Understanding Glaucomatous Optic Neuropathy: the Synergy Between Clinical Observation and Investigation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Optic Disc Edema, Globe Flattening, Choroidal Folds, and Hyperopic Shifts Observed in Astronauts After Long-Duration Space Flight
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln NASA Publications National Aeronautics and Space Administration 10-2011 Optic Disc Edema, Globe Flattening, Choroidal Folds, and Hyperopic Shifts Observed in Astronauts after Long-duration Space Flight Thomas H. Mader Alaska Native Medical Center, [email protected] C. Robert Gibson Coastal Eye Associates Anastas F. Pass University of Houston Larry A. Kramer University of Texas Health Science Center Andrew G. Lee The Methodist Hospital See next page for additional authors Follow this and additional works at: https://digitalcommons.unl.edu/nasapub Part of the Physical Sciences and Mathematics Commons Mader, Thomas H.; Gibson, C. Robert; Pass, Anastas F.; Kramer, Larry A.; Lee, Andrew G.; Fogarty, Jennifer; Tarver, William J.; Dervay, Joseph P.; Hamilton, Douglas R.; Sargsyan, Ashot; Phillips, John L.; Tran, Duc; Lipsky, William; Choi, Jung; Stern, Claudia; Kuyumjian, Raffi; andolk, P James D., "Optic Disc Edema, Globe Flattening, Choroidal Folds, and Hyperopic Shifts Observed in Astronauts after Long-duration Space Flight" (2011). NASA Publications. 69. https://digitalcommons.unl.edu/nasapub/69 This Article is brought to you for free and open access by the National Aeronautics and Space Administration at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in NASA Publications by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Authors Thomas H. Mader, C. Robert Gibson, Anastas F. Pass, Larry A. -

98796-Anatomy of the Orbit
Anatomy of the orbit Prof. Pia C Sundgren MD, PhD Department of Diagnostic Radiology, Clinical Sciences, Lund University, Sweden Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lay-out • brief overview of the basic anatomy of the orbit and its structures • the orbit is a complicated structure due to its embryological composition • high number of entities, and diseases due to its composition of ectoderm, surface ectoderm and mesoderm Recommend you to read for more details Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 3 x 3 Imaging technique 3 layers: - neuroectoderm (retina, iris, optic nerve) - surface ectoderm (lens) • CT and / or MR - mesoderm (vascular structures, sclera, choroid) •IOM plane 3 spaces: - pre-septal •thin slices extraconal - post-septal • axial and coronal projections intraconal • CT: soft tissue and bone windows 3 motor nerves: - occulomotor (III) • MR: T1 pre and post, T2, STIR, fat suppression, DWI (?) - trochlear (IV) - abducens (VI) Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Superior orbital fissure • cranial nerves (CN) III, IV, and VI • lacrimal nerve • frontal nerve • nasociliary nerve • orbital branch of middle meningeal artery • recurrent branch of lacrimal artery • superior orbital vein • superior ophthalmic vein Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. -
Eye60. Instrumental Eye Examination.Pdf
INSTRUMENTAL EYE EXAMINATION Eye60 (1) Instrumental Eye Examination Last updated: May 9, 2019 “BEDSIDE” EXAMINATIONS ..................................................................................................................... 1 OPHTHALMOSCOPY (FUNDUSCOPY) ........................................................................................................ 1 DIRECT OPHTHALMOSCOPY .................................................................................................................... 1 INDIRECT OPHTHALMOSCOPY ................................................................................................................. 2 OPHTHALMOSCOPIC FINDINGS ............................................................................................................... 2 Hypertensive retinopathy ................................................................................................................. 