Resolution of Bilateral Ptosis After Reduction of Unilaterally Elevated Intraocular Pressure in a Child with Axenfeld-Reiger Spectrum Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Corneal Ectasia
Corneal Ectasia Secretary for Quality of Care Anne L. Coleman, MD, PhD Academy Staff Nicholas P. Emptage, MAE Nancy Collins, RN, MPH Doris Mizuiri Jessica Ravetto Flora C. Lum, MD Medical Editor: Susan Garratt Design: Socorro Soberano Approved by: Board of Trustees September 21, 2013 Copyright © 2013 American Academy of Ophthalmology® All rights reserved AMERICAN ACADEMY OF OPHTHALMOLOGY and PREFERRED PRACTICE PATTERN are registered trademarks of the American Academy of Ophthalmology. All other trademarks are the property of their respective owners. This document should be cited as follows: American Academy of Ophthalmology Cornea/External Disease Panel. Preferred Practice Pattern® Guidelines. Corneal Ectasia. San Francisco, CA: American Academy of Ophthalmology; 2013. Available at: www.aao.org/ppp. Preferred Practice Pattern® guidelines are developed by the Academy’s H. Dunbar Hoskins Jr., MD Center for Quality Eye Care without any external financial support. Authors and reviewers of the guidelines are volunteers and do not receive any financial compensation for their contributions to the documents. The guidelines are externally reviewed by experts and stakeholders before publication. Corneal Ectasia PPP CORNEA/EXTERNAL DISEASE PREFERRED PRACTICE PATTERN DEVELOPMENT PROCESS AND PARTICIPANTS The Cornea/External Disease Preferred Practice Pattern® Panel members wrote the Corneal Ectasia Preferred Practice Pattern® guidelines (“PPP”). The PPP Panel members discussed and reviewed successive drafts of the document, meeting in person twice and conducting other review by e-mail discussion, to develop a consensus over the final version of the document. Cornea/External Disease Preferred Practice Pattern Panel 2012–2013 Robert S. Feder, MD, Co-chair Stephen D. McLeod, MD, Co-chair Esen K. -

Albinism Terminology
Albinism Terminology Oculocutaneous Albinism (OCA): Oculocutaneous (pronounced ock-you-low-kew- TAIN-ee-us) Albinism is an inherited genetic condition characterized by the lack of or diminished pigment in the hair, skin, and eyes. Implications of this condition include eye and skin sensitivities to light and visual impairment. Ocular Albinism (OA): Ocular Albinism is an inherited genetic condition, diagnosed predominantly in males, characterized by the lack of pigment in the eyes. Implications of this condition include eye sensitivities to light and visual impairment. Hermansky Pudlak Syndrome (HPS): Hermansky-Pudlak Syndrome is a type of albinism which includes a bleeding tendency and lung disease. HPS may also include inflammatory bowel disease or kidney disease. The severity of these problems varies much from person to person, and the condition can be difficult to diagnose with traditional blood tests Chediak Higashi Syndrome: Chediak Higashi Syndrome is a type of albinism in which the immune system is affected. Illnesses and infections are common from infancy and can be severe. Issues also arise with blood clotting and severe bleeding. Melanin: Melanin is pigment found in a group of cells called melanocytes in most organisms. In albinism, the production of melanin is impaired or completely lacking. Nystagmus: Nystagmus is an involuntary movement of the eyes in either a vertical, horizontal, pendular, or circular pattern caused by a problem with the visual pathway from the eye to the brain. As a result, both eyes are unable to hold steady on objects being viewed. Nystagmus may be accompanied by unusual head positions and head nodding in an attempt to compensate for the condition. -

