View Our IPC Annual Report 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Beer Shop Beer Shop
1 3 10 11 13 14 West Norfolk C5 E3 C4 C3 Sandringham House C2 C3 VISIT BRITAIN’S BIGGEST BEER SHOP & What To Do 2016 Plus WINE AND SPIRIT WWAREHOUSEAREHOUSE Sandringham House, the Royal Family’s country retreat, ATTRACTIONS is perhaps the most famous stately home in Norfolk - and certainly one of the most beautiful. The Coffee Shop at Thaxters Garden Centre is PLACES TO VISIT Opens Easter 2016 Set in 60 acres of stunning gardens, with a fascinating renowned locally for its own home-made cakes museum of Royal vehicles and mementos, the principal and scones baked daily. Its menu ranges from the EVENTS ground floor apartments with their charming collections popular cooked breakfast to sandwiches, baguettes YOUYOU DON’TDON’T HAVEHAVE Visit King’s Lynn’s of porcelain, jade, furniture and family portraits are open throughout West Norfolk and our homemade specials of the day. During the stunning new to the public. Visitor Centre open every day all year. warmer months there is an attractive garden when TOTO TRAVELTRAVEL THETHE attraction, which Open daily 26 March- 30 October you can sit and enjoy lunch and coffee. EXCEPT Wednesday 27 July. tells the stories of the Take a stroll around the attractive Garden Centre. Adults £14.00, Seniors £12.50, Children £7.00 GLOBEGLOBE TOTO ENJOYENJOY seafarers, explorers, Family (2 adults + 3 children) £35.00 It sells everything the garden could need as well as merchants, mayors, www.sandringhamestate.co.uk a large range of giftware. WORLDWORLD BEERS.BEERS.BEERS. magistrates and If you are staying in self-catering accommodation 4 North Brink, Wisbech, PE13 1LW 12 or a caravan there is a well stocked grocery store Tel: 01945 583160 miscreants who have A5 www.elgoods-brewery.co.uk C4 on site that sells hot chickens from its rotisserie, It is just a short haul to shaped King’s Lynn, one of freshly baked bread, newspapers, lottery and England’s most important everything you could possibly need. -

Regional Drive – Norfolk & Suffolk Friday 5
REGIONAL DRIVE – NORFOLK & SUFFOLK FRIDAY 5 – SATURDAY 6 MAY 2017 NORFOLK & SUFFOLK REGIONAL EVENT FRIDAY 5 – SATURDAY 6 MAY 2017 • SUDBURY REGIONAL SOCIAL FRIDAY 5 MAY • NORFOLK & SUFFOLK REGIONAL DRIVE SATURDAY 6 MAY • HUNTINGDON REGIONAL SOCIAL SATURDAY 6 MAY Join the GRRC as we set off on our first Regional Drive of 2017 to explore Suffolk and Norfolk across 5-6 May. Following the same format as our drives of 2016, the drive will begin with a social evening at Sudbury on Friday and end with a social at Huntingdon on Saturday, allowing Members from across East Anglia to pop by and say hello to the Club and other regional GRRC Members. Our aim from these events is to get like-minded Members together to enjoy their cars on some of the best roads and most beautiful areas of the UK. With this in mind, we have suggested a route which we believe explores some of the finest roads through Suffolk and Norfolk, but it is very much up to you how to make the most of the day. There are far too many quaint towns and wonderful routes to explore throughout East Anglia, but by using the guide below, we hope you will be able to tailor the day, in the knowledge that there is a group of like-minded GRRC members on the adventure with you. We have also built in plenty of extra time to allow Members to take photos and have rest stops along the way. We will start the weekend with a Friday night social at the Mill Hotel, Sudbury. -