6 Diabetic retinopathy ......................................................................................................................... 7 PEDIATRIC ASPECTS ............................................................................................................................... 9 APPLANATION TONOMETRY .................................................................................................................... 9 SLIT LAMP EXAMINATION (BIOMICROSCOPY) ........................................................................................ 9 ULTRASONOGRAPHY .............................................................................................................................. -

Anatomy and Physiology of the Afferent Visual System
Handbook of Clinical Neurology, Vol. 102 (3rd series) Neuro-ophthalmology C. Kennard and R.J. Leigh, Editors # 2011 Elsevier B.V. All rights reserved Chapter 1 Anatomy and physiology of the afferent visual system SASHANK PRASAD 1* AND STEVEN L. GALETTA 2 1Division of Neuro-ophthalmology, Department of Neurology, Brigham and Womens Hospital, Harvard Medical School, Boston, MA, USA 2Neuro-ophthalmology Division, Department of Neurology, Hospital of the University of Pennsylvania, Philadelphia, PA, USA INTRODUCTION light without distortion (Maurice, 1970). The tear–air interface and cornea contribute more to the focusing Visual processing poses an enormous computational of light than the lens does; unlike the lens, however, the challenge for the brain, which has evolved highly focusing power of the cornea is fixed. The ciliary mus- organized and efficient neural systems to meet these cles dynamically adjust the shape of the lens in order demands. In primates, approximately 55% of the cortex to focus light optimally from varying distances upon is specialized for visual processing (compared to 3% for the retina (accommodation). The total amount of light auditory processing and 11% for somatosensory pro- reaching the retina is controlled by regulation of the cessing) (Felleman and Van Essen, 1991). Over the past pupil aperture. Ultimately, the visual image becomes several decades there has been an explosion in scientific projected upside-down and backwards on to the retina understanding of these complex pathways and net- (Fishman, 1973). works. Detailed knowledge of the anatomy of the visual The majority of the blood supply to structures of the system, in combination with skilled examination, allows eye arrives via the ophthalmic artery, which is the first precise localization of neuropathological processes. -
Using the Ophthalmoscope: Viewing the Optic Disc and Retina
Using the Ophthalmoscope: Viewing the Optic Disc and Retina Judith Warner, MD University of Utah THE OPHTHALMOSCOPE DIRECT OPHTHALMOSCOPY • Jan Purkinje 1823 • Hermann von Helmholtz 1851 • Hand held ophthalmoscope • Direct up-right image Dials of the Ophthalmoscope RED-FREE FILTER (GREEN LIGHT) 450 nm monochromatic light nerve fiber layer optic nerve drusen OTHER DIALS • Used for measuring lesion size • Looking for the center of fixation OTHER DIALS: SLIT BEAM The wheel has lenses of power Panoptic-ophthalmoscope Direct type Wider field of view Distance from pt greater Similar apertures Not as easy to carry Slightly dimmer light source Not as magnified view of Disc Clean the rubber cup between patients Photographs: http://panoptic.welchallyn.com/faq.html WHEN EVER POSSIBLE: DILATE THE PATIENT Steps to Direct Ophthalmoscopy • Dimly lit room • Dilating drops • Patient fixates distant target • Align yourself • Red reflex • Dial in HOW TO USE THE DIRECT Ophthalmoscope.avi ophthalmoscope.wmv THE RED REFLEX The layers you will go through to see the optic disc THE OPTIC NERVE WHAT YOU SHOULD OBSERVE IN EVERYONE RIGHT EYE AND LEFT EYE THE NORMAL DISC • The disc is 1.62 mm or 1 million fibers • Central retinal artery and vein • Lamina Cribrosa • The optic cup The Normal Disc Appearance The lamina cribrosa is an important disc structure --Means Sieve --Anatomically present in all discs --Visible in about 1/3 --Shallow in myopia Look at the Cup-to-disc ratio: WHAT IS THE CUP-TO-DISC RATIO? .7 NO CUP 0.1 CUP 0.3 CUP 0.7 CUP 0.9 CUP What is the cup -