Partial Albinism (Heterochromia Irides) in Black Angus Cattle
Partial Albinism (Heterochromia irides) in Black Angus Cattle C. A. Strasia, Ph.D.1 2 J. L. Johnson, D. V.M., Ph.D.3 D. Cole, D. V.M.4 H. W. Leipold, D.M.V., Ph.D.5 Introduction Various types of albinism have been reported in many Pathological changes in ocular anomalies of incomplete breeds of cattle throughout the world.4 We describe in this albino cattle showed iridal heterochromia grossly. paper a new coat and eye color defect (partial albinism, Histopathological findings of irides showed only the heterochromia irides) in purebred Black Angus cattle. In posterior layer fairly pigmented and usually no pigment in addition, the results of a breeding trial using a homozygous the stroma nor the anterior layer. The ciliary body showed affected bull on normal Hereford cows are reported. reduced amount of pigmentation and absence of corpora Albinism has been described in a number of breeds of nigra. Choroid lacked pigmentation. The Retina showed cattle.1,3-8,12,16,17 An albino herd from Holstein parentage disorganization. Fundus anomalies included colobomata of was described and no pigment was evident in the skin, eyes, varying sizes at the ventral aspect of the optic disc and the horns, and hooves; in addition, the cattle exhibited photo tapetum fibrosum was hypoplastic.12 In albino humans, the phobia. A heifer of black pied parentage exhibited a fundus is depigmented and the choroidal vessels stand out complete lack of pigment in the skin, iris and hair; however, strikingly. Nystagmus, head nodding and impaired vision at sexual maturity some pigment was present and referred to also may occur. -
Wavelength of Light and Photophobia in Inherited Retinal Dystrophy
www.nature.com/scientificreports OPEN Wavelength of light and photophobia in inherited retinal dystrophy Yuki Otsuka1, Akio Oishi1,2*, Manabu Miyata1, Maho Oishi1, Tomoko Hasegawa1, Shogo Numa1, Hanako Ohashi Ikeda1 & Akitaka Tsujikawa1 Inherited retinal dystrophy (IRD) patients often experience photophobia. However, its mechanism has not been elucidated. This study aimed to investigate the main wavelength of light causing photophobia in IRD and diference among patients with diferent phenotypes. Forty-seven retinitis pigmentosa (RP) and 22 cone-rod dystrophy (CRD) patients were prospectively recruited. We designed two tinted glasses: short wavelength fltering (SWF) glasses and middle wavelength fltering (MWF) glasses. We classifed photophobia into three types: (A) white out, (B) bright glare, and (C) ocular pain. Patients were asked to assign scores between one (not at all) and fve (totally applicable) for each symptom with and without glasses. In patients with RP, photophobia was better relieved with SWF glasses {“white out” (p < 0.01) and “ocular pain” (p = 0.013)}. In CRD patients, there was no signifcant diference in the improvement wearing two glasses (p = 0.247–1.0). All RP patients who preferred MWF glasses had Bull’s eye maculopathy. Meanwhile, only 15% of patients who preferred SWF glasses had the fnding (p < 0.001). Photophobia is primarily caused by short wavelength light in many patients with IRD. However, the wavelength responsible for photophobia vary depending on the disease and probably vary according to the pathological condition. Inherited retinal degenerations (IRDs) represent a diverse group of diseases characterized by progressive photo- receptor cell death that can lead to blindness 1. -

Congenital Ocular Anomalies in Newborns: a Practical Atlas
www.jpnim.com Open Access eISSN: 2281-0692 Journal of Pediatric and Neonatal Individualized Medicine 2020;9(2):e090207 doi: 10.7363/090207 Received: 2019 Jul 19; revised: 2019 Jul 23; accepted: 2019 Jul 24; published online: 2020 Sept 04 Mini Atlas Congenital ocular anomalies in newborns: a practical atlas Federico Mecarini1, Vassilios Fanos1,2, Giangiorgio Crisponi1 1Neonatal Intensive Care Unit, Azienda Ospedaliero-Universitaria Cagliari, University of Cagliari, Cagliari, Italy 2Department of Surgery, University of Cagliari, Cagliari, Italy Abstract All newborns should be examined for ocular structural abnormalities, an essential part of the newborn assessment. Early detection of congenital ocular disorders is important to begin appropriate medical or surgical therapy and to prevent visual problems and blindness, which could deeply affect a child’s life. The present review aims to describe the main congenital ocular anomalies in newborns and provide images in order to help the physician in current clinical practice. Keywords Congenital ocular anomalies, newborn, anophthalmia, microphthalmia, aniridia, iris coloboma, glaucoma, blepharoptosis, epibulbar dermoids, eyelid haemangioma, hypertelorism, hypotelorism, ankyloblepharon filiforme adnatum, dacryocystitis, dacryostenosis, blepharophimosis, chemosis, blue sclera, corneal opacity. Corresponding author Federico Mecarini, MD, Neonatal Intensive Care Unit, Azienda Ospedaliero-Universitaria Cagliari, University of Cagliari, Cagliari, Italy; tel.: (+39) 3298343193; e-mail: [email protected]. -