Contents of Volume 14 Norwich Marriages 1813-37 (Are Distinguished by Letter Code, Given Below) Those from 1801-13 Have Also Been Transcribed and Have No Code
Norfolk Family History Society Norfolk Marriages 1801-1837 The contents of Volume 14 Norwich Marriages 1813-37 (are distinguished by letter code, given below) those from 1801-13 have also been transcribed and have no code. ASt All Saints Hel St. Helen’s MyM St. Mary in the S&J St. Simon & St. And St. Andrew’s Jam St. James’ Marsh Jude Aug St. Augustine’s Jma St. John McC St. Michael Coslany Ste St. Stephen’s Ben St. Benedict’s Maddermarket McP St. Michael at Plea Swi St. Swithen’s JSe St. John Sepulchre McT St. Michael at Thorn Cle St. Clement’s Erh Earlham St. Mary’s Edm St. Edmund’s JTi St. John Timberhill Pau St. Paul’s Etn Eaton St. Andrew’s Eth St. Etheldreda’s Jul St. Julian’s PHu St. Peter Hungate GCo St. George Colegate Law St. Lawrence’s PMa St. Peter Mancroft Hei Heigham St. GTo St. George Mgt St. Margaret’s PpM St. Peter per Bartholomew Tombland MtO St. Martin at Oak Mountergate Lak Lakenham St. John Gil St. Giles’ MtP St. Martin at Palace PSo St. Peter Southgate the Baptist and All Grg St. Gregory’s MyC St. Mary Coslany Sav St. Saviour’s Saints The 25 Suffolk parishes Ashby Burgh Castle (Nfk 1974) Gisleham Kessingland Mutford Barnby Carlton Colville Gorleston (Nfk 1889) Kirkley Oulton Belton (Nfk 1974) Corton Gunton Knettishall Pakefield Blundeston Cove, North Herringfleet Lound Rushmere Bradwell (Nfk 1974) Fritton (Nfk 1974) Hopton (Nfk 1974) Lowestoft Somerleyton The Norfolk parishes 1 Acle 36 Barton Bendish St Andrew 71 Bodham 106 Burlingham St Edmond 141 Colney 2 Alburgh 37 Barton Bendish St Mary 72 Bodney 107 Burlingham -

WESTGATE FARM, Burnham Market, Norfolk WESTGATE FARM Ringstead Road, Burnham Market, Norfolk PE31 8JR
WESTGATE FARM, Burnham Market, Norfolk WESTGATE FARM Ringstead Road, Burnham Market, Norfolk PE31 8JR Brancaster 5 miles. Holkham Beach 6 miles. Wells-next-the-Sea 7.5 miles. King’s Lynn 23 miles. Norwich 37 miles. London King’s Cross 1hr 40 minutes by rail from King’s Lynn Introduction: Tenure and Possession: The sale of Westgate Farm provides interested parties with an exceptionally rare All the property included herein is to be offered freehold with the benefit of vacant opportunity to purchase a coastal smallholding with planning potential on the outskirts of possession subject to those rights of Holdover detailed herein. the much sought-after North Norfolk Village of Burnham Market. Viewing: Set in a ring-fence with spectacular views to all sides, the sale comprises Westgate Viewing is accompanied and strictly by prior appointment only with the Vendors’ Farm House, Greenfields Bungalow, a range of modern farm buildings and arable land Agents, Cruso & Wilkin. Tel. 01553 691691. amounting to 11.07 hectares. Health and Safety: PARTICULARS: Given the potential hazards of a working farm and for your own personal safety we Location and Situation: would ask you to be as vigilant as possible when making an inspection, particularly Burnham Market is a stunning Georgian village complete with Village Green, around farm machinery. We regret to advise that children and/or pets are not permitted surrounded by 18th Century houses together with shops, boutiques and on the farm when viewing. Public Houses including The Hoste Arms. The village has a range of essential amenities including a doctors and a dental surgery, pharmacy, primary school and post office together with a bakery, butcher, fresh fish shop, beauty salon and a range of clothing outfitters. -