The Horizontal Raphe of the Human Retina and Its Watershed Zones
vision Review The Horizontal Raphe of the Human Retina and its Watershed Zones Christian Albrecht May * and Paul Rutkowski Department of Anatomy, Medical Faculty Carl Gustav Carus, TU Dresden, 74, 01307 Dresden, Germany; [email protected] * Correspondence: [email protected] Received: 24 September 2019; Accepted: 6 November 2019; Published: 8 November 2019 Abstract: The horizontal raphe (HR) as a demarcation line dividing the retina and choroid into separate vascular hemispheres is well established, but its development has never been discussed in the context of new findings of the last decades. Although factors for axon guidance are established (e.g., slit-robo pathway, ephrin-protein-receptor pathway) they do not explain HR formation. Early morphological organization, too, fails to establish a HR. The development of the HR is most likely induced by the long posterior ciliary arteries which form a horizontal line prior to retinal organization. The maintenance might then be supported by several biochemical factors. The circulation separate superior and inferior vascular hemispheres communicates across the HR only through their anastomosing capillary beds resulting in watershed zones on either side of the HR. Visual field changes along the HR could clearly be demonstrated in vascular occlusive diseases affecting the optic nerve head, the retina or the choroid. The watershed zone of the HR is ideally protective for central visual acuity in vascular occlusive diseases but can lead to distinct pathological features. Keywords: anatomy; choroid; development; human; retina; vasculature 1. Introduction The horizontal raphe (HR) was first described in the early 1800s as a horizontal demarcation line that extends from the macula to the temporal Ora dividing the temporal retinal nerve fiber layer into a superior and inferior half [1]. -

Molecular Regulation of Visual System Development: More Than Meets the Eye
Downloaded from genesdev.cshlp.org on September 30, 2021 - Published by Cold Spring Harbor Laboratory Press REVIEW Molecular regulation of visual system development: more than meets the eye Takayuki Harada,1,2 Chikako Harada,1,2 and Luis F. Parada1,3 1Department of Developmental Biology and Kent Waldrep Foundation Center for Basic Neuroscience Research on Nerve Growth and Regeneration, University of Texas Southwestern Medical Center, Dallas, Texas 75235, USA; 2Department of Molecular Neurobiology, Tokyo Metropolitan Institute for Neuroscience, Fuchu, Tokyo 183-8526, Japan Vertebrate eye development has been an excellent model toderm, intercalating mesoderm, surface ectoderm, and system to investigate basic concepts of developmental neural crest (Fig. 1). The neuroectoderm differentiates biology ranging from mechanisms of tissue induction to into the retina, iris, and optic nerve; the surface ecto- the complex patterning and bidimensional orientation of derm gives rise to lens and corneal epithelium; the me- the highly specialized retina. Recent advances have shed soderm differentiates into the extraocular muscles and light on the interplay between numerous transcriptional the fibrous and vascular coats of the eye; and neural crest networks and growth factors that are involved in the cells become the corneal stroma sclera and corneal en- specific stages of retinogenesis, optic nerve formation, dothelium. The vertebrate eye originates from bilateral and topographic mapping. In this review, we summarize telencephalic optic grooves. In humans, optic vesicles this recent progress on the molecular mechanisms un- emerge at the end of the fourth week of development and derlying the development of the eye, visual system, and soon thereafter contact the surface ectoderm to induce embryonic tumors that arise in the optic system. -

The Optic Disc in Glaucoma I: Classification