Eleventh Edition
SUPPLEMENT TO April 15, 2009 A JOBSON PUBLICATION www.revoptom.com Eleventh Edition Joseph W. Sowka, O.D., FAAO, Dipl. Andrew S. Gurwood, O.D., FAAO, Dipl. Alan G. Kabat, O.D., FAAO Supported by an unrestricted grant from Alcon, Inc. 001_ro0409_handbook 4/2/09 9:42 AM Page 4 TABLE OF CONTENTS Eyelids & Adnexa Conjunctiva & Sclera Cornea Uvea & Glaucoma Viitreous & Retiina Neuro-Ophthalmic Disease Oculosystemic Disease EYELIDS & ADNEXA VITREOUS & RETINA Blow-Out Fracture................................................ 6 Asteroid Hyalosis ................................................33 Acquired Ptosis ................................................... 7 Retinal Arterial Macroaneurysm............................34 Acquired Entropion ............................................. 9 Retinal Emboli.....................................................36 Verruca & Papilloma............................................11 Hypertensive Retinopathy.....................................37 Idiopathic Juxtafoveal Retinal Telangiectasia...........39 CONJUNCTIVA & SCLERA Ocular Ischemic Syndrome...................................40 Scleral Melt ........................................................13 Retinal Artery Occlusion ......................................42 Giant Papillary Conjunctivitis................................14 Conjunctival Lymphoma .......................................15 NEURO-OPHTHALMIC DISEASE Blue Sclera .........................................................17 Dorsal Midbrain Syndrome ..................................45 -

An Operation for Congenital Ptosis by George Young
Br J Ophthalmol: first published as 10.1136/bjo.8.6.272 on 1 June 1924. Downloaded from 272 THE BRITISH JOURNAL OF OPHTHALMIOI,OGY added plus lenses (eye being under atropin), J.2, fluently. This made her left eye equal, for distance, to her better eye, which is now getting worse owing to increased bulging, and will probably follow the course of the other one soon. R.V.: 6/36, c. -1.OD sph. + 3.50D cyl. 1550: 6/24 and J.5. Furthermore, it may be noted that the intraocular tension was now normal on the side of the iridectomy, while the right eye was hard, and I submitted it again to pilocarpin and bandage at night. I sent her home for a fortnight to feed up, take malt and cod liver oil and fats, and to take plenty of rest and recuperate. On July 8 the final result was: L.V.: 6/36, c.-5.OD sph. +3.50D cyl. 1600: 6/12 full, and -3.OD sph. and +3.50D cyl. J.2. Soon I shall tattoo the stellate leucoma with an artificial pupil. May 10, 1924. Since writing the above, some ten months ago, affairs have kept steady. There is no bulging of the left cornea or scar. I attempted tattooing at two sittings, and have considerably diminished the glare of the scar, but I refrain from risking the deep tattooing necessary for securing an imitation round black pupil, fearing to do harm. Glasses were prescribed and worn with comfort and great help, the vision being maintained as above. -