Parish Registers and Transcripts in the Norfolk Record Office
Parish Registers and Transcripts in the Norfolk Record Office This list summarises the Norfolk Record Office’s (NRO’s) holdings of parish (Church of England) registers and of transcripts and other copies of them. Parish Registers The NRO holds registers of baptisms, marriages, burials and banns of marriage for most parishes in the Diocese of Norwich (including Suffolk parishes in and near Lowestoft in the deanery of Lothingland) and part of the Diocese of Ely in south-west Norfolk (parishes in the deanery of Fincham and Feltwell). Some Norfolk parish records remain in the churches, especially more recent registers, which may be still in use. In the extreme west of the county, records for parishes in the deanery of Wisbech Lynn Marshland are deposited in the Wisbech and Fenland Museum, whilst Welney parish records are at the Cambridgeshire Record Office. The covering dates of registers in the following list do not conceal any gaps of more than ten years; for the populous urban parishes (such as Great Yarmouth) smaller gaps are indicated. Whenever microfiche or microfilm copies are available they must be used in place of the original registers, some of which are unfit for production. A few parish registers have been digitally photographed and the images are available on computers in the NRO's searchroom. The digital images were produced as a result of partnership projects with other groups and organizations, so we are not able to supply copies of whole registers (either as hard copies or on CD or in any other digital format), although in most cases we have permission to provide printout copies of individual entries. -

21 Bus Time Schedule & Line Route
21 bus time schedule & line map 21 Docking View In Website Mode The 21 bus line (Docking) has 4 routes. For regular weekdays, their operation hours are: (1) Docking: 2:30 PM (2) Hunstanton: 8:45 AM - 3:25 PM (3) King's Lynn: 7:30 AM - 4:50 PM (4) Sedgeford: 4:35 PM - 5:45 PM Use the Moovit App to ƒnd the closest 21 bus station near you and ƒnd out when is the next 21 bus arriving. Direction: Docking 21 bus Time Schedule 22 stops Docking Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 2:30 PM Transport Interchange, King's Lynn Tuesday 2:30 PM Kettlewell Lane, King's Lynn Littleport Street, King's Lynn Wednesday 2:30 PM Highgate School, King's Lynn Thursday 2:30 PM Friday 2:30 PM King Edward VII School, King's Lynn Saturday Not Operational Tesco, Gaywood Health Centre, King's Lynn Gayton Road, King's Lynn 21 bus Info Kent Road, King's Lynn Direction: Docking Stops: 22 Queensway, King's Lynn Trip Duration: 45 min Line Summary: Transport Interchange, King's Lynn, Elvington Road, King's Lynn Kettlewell Lane, King's Lynn, Highgate School, King's Lynn, King Edward VII School, King's Lynn, Tesco, Bus Shelter, Queen Elizabeth Hospital Gaywood, Health Centre, King's Lynn, Kent Road, King's Lynn, Queensway, King's Lynn, Elvington Road, King's Lynn, Bus Shelter, Queen Elizabeth Hospital, Ffolkes Arms, Hillington Ffolkes Arms, Hillington, Tapping House Norfolk Hospice, Hillington, Amner Road, Flitcham, Country Tapping House Norfolk Hospice, Hillington Stores, Bircham, Stocks Close, Bircham Tofts, Church Wheatƒelds, Hillington Civil -