Br J Ophthalmol: first published as 10.1136/bjo.60.11.778 on 1 November 1976. Downloaded from Brit. Y. Ophthal. (1976) 6o, 778 The optic disc in glaucoma i: Classification R. A. HITCHINGS Moorfields Eye Hospital, City Road, London AND G. L. SPAETH Wills Eye Hospital, Spring Garden Street, Philadelphia I9I30, USA The pale, cupped disc found in the final stages of deepening of the cup exposing the lamina cribrosa glaucomatous disease has been known from the (the 'laminar dots' sign (Reed and Spaeth, 1974)); time of Von Graefe (I854). Since then many and change in the course of the retinal vessel which observers have described changes that occur at the is seen as a sharp change in direction ('kinking' or optic disc in chronic, simple glaucoma. There has bayoneting (Reed and Spaeth, 1974)). In addition, been particular interest in changes which may the presence of localized regions of nerve fibre loss occur in the early stages of the disease. or 'gutters' has been demonstrated in some cases Studies of the normal population have shown of early glaucoma by Hoyt, Frisen, and Neuman that while there is a wide diversity in the appearance (1973). copyright. of the normal optic disc, in a single subject (Armaly, The aim of this paper was to assess systematically I969; Fishman, I970; Kolker and Hetherington, glaucomatous discs and look for those features that 1970; Portnoy, 1973) the two discs are remarkably are commonly associated. As a result, five different similar (Witsiuk, I966; Kronfeld, 1970; Woodruff, types of optic disc appearance are described. 1970; Portnoy, I973). -

Peri-Papillary Atrophy
Peri-Papillary Atrophy Maryke Neiberg, OD Author’s Bio Dr. Maryke Neiberg is an associate professor and full-time faculty at Western University College of Optometry in Pomona, California. Any opinions expressed in this article are her own and she has no financial interest to disclose. ________________________________________________________________________________________________ As optometrists, the optic nerve and rim tissue are of great interest to us. We look very carefully at the disc margins, color, and cup-to-disk ratio. We certainly look at the nerve fiber layer, and we may even pay special attention to the tissue directly surrounding the optic nerve. What can this area tell us? To answer this question, we would have to know a little about the unique anatomy of this area. This area is significant in terms of its vascular supply. It shares its vascular supply with that of the prelaminar, laminar and retrolaminar optic nerve. This section of the optic nerve and the peri-papillary area is supplied by the circle of Zinn-Haller, which represents anastomosis of the short posterior cilliary arteries.1 Usually, this area appears uniform in pigmentation with a clear demarcation between retina and optic nerve. In some cases, the optic nerve is surrounded by an area of hyper and hypopigmentation that may encircle the disc margin, commonly more visible in the temporal disc area.2 This pigment disturbance or mottling represents chorioretinal atrophy around the optic disc. This chorioretinal atrophy is known as peri-papillary or para-papillary atrophy (PPA), and is a relatively common finding. 3 Fluorescein or indocyanogreen angiopathy show characteristic filling patterns that can be used to further differentiate the peripapillary atrophy. -

Determining the Location of the Fovea Centralis Via En-Face SLO and Cross-Sectional OCT Imaging in Patients Without Retinal Pathology
Article Determining the Location of the Fovea Centralis Via En-Face SLO and Cross-Sectional OCT Imaging in Patients Without Retinal Pathology Archana A. Nair1, Rebecca Liebenthal1, Shefali Sood1, Grant L. Hom2, Marc E. Ohlhausen3,ThaisF.Conti2,CarolinaC.S.Valentim2, Hiroshi Ishikawa1, Gadi Wollstein1,JoelS.Schuman1, Rishi P. Singh2, and Yasha S. Modi1 1 Department of Ophthalmology, NYU Langone Health, New York University, New York, NY, USA 2 Center for Ophthalmic Bioinformatics, Cole Eye Institute, Cleveland Clinic, Cleveland, OH, USA 3 Case Western Reserve University, Cleveland OH, USA Correspondence: Yasha S. Modi, 222 Purpose: The purpose was to establish the position of the fovea centralis to the optic E. 41st Street, 3rd Floor,NewYork,NY nerve via en-face, near-infrared spectral domain optical coherence tomography (NIR- 10017, USA. e-mail: OCT) in healthy patients. This may shed light on physiological