What Is Hermansky-Pudlak Syndrome?
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What is Hermansky-Pudlak Syndrome? Hermansky-Pudlak Syndrome (HPS) is a rare inherited disease, named after two doctors in Czechoslovakia who, in 1959, recognized similar health conditions in two unrelated adults. Since the discovery of HPS, the condition has occurred all over the world but is most often seen in Puerto Rico. The most common health conditions with HPS are albinism, the tendency to Journal of Hematology bleed easily, and pulmonary fibrosis. A Figure 1. Normal platelet with dense bodies growing number of gene mutations have visualized by electron microscopy. been identified causing HPS (including numbers HPS1 to HPS10). What is albinism? Albinism is an inherited condition in which CLIP AND COPY AND CLIP reduced pigmentation (coloring) is present in the body. As a result, people with albinism are often fair-skinned with light hair. However, skin, hair, and eye color may vary, as some people with albinism may have dark brown hair and green or hazel/brown eyes. Journal of Hematology People with albinism all have low vision and Figure 2. Patient’s platelet with virtually absent dense bodies visualized by electron microscopy. varying degrees of nystagmus. All people who have HPS have albinism, but not all circulate in the blood stream and help the people with albinism have HPS. blood to clot. HPS patients have normal Skin problems—The reduction of numbers of platelets, but they are not pigmentation in the skin from albinism made correctly and do not function well, so results in an increased chance of developing the blood does not clot properly. -
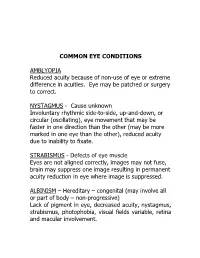
Common Eye Conditions
COMMON EYE CONDITIONS AMBLYOPIA Reduced acuity because of non-use of eye or extreme difference in acuities. Eye may be patched or surgery to correct. NYSTAGMUS - Cause unknown Involuntary rhythmic side-to-side, up-and-down, or circular (oscillating), eye movement that may be faster in one direction than the other (may be more marked in one eye than the other), reduced acuity due to inability to fixate. STRABISMUS - Defects of eye muscle Eyes are not aligned correctly, images may not fuse, brain may suppress one image resulting in permanent acuity reduction in eye where image is suppressed. ALBINISM – Hereditary – congenital (may involve all or part of body – non-progressive) Lack of pigment in eye, decreased acuity, nystagmus, strabismus, photophobia, visual fields variable, retina and macular involvement. ANIRIDIA – Hereditary Underdeveloped or absent iris. Decreased acuity, photophobia, nystagmus, cataracts, under developed retina. Visual fields normal unless glaucoma develops. CATARACTS – Congenital, hereditary, traumatic, disease, or age related (normal part of aging process) Lens opacity (chemical change in lens protein), decreased visual acuity, nystagmus, photophobia (light sensitivity). DIABETIC RETINOPATHY – Pathologic Retinal changes, proliferative – growth of abnormal new blood vessels, hemorrhage, fluctuating visual acuity, loss of color vision, field loss, retinal detachment, total blindness. GLAUCOMA (Congenital or adult) – “SNEAK THIEF OF SIGHT” hereditary, traumatic, surgery High intraocular pressure (above 20-21 mm of mercury) – (in children often accompanied by hazy corneas and large eyes), often due to obstructions that prevent fluid drainage, resulting in damage to optic nerve. Excessive tearing, photophobia, uncontrolled blinking, decreased acuity, constricted fields. HEMIANOPSIA – (Half-vision) optic pathway malfunction pathologic or trauma (brain injury, stroke or tumor) Macular vision may or may not be affected. -

Guidelines for Universal Eye Screening in Newborns Including RETINOPATHY of Prematurity
GUIDELINES FOR UNIVERSAL EYE SCREENING IN NEWBORNS INCLUDING RETINOPATHY OF PREMATURITY RASHTRIYA BAL SWASthYA KARYAKRAM Ministry of Health & Family Welfare Government of India June 2017 MESSAGE The Ministry of Health & Family Welfare, Government of India, under the National Health Mission launched the Rashtriya Bal Swasthya Karyakram (RBSK), an innovative and ambitious initiative, which envisages Child Health Screening and Early Intervention Services. The main focus of the RBSK program is to improve the quality of life of our children from the time of birth till 18 years through timely screening and early management of 4 ‘D’s namely Defects at birth, Development delays including disability, childhood Deficiencies and Diseases. To provide a healthy start to our newborns, RBSK screening begins at birth at delivery points through comprehensive screening of all newborns for various defects including eye and vision related problems. Some of these problems are present at birth like congenital cataract and some may present later like Retinopathy of prematurity which is found especially in preterm children and if missed, can lead to complete blindness. Early Newborn Eye examination is an integral part of RBSK comprehensive screening which would prevent childhood blindness and reduce visual and scholastic disabilities among children. Universal newborn eye screening at delivery points and at SNCUs provides a unique opportunity to identify and manage significant eye diseases in babies who would otherwise appear healthy to their parents. I wish that State and UTs would benefit from the ‘Guidelines for Universal Eye Screening in Newborns including Retinopathy of Prematurity’ and in supporting our future generation by providing them with disease free eyes and good quality vision to help them in their overall growth including scholastic achievement. -