RV Ratepayer Address 3,900 £ RK&J Jones Ltd 15 Bennett Street, Downham Market, Norfolk, PE38 9EE 2,100 £ 54 Bridge
RV Ratepayer Address £ 3,900 RK&J Jones ltd 15 Bennett Street, Downham Market, Norfolk, PE38 9EE £ 2,100 54 Bridge Street, Downham Market, Norfolk, PE38 9DJ £ 2,350 3 Fairfield Road, Downham Market, Norfolk, PE38 9ET £ 19,250 HSBC Bank Plc 24 High Street, Downham Market, Norfolk, PE38 9DB £ 950 The Chalet, Priory Road, Downham Market, Norfolk, PE38 9JS £ 220 213 Old Hunstanton Beach, Hunstanton, Norfolk, PE36 6JN £ 19,750 Borough Council of King's Lynn & West Norfolk Council Offices, Valentine Road, Hunstanton, Norfolk, PE36 5HG £ 25,750 North Lynn Discovery Ltd North Lynn Discovery Centre, Columbia Way, Kings Lynn, Norfolk, PE30 2LA £ 15,250 Hugh Smith (Estuary Road Ltd) In AdministrationEstuary Road, Kings Lynn, Norfolk, PE30 2HH £ 13,000 Mars Food UK Ltd 61 Oldmedow Road, Hardwick Industrial Estate, Kings Lynn, Norfolk, PE30 4JJ £ 1,375 Basement, 9 Portland Street, Kings Lynn, Norfolk, PE30 1PB £ 2,550 237 Saddlebow Road, Kings Lynn, Norfolk, PE30 5BW £ 3,250 Lynn Road, Gayton, Kings Lynn, Norfolk, PE32 1QJ £ 1,875 2 Fen Lane, Pott Row, Kings Lynn, Norfolk, PE32 1DA £ 4,350 Kings Lynn Sand & Gravel Co Ltd Big Pit, Wormegay Road, Blackborough End, Kings Lynn, Norfolk, PE32 1SG £ 1,825 Workshop R/O, 111 School Road, Upwell, Wisbech, Cambridgeshire, PE14 9ES £ 1,850 Workshop, Desford Lodge, Church Road, Walpole St Peter, Wisbech Cambridgeshire, PE14 7NS £ 320 Victory Farm, Eastmoor, Kings Lynn, Norfolk, PE33 9PY £ - Bexwell Tractors Ltd Alexander Works, High Street, Fincham, Kings Lynn, Norfolk, PE33 9EL £ 550 Caravan Site At Warren House, -

NORFOLK. SMI 793 Dyball Alfred, West Raynham, Faken- Hales William Geo
TRADES DIRECTORY. J NORFOLK. SMI 793 Dyball Alfred, West Raynham, Faken- Hales William Geo. Ingham, Norwich Kitteringham John, Tilney St. Law- ham Hall P. Itteringham, Aylsham R.S.O rence, Lynn Dyball E. T. 24 Fuller's hill, Yarmouth Hammond F. Barroway Drove, Downhm Knights Edwd. H. London rd. Harleston Dye Henry Samuel, 39 Audley street & Hammond Richard, West Bilney, Lynn Knott Charles, Ten Mile Bank, Downhm North Market road, Yarmouth & at Pentney, Swaffham Kybird J ames, Croxton, Thetford Earl Uriah, Coltishall, Norwich Hammond Robert Edward Hazel, Lade Frederick Wacton, Long Stratton Easter Frederick, Mileham, Swaffham Gayton, Lynn Lake Thomas, Binham, Wighton R.S.O Easter George, Blofield, Norwich Hammond William, Stow Bridge, Stow Lambert William Claydon, Wiggenhall Ebbs William, Alburgh, Harleston Bardolph, Downham St. Mary Magdalen, Lynn Edward Alfred, Griston, Thetford Hanton J ames, W estEnd street, Norwich Langham Alfred, Martham, Yarmouth Edwards Edward, Wretham, Great Harbord P. Burgh St. Margaret, Yarmth Lansdell Brothers, Hempnall, Norwich Hockham, Thetford Hardy Harry, Lake's end, Wisbech Lansdell Albert, Stratton St. Mary, Eggleton W. Great Ryburgh, Fakenham Harper Robt. Alfd. Halvergate, Nrwch Long Stratton R.S.O Eglington & Gooch, Hackford, Norwich Harrold Samuel, Church end, West Larner Henry, Stoke Ferry ~.0 Eke Everett, Mulbarton, Norwich Walton, Wisbech Last F. B. 93 Sth. Market rd. Yarmouth Eke Everet, Bracon Ash, Norwich Harrowven Henry, Catton, Norwich Lawes Harry Wm. Cawshm, Norwich Eke James, Saham Ton.ey, Thetford Hawes A. Terrington St. John, Wisbech Laws .Jo~eph, Spixworth, Norwich Eke R. Drayton, Norwich Hawes Robert Hilton, Terrington St. Leader James, Po!'ltwick, Norwich Ellis Charles, Palling, Norwich Clement, Lynn Leak T. -