variability and be used [email protected] for studying subtle cases of foveal ectopia in macular pathology and after retinal detach- Received: July 15, 2020 ment. Accepted: January 3, 2021 Methods: SD-OCT data of 890 healthy eyes were retrospectively analyzed. Exclusion Published: February 17, 2021 criteria included axial myopia causing tilting of the optic disc, peripapillary atrophy >1/3 Keywords: fovea centralis; OCT; the width of the disc, macular images excluding greater than half of the optic disc, retina and patients unable to maintain vertical head positioning. Two independent reviewers measured the horizontal and vertical distance from the fovea to the optic disc center and Citation: Nair AA, Liebenthal R, Sood optic disc diameter via cross-sectional and en-face scanning laser ophthalmoloscopy S, Hom GL, Ohlhausen ME, Conti TF, OCT imaging. -
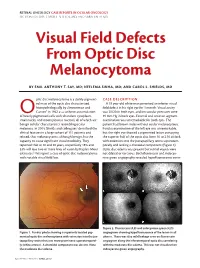
Visual Field Defects from Optic Disc Melanocytoma
RETINAL ONCOLOGY CASE REPORTS IN OCULAR ONCOLOGY SECTION EDITORS: CAROL L. SHIELDS, MD; AND SARA LALLY, MD Visual Field Defects From Optic Disc Melanocytoma BY EMIL ANTHONY T. SAY, MD; NEELEMA SINHA, MD; AND CAROL L. SHIELDS, MD ptic disc melanocytoma is a darkly pigment- CASE DESCRIPTION ed mass of the optic disc characterized A 33 year-old white man perceived an inferior visual histopathologically by Zimmerman and field defect in his right eye for 1 month. Visual acuity O Garron1 in 1962 as a uniform accumulation was 20/20 in both eyes, and intraocular pressures were of heavily pigmented cells with abundant cytoplasm, 19 mm Hg in both eyes. External and anterior segment small nuclei, and inconspicuous nucleoli, all of which are examination was unremarkable for both eyes. The benign cellular characteristics resembling ocular patient had brown irides without ocular melanocytosis. melanosis. In 2004, Shields and colleagues2 described the Fundus examination of the left eye was unremarkable, clinical features in a large cohort of 115 patients and but the right eye showed a pigmented lesion occupying related, that melanocytoma, although benign, has the the superior half of the optic disc from 10 to 2:30 o’clock, capacity to cause significant visual morbidity. They with extension into the juxtapapillary retina superotem- reported that at 10 and 20 years, respectively 18% and porally and lacking a choroidal component (Figure 1). 33% will lose two or more lines of vision by Kaplan-Meier Optic disc edema was present but retinal vessels were estimates.2 We report a case of optic disc melanocytoma not dilated or tortuous. -

Your Glaucoma Eye Examination: Part 2 Your Optic Disc
Your Glaucoma Eye Examination: Part 2 Your Optic Disc In the last issue of Eyelights we discussed What happens in glaucoma? the significance of eye pressure measurement Glaucoma causes damage to the nerve fibres in glaucoma care. This time we look at the and although the exact mechanism is still importance of examining the optic disc. unknown, there are two main theories that may explain glaucoma damage. What is the optic disc? The optic disc or optic nerve head is the The mechanical theory proposes it is the portion of the optic nerve which can be seen effect of eye pressure that damages the on examination of your eye. nerve fibres. It is thought that the nerve fibres are compressed at their exit point and The optic nerve begins in the eye and is continued, long-term damage causes the composed of 1,200,000 tiny nerve fibres that nerve fibres to atrophy or slowly die. send signals from the eye to the brain. It is these nerve fibres that can be seen, almost The vascular or “blood flow” theory proposes end-on, within the eye. that the pressure of the eye has an effect on blood flow to the optic nerve. If the nerve Each nerve fibre receives visual signals from fibres are starved of blood, nutrients and a certain area of retina and thus represents oxygen, then they undergo atrophy. an area of your field of vision. The loss of nerve fibres means that there will The typical optic disc is a circular structure be a corresponding loss or defect in the visual where the nerve fibres exit the eye.