface formation and lumenogenesis. Together with MYO5B and RAB11A participates in epithelial cell polarization. -

Gene Section Short Communication
Atlas of Genetics and Cytogenetics in Oncology and Haematology OPEN ACCESS JOURNAL INIST -CNRS Gene Section Short Communication SSX2IP (synovial sarcoma, X breakpoint 2 interacting protein) Ghazala Khan, Barbara Guinn University of Bedfordshire, Division of Science, Park Square, Luton, Bedfordshire, UK (GK), University of Bedfordshire, Division of Science, Park Square, Luton, Bedfordshire, UK; Cancer Sciences Unit, University of Southampton, Southampton, UK; Department of Haematological Medicine, Kings College, London, UK (BG) Published in Atlas Database: March 2012 Online updated version : http://AtlasGeneticsOncology.org/Genes/SSX2IPID42407ch1p22.html DOI: 10.4267/2042/47489 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 2.0 France Licence. © 2012 Atlas of Genetics and Cytogenetics in Oncology and Haematology exons however the first one is not translated (de Bruijn Identity et al., 2002). Other names: ADIP Transcription HGNC (Hugo): SSX2IP The gene contains 33 introns. 18 different mRNAs are Location: 1p22.3 produced; 17 spliced and 1 un-spliced form (Thierry- Note Mieg and Thierry-Mieg, 2006). SSX2IP gene encodes the protein SSX2IP which Pseudogene interacts with the cancer-testis antigen SSX2. It is A pseudogene of this gene is found on chromosome 3 thought that SSX2IP regulates the function of SSX2 in (provided by RefSeq, Oct 2009 from Entrez Gene). the testes and malignant cells. The rodent equivalent is known as afadin DIL domain-interacting protein (ADIP) and the chicken orthologue is called clock- Protein controlled gene (LCG) (Breslin et al., 2007). Note SSX2IP was discovered due to its interaction with DNA/RNA SSX2 in a yeast two-hybrid system and believed to regulate the function of SSX2 in the testes and Note malignant cells (de Bruijn et al., 2002). -

Open Dogan Phdthesis Final.Pdf
The Pennsylvania State University The Graduate School Eberly College of Science ELUCIDATING BIOLOGICAL FUNCTION OF GENOMIC DNA WITH ROBUST SIGNALS OF BIOCHEMICAL ACTIVITY: INTEGRATIVE GENOME-WIDE STUDIES OF ENHANCERS A Dissertation in Biochemistry, Microbiology and Molecular Biology by Nergiz Dogan © 2014 Nergiz Dogan Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy August 2014 ii The dissertation of Nergiz Dogan was reviewed and approved* by the following: Ross C. Hardison T. Ming Chu Professor of Biochemistry and Molecular Biology Dissertation Advisor Chair of Committee David S. Gilmour Professor of Molecular and Cell Biology Anton Nekrutenko Professor of Biochemistry and Molecular Biology Robert F. Paulson Professor of Veterinary and Biomedical Sciences Philip Reno Assistant Professor of Antropology Scott B. Selleck Professor and Head of the Department of Biochemistry and Molecular Biology *Signatures are on file in the Graduate School iii ABSTRACT Genome-wide measurements of epigenetic features such as histone modifications, occupancy by transcription factors and coactivators provide the opportunity to understand more globally how genes are regulated. While much effort is being put into integrating the marks from various combinations of features, the contribution of each feature to accuracy of enhancer prediction is not known. We began with predictions of 4,915 candidate erythroid enhancers based on genomic occupancy by TAL1, a key hematopoietic transcription factor that is strongly associated with gene induction in erythroid cells. Seventy of these DNA segments occupied by TAL1 (TAL1 OSs) were tested by transient transfections of cultured hematopoietic cells, and 56% of these were active as enhancers. Sixty-six TAL1 OSs were evaluated in transgenic mouse embryos, and 65% of these were active enhancers in various tissues. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

The Impact of Chromosomal Translocation Locus and Fusion Oncogene Coding Sequence in Synovial Sarcomagenesis
Oncogene (2016) 35, 5021–5032 © 2016 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-9232/16 www.nature.com/onc ORIGINAL ARTICLE The impact of chromosomal translocation locus and fusion oncogene coding sequence in synovial sarcomagenesis KB Jones1,2,3, JJ Barrott1,2,3, M Xie4, M Haldar5, H Jin1,2,3, J-F Zhu1,2,3, MJ Monument1,3, TL Mosbruger3,6, EM Langer5, RL Randall1,3, RK Wilson4,7,8,9, BR Cairns2,3,10, L Ding4,7,8,9 and MR Capecchi5 Synovial sarcomas are aggressive soft-tissue malignancies that express chromosomal translocation-generated fusion genes, SS18-SSX1 or SS18-SSX2 in most cases. Here, we report a mouse sarcoma model expressing SS18-SSX1, complementing our prior model expressing SS18-SSX2. Exome sequencing identified no recurrent secondary mutations in tumors of either genotype. Most of the few mutations identified in single tumors were present in genes that were minimally or not expressed in any of the tumors. Chromosome 6, either entirely or around the fusion gene expression locus, demonstrated a copy number gain in a majority of tumors of both genotypes. Thus, by fusion oncogene coding sequence alone, SS18-SSX1 and SS18-SSX2 can each drive comparable synovial sarcomagenesis, independent from other genetic drivers. SS18-SSX1 and SS18-SSX2 tumor transcriptomes demonstrated very few consistent differences overall. In direct tumorigenesis comparisons, SS18-SSX2 was slightly more sarcomagenic than SS18-SSX1, but equivalent in its generation of biphasic histologic features. Meta-analysis of human synovial sarcoma patient series identified two tumor–gentoype–phenotype correlations that were not modeled by the mice, namely a scarcity of male hosts and biphasic histologic features among SS18-SSX2 tumors. -