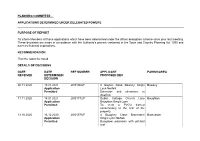
Delegated List 08.02.21 , Item PC197: PDF 348 KB
PLANNING COMMITTEE - APPLICATIONS DETERMINED UNDER DELEGATED POWERS PURPOSE OF REPORT To inform Members of those applications which have been determined under the officer delegation scheme since your last meeting. These decisions are made in accordance with the Authority’s powers contained in the Town and Country Planning Act 1990 and have no financial implications. RECOMMENDATION That the report be noted. DETAILS OF DECISIONS DATE DATE REF NUMBER APPLICANT PARISH/AREA RECEIVED DETERMINED/ PROPOSED DEV DECISION 20.11.2020 13.01.2021 20/01963/F 8 Gayton Road Bawsey King's Bawsey Application Lynn Norfolk Permitted Extension and alterations to dwelling 11.11.2020 18.01.2021 20/01772/F Dublin Cottage Church Lane Boughton Application Boughton King's Lynn Permitted To erect a PVCU framed conservatory to the rear of the property 13.10.2020 16.12.2020 20/01575/F 4 Boughey Close Brancaster Brancaster Application King's Lynn Norfolk Permitted Bungalow extension with pitched roof 05.11.2020 08.01.2021 20/01726/F The Smithy Main Road Brancaster Brancaster Application Staithe King's Lynn Permitted Installation of boat store 27.11.2020 20.01.2021 20/01890/F North House The Drove Brancaster Application Brancaster Staithe KINGS LYNN Permitted Variation of Condition 2 attached to planning permission 19/01480/F for minor changes to the design 22.09.2020 13.01.2021 20/01430/F The Old Crabbe Hall 22 Front Burnham Market Application Street Burnham Market Norfolk Permitted Single storey linked extension, alteration and conversion of stables, proposed door -

NORFOLK. Bould : the Lectern
128 DOCKING. NORFOLK. bould : the lectern,. of carved oak, was presented m Strachan Charles Edward E*lq. Heacham hall, Lynn n'l82 by the Misse:i! Chadwick, of Tunbridge Wells, in The chairmen of the New Hunstanton Urban District. memory of Mrs. H. E. Ha.re: the ancient font 'i.IJ adorned Council & Docking ,Rural District Council, for the with many carved figures, but much mutilated: the time being, are ex-oili.cio justices of the peace ohurch was new roofed in r875, and additions made, Clerk to the Justic~ G. Whitby, Hunstanton at a. cost of over £4,ooo, and now affords 65o sit tings. The register dates from tihe year 155 8. The Petty Se8sions are helq at the Sessions house, Docking, living is a. discharged vicarage, gross yearly . value the last monday in every month at r r a. m. & at the Council hall, New Hnnstanton, on t·he second monday £419, with 45 acres of glebe and residence, in the gift in each month at 10.30 a.m. The following places are of the Provost and Fellows of Eton College, on the included in the petty sessional division :-Barwick, nomination of the Bishop of Norwich, and held since Bircham Great, Birobam Newton, Biraham Tofts, Bran 1909 by the Rev. James Amiraux Fletcher B.A. of caster, Bul"'ltbam Deepdale, Burnb!lm Norton, Burnbam Corpus Christi College, Cambridge, surrogate· and Sutton & Uiph, Burnham Overy, Burnham Westgate; chaplain of. Docking union. The great tithes are .Buruham• Thorpe, North & South Creake, Ohoseley, commuted at [1,II4. The Wesleyan chapel is of red Docking, Fring, Heaoh:1m, Holme-next-the-Sea., Hun brick, and was erected in 1821 ; the Primitive Methodist stanton, New Hunsta'lton, Ingoldisthorpe, Ringstead, chapel, also of brick faced with cement, was erected in Sedgeford, .Shernbonrne, Snettisham, Stanhoe, Thorn 1836, and has 350 sittings. -