Upper Eyelid Ptosis Revisited Padmaja Sudhakar, MBBS, DNB (Ophthalmology) Qui Vu, BS, M3 Omofolasade Kosoko-Lasaki, MD, MSPH, MBA Millicent Palmer, MD
® AmericAn JournAl of clinicAl medicine • Summer 2009 • Volume Six, number Three 5 Upper Eyelid Ptosis Revisited Padmaja Sudhakar, MBBS, DNB (Ophthalmology) Qui Vu, BS, M3 Omofolasade Kosoko-Lasaki, MD, MSPH, MBA Millicent Palmer, MD Abstract Epidemiology of Ptosis Blepharoptosis, commonly referred to as ptosis is an abnormal Although ptosis is commonly encountered in patients of all drooping of the upper eyelid. This condition has multiple eti- ages, there are insufficient statistics regarding the prevalence ologies and is seen in all age groups. Ptosis results from a con- and incidence of ptosis in the United States and globally.2 genital or acquired weakness of the levator palpebrae superioris There is no known ethnic or sexual predilection.2 However, and the Muller’s muscle responsible for raising the eyelid, dam- there have been few isolated studies on the epidemiology of age to the nerves which control those muscles, or laxity of the ptosis. A study conducted by Baiyeroju et al, in a school and a skin of the upper eyelids. Ptosis may be found isolated, or may private clinic in Nigeria, examined 25 cases of blepharoptosis signal the presence of a more serious underlying neurological and found during a five-year period that 52% of patients were disorder. Treatment depends on the underlying etiology. This less than 16 years of age, while only 8% were over 50 years review attempts to give an overview of ptosis for the primary of age. There was a 1:1 male to female ratio in the study with healthcare provider with particular emphasis on the classifica- the majority (68%) having only one eye affected. -

Clinical Manifestations of Congenital Aniridia
Clinical Manifestations of Congenital Aniridia Bhupesh Singh, MD; Ashik Mohamed, MBBS, M Tech; Sunita Chaurasia, MD; Muralidhar Ramappa, MD; Anil Kumar Mandal, MD; Subhadra Jalali, MD; Virender S. Sangwan, MD ABSTRACT Purpose: To study the various clinical manifestations as- were subluxation, coloboma, posterior lenticonus, and sociated with congenital aniridia in an Indian population. microspherophakia. Corneal involvement of varying degrees was seen in 157 of 262 (59.9%) eyes, glaucoma Methods: In this retrospective, consecutive, observa- was identified in 95 of 262 (36.3%) eyes, and foveal hy- tional case series, all patients with the diagnosis of con- poplasia could be assessed in 230 of 262 (87.7%) eyes. genital aniridia seen at the institute from January 2005 Median age when glaucoma and cataract were noted to December 2010 were reviewed. In all patients, the was 7 and 14 years, respectively. None of the patients demographic profile, visual acuity, and associated sys- had Wilm’s tumor. temic and ocular manifestations were studied. Conclusions: Congenital aniridia was commonly as- Results: The study included 262 eyes of 131 patients sociated with classically described ocular features. with congenital aniridia. Median patient age at the time However, systemic associations were characteristically of initial visit was 8 years (range: 1 day to 73 years). Most absent in this population. Notably, cataract and glau- cases were sporadic and none of the patients had par- coma were seen at an early age. This warrants a careful ents afflicted with aniridia. The most common anterior evaluation and periodic follow-up in these patients for segment abnormality identified was lenticular changes.