SYT-SSX1 and SYT-SSX2 Interfere with Repression of E-Cadherin by Snail and Slug
Research Article SYT-SSX1 and SYT-SSX2 Interfere with Repression of E-Cadherin by Snail and Slug: A Potential Mechanism for Aberrant Mesenchymal to Epithelial Transition in Human Synovial Sarcoma Tsuyoshi Saito, Makoto Nagai, and Marc Ladanyi Department of Pathology, Memorial Sloan-Kettering Cancer Center, New York, New York Abstract open spaces [i.e., glandular epithelial differentiation (GED)] in a Synovial sarcoma is a primitive mesenchymal neoplasm background of spindle cells (Supplementary Fig. S1). Both the characterized in almost all cases by a t(X;18) fusing the SYT spindle and epithelial elements of synovial sarcoma contain transcriptional coactivator gene with either SSX1 or SSX2, the t(X;18) and are thus clonally related (2, 3). The GED in synovial with the resulting fusion gene encoding an aberrant tran- sarcoma has the hallmarks of a genuine mesenchymal to epithelial scriptional regulator.A subset of synovial sarcoma, predom- transition (MET) akin to those seen in embryonic development inantly cases with the SYT-SSX1 fusion, shows foci of (e.g., in developing kidney). Thus, the epithelial cells in synovial h morphologic epithelial differentiation in the form of nests of sarcoma express E-cadherin, keratins, a-catenin, -catenin, and glandular epithelium.The striking spontaneous mesenchymal g-catenin, whereas the spindle cells express vimentin and, focally, to epithelial differentiation in this cancer is reminiscent of a N-cadherin (4, 5). Epithelial differentiation in synovial sarcoma is developmental switch, but the only -

A Novel Type of SYT/SSX Fusion
A Novel Type of SYT/SSX Fusion: Methodological and Biological Implications Maria Törnkvist, M.Sc., Bertha Brodin, Ph.D., Armando Bartolazzi, M.D., Ph.D., Olle Larsson, M.D., Ph.D. Department of Cellular and Molecular Tumor Pathology, Cancer Centrum Karolinska, Karolinska Hospital (MT, BB, AB, OL), Stockholm, Sweden; and Department of Pathology, Regina Elena Cancer Institute (AB), Rome, Italy the presence of SYT/SSX transcripts in two cases Synovial sarcoma (SS) is a rare soft-tissue tumor using the proposed RT-PCR approach. Applications that affects children and young adults. It is charac- of optimized RT-PCR can contribute to reduce false- terized by the chromosomal translocation t(X; negative SYT/SSX SS cases reported in literature. 18)(p11.2;q11.2), which results in the fusion of the SYT gene on chromosome 18 with a SSX gene on KEY WORDS: RT-PCR, Synovial sarcoma, SYT/SSX chromosome X. In the majority of cases, SYT is fusion gene, SYT/SSX variants. fused to exon 5 of SSX1 (64%), SSX2 (36%), or, Mod Pathol 2002;15(6):679–685 rarely, SSX4. A novel fusion transcript variant deriv- ing from the fusion of SYT to exon 6 of SSX4 gene Synovial sarcomas (SS) account for 7 to 10% of all (SYT/SSX4v) was found coexpressed in one of the human soft-tissue sarcomas and are mainly located previously reported SYT/SSX4 cases. In the present in the extremities in the vicinity of large joints (1). investigation, we describe a new SS case that was Depending on histomorphological appearance, SSs previously shown to be negative for SYT/SSX1 and are usually subdivided into two major forms, bipha- SYT/SSX2 expression by conventional reverse tran- sic and monophasic. -

Radiation-Associated Synovial Sarcoma
Radiation-Associated Synovial Sarcoma: Clinicopathologic and Molecular Analysis of Two Cases Jean-François Egger, M.D., Jean-Michel Coindre, M.D., Jean Benhattar, Ph.D., Philippe Coucke, M.D., Louis Guillou, M.D. University Institute of Pathology (J-FE, JB, LG) and Department of Radiooncology, University Hospital (PC), Lausanne, Switzerland; Bergonié Institute and University of Bordeaux II (J-MC), Bordeaux, France region, or viscera (1, 2). SS bears the t(X;18) (SYT- Development of a soft-tissue sarcoma is an infre- SSX) reciprocal translocation that seems to be spe- quent but well-known long-term complication of cific for this tumor type and can be routinely de- radiotherapy. Malignant fibrous histiocytomas, ex- tected in paraffin-embedded tissue using the traskeletal osteosarcomas, fibrosarcomas, malig- reverse transcriptase–polymerase chain reaction nant peripheral nerve sheath tumors, and angiosar- (RT-PCR; 3–6). Radiation-associated sarcomas are comas are most frequently encountered. Radiation- an infrequent but well-known long-term complica- associated synovial sarcomas are exceptional. We tion of radiotherapy (7–16). They occur in about report the clinicopathologic, immunohistochemi- 1/1000 patients who have undergone radiation cal, and molecular features of two radiation- therapy (7–11). Radiation-associated sarcomas are associated synovial sarcomas. One tumor developed defined as sarcomas arising in a previously irradi- in a 42-year-old female 17 years after external irra- ated field after a latency period of Ն2 years (12). diation was given for breast carcinoma; the other They usually show a more aggressive clinical course occurred in a 34-year-old female who was irradiated associated with shortened patient survival as com- at the age of 7 years for a nonneoplastic condition of pared with sporadic sarcomas (9–12, 14).