Areas Designated As 'Rural' for Right to Buy Purposes
Areas designated as 'Rural' for right to buy purposes Region District Designated areas Date designated East Rutland the parishes of Ashwell, Ayston, Barleythorpe, Barrow, 17 March Midlands Barrowden, Beaumont Chase, Belton, Bisbrooke, Braunston, 2004 Brooke, Burley, Caldecott, Clipsham, Cottesmore, Edith SI 2004/418 Weston, Egleton, Empingham, Essendine, Exton, Glaston, Great Casterton, Greetham, Gunthorpe, Hambelton, Horn, Ketton, Langham, Leighfield, Little Casterton, Lyddington, Lyndon, Manton, Market Overton, Martinsthorpe, Morcott, Normanton, North Luffenham, Pickworth, Pilton, Preston, Ridlington, Ryhall, Seaton, South Luffenham, Stoke Dry, Stretton, Teigh, Thistleton, Thorpe by Water, Tickencote, Tinwell, Tixover, Wardley, Whissendine, Whitwell, Wing. East of North Norfolk the whole district, with the exception of the parishes of 15 February England Cromer, Fakenham, Holt, North Walsham and Sheringham 1982 SI 1982/21 East of Kings Lynn and the parishes of Anmer, Bagthorpe with Barmer, Barton 17 March England West Norfolk Bendish, Barwick, Bawsey, Bircham, Boughton, Brancaster, 2004 Burnham Market, Burnham Norton, Burnham Overy, SI 2004/418 Burnham Thorpe, Castle Acre, Castle Rising, Choseley, Clenchwarton, Congham, Crimplesham, Denver, Docking, Downham West, East Rudham, East Walton, East Winch, Emneth, Feltwell, Fincham, Flitcham cum Appleton, Fordham, Fring, Gayton, Great Massingham, Grimston, Harpley, Hilgay, Hillington, Hockwold-Cum-Wilton, Holme- Next-The-Sea, Houghton, Ingoldisthorpe, Leziate, Little Massingham, Marham, Marshland -

The PARISH CHURCH of ALL SAINTS, STANHOE, Norfolk
The M PARISH y .7 > ./- CHURCH }/ „Ji "ft of ALL SAINTS, P STANHOE, Norfolk r As is the case of so many of our ancient parish churches, this one is in great need of money for restoration work particularly to the roof which is in a bad state. The compilers of this booklet hope that the restoration fund will benefit from its sale. THE PARISH CHURCH OF ALL SAINTS STANHOE - NORFOLK XHE beauty of the church is in its proportions which can best be seen from the chancel and looking back to the transitional west window which gives light to the whole building. The octagonal piers of the arcades, the lovely shafted arches of the chancel windows with a string-course connecting the whole are most satisfying, and best of all is the piscina-sedilia with its ogee arches and head-stops which seem to represent from E to W, a woman, a crowned king and a bishop. It is always unwise to give an exact date, but the time of building can be fixed with fair certainty from c 1290-1340 and most of the work mentioned, and the slim unbuttressed tower which iorms the south porch, belongs to this period. The doorways and most of the windows are also of this date, and the inner south doorwav appears to be earlier than the outer. The windows in the south aisle are a decade or two later and two in the north aisle were replaced by three-light windows in the 15th century and contain good clear glaze. In one heraldic glass with the Seymour crest of two eagles wings has been inserted in memory of Colonel Charles Seymour of Barwick House.