Histological Evidence of Alternating Ovulation in Women A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter V FOLLICULAR DYNAMICS and REPRODUCTIVE
Chapter V FOLLICULAR DYNAMICS AND REPRODUCTIVE TECHNOLOGIES IN BUFFALO Giuseppina Maria Terzano Istituto Sperimentale per la Zootecnia (Animal Production Research Institute) Via Salaria 31, 00016 Monterotondo (Rome), Italy The general characteristics of reproduction like seasonality, cyclicity and ovulation differ widely in mammals for the following reasons: a) reproductive activity may take place during the whole year or at defined seasons, according to the species and their adaptation to environmental conditions; thus, photoperiod plays a determinant role in seasonal breeders such as rodents, carnivores and ruminants (sheep, goats, buffaloes, deer, etc.,). An extreme situation is observed in foxes with only one ovulation per year, occurring in January or February; b) mammals may be distinguished according to the absence or presence of spontaneous ovulations: in the first group of mammals ( rabbits, hares, cats, mink, camels, Llama), the ovulation is induced by mating and cyclicity is not obvious; in the second group, ovulation occurs spontaneously in each cycle, separating the follicular phase from the luteal phase; c) the length of cycles is quite different among species: small rodents have short cycles of four or five days, farm animals and primates have longer cycles (sheep: 17 days; cow, goat, buffalo, horse and pig: 21 days; primates: 28 days), and dogs are characterized by long cycles of six to seven months, including a two month luteal phase (Concannon, 1993); d) ovulation rates differ widely among species and breeds within a given species: in sheep for example, Merinos d'Arles or Ile-de-France breeds have only one ovulation per cycle, whereas average rates of two to four ovulations per cycle are observed in prolific breeds like Romanov or Finn (Land et al., 1973). -
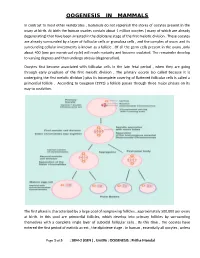
Oogenesis in Mammals
OOGENESIS IN MAMMALS In contrast to most other vertebrates , mammals do not replenish the stores of oocytes present in the ovary at birth. At birth the human ovaries contain about 1 million oocytes ( many of which are already degenerating) that have been arrested in the diplotene stage of the first meiotic division . These oocytes are already surrounded by a layer of follicular cells or granulosa cells , and the complex of ovum and its surrounding cellular investments is known as a follicle . Of all the germ cells present in the ovary ,only about 400 (one per menstrual cycle) will reach maturity and become ovulated. The remainder develop to varying degrees and then undergo atresia (degeneration). Oocytes first become associated with follicular cells in the late fetal period , when they are going through early prophase of the first meiotic division . The primary oocyte (so called because it is undergoing the first meiotic division ) plus its incomplete covering of flattened follicular cells is called a primordial follicle . According to Gougeon (1993) a follicle passes through three major phases on its way to ovulation. The first phase is characterized by a large pool of nongrowing follicles , approximately 500,000 per ovary at birth. In this pool are primordial follicles, which develop into primary follicles by surrounding themselves with a complete single layer of cuboidal follicular cells . By this time , the oocytes have entered the first period of meiotic arrest , the diplotene stage . In human , essentially all oocytes , unless Page 1 of 5 : SEM-2 (GEN ) , Unit#6 : OOGENESIS : Pritha Mondal they degenerate ,remain arrested in the diplotene stage until puberty ; some will not progress past the diplotene stage until the woman’s last reproductive cycle (age 45 to 55 years). -

Polycystic Ovary Syndrome.Pdf
Female reproductive system diseases Polycystic ovary syndrome Introduction: Polycystic ovary syndrome is one of the most common hormonal disorders among women. The name of this condition comes from the cysts that develop when ovulation vesicles get trapped under the surface of the ovaries preventing them from releasing the eggs. Cause: Normally, the pituitary gland in the brain secretes hormones (FSH) and (LH), that are responsible for controlling ovulation, while the ovary secretes estrogen and progesterone hormones, which prepare the uterus for the egg. The ovary also secretes the male hormone (androgen). However, in the case of polycystic ovary syndrome, the pituitary gland secretes excess amounts of (LH) and the ovary secretes excess amounts of the male hormone (androgen), resulting in irregular menstrual cycles and difficulties conceiving, as well as an increase facial hair and acne. There are many factors that may play a role in causing polycystic ovary syndrome: • Increased resistance to insulin (high blood glucose levels). • Heredity Symptoms: • Menstrual cycle abnormalities: The duration of the menstrual cycle may be prolonged to 35 days, or it could become less frequent occurring less than 8 times a year or it could be completely absent. • Increased body and facial hair • Acne • Obesity • Difficulty conceiving Diagnosis: • Medical history: Absence of the menstrual cycle - increased facial and body hair - acne - excess weight. • Ultrasound examination: of the uterus and ovaries • Blood test: To measure hormone levels, especially androgens and (LH). Treatment: Treatment depends on the symptoms regardless of whether the woman wants to conceive or not: • Lifestyle changes: This includes following a low-carb diet that is rich in grains, vegetables, fruits and small amounts of meat. -

Evolution of Oviductal Gestation in Amphibians MARVALEE H
THE JOURNAL OF EXPERIMENTAL ZOOLOGY 266394-413 (1993) Evolution of Oviductal Gestation in Amphibians MARVALEE H. WAKE Department of Integrative Biology and Museum of Vertebrate Zoology, University of California,Berkeley, California 94720 ABSTRACT Oviductal retention of developing embryos, with provision for maternal nutrition after yolk is exhausted (viviparity) and maintenance through metamorphosis, has evolved indepen- dently in each of the three living orders of amphibians, the Anura (frogs and toads), the Urodela (salamanders and newts), and the Gymnophiona (caecilians). In anurans and urodeles obligate vivi- parity is very rare (less than 1%of species); a few additional species retain the developing young, but nutrition is yolk-dependent (ovoviviparity) and, at least in salamanders, the young may be born be- fore metamorphosis is complete. However, in caecilians probably the majority of the approximately 170 species are viviparous, and none are ovoviviparous. All of the amphibians that retain their young oviductally practice internal fertilization; the mechanism is cloaca1 apposition in frogs, spermato- phore reception in salamanders, and intromission in caecilians. Internal fertilization is a necessary but not sufficient exaptation (sensu Gould and Vrba: Paleobiology 8:4-15, ’82) for viviparity. The sala- manders and all but one of the frogs that are oviductal developers live at high altitudes and are subject to rigorous climatic variables; hence, it has been suggested that cold might be a “selection pressure” for the evolution of egg retention. However, one frog and all the live-bearing caecilians are tropical low to middle elevation inhabitants, so factors other than cold are implicated in the evolu- tion of live-bearing. -

The Discovery of Different Types of Cervical Mucus and the Billings Ovulation Method
The Discovery of Different Types of Cervical Mucus and the Billings Ovulation Method Erik Odeblad Emeritus Professor, Dept. of Medical Biophysics, University of Umeå, Sweden Published with permission from the Bulletin of the Ovulation Method Research and Reference Centre of Australia, 27 Alexandra Parade, North Fitzroy, Victoria 3068, Australia, Volume 21, Number 3, pages 3-35, September 1994. Copyright © Ovulation Method Research and Reference Centre of Australia 1. Abstract 2. Introduction 3. Anatomy and Physiology 4. What is Mucus? 5. The Commencement of my Research 6. The Existence of Different Types of Crypts and of Mucus 7. Identification and Description of G, L, and S Mucus 8. G- and G+ Mucus 9. Age, Pregnancy, the Pill and Microsurgery 10. P Mucus 11. F Mucus 12. The Role of the Vagina 13. The Different Types of Secretions and the Billings Ovulation Method 14. Early Infertile Days 15. The Days of Possible Fertility 16. Late Infertile Days 17. Anovulatory Cycles 18. Lactation 19. Diseases and the Billings Ovulation Method 20. The Future 21. Acknowledgements 22. Author's Note 23. References 24. Appendix Abstract An introduction to and some new anatomical and physiological aspects of the cervix and vagina are presented and also an explanation of the biosynthesis and molecular structure of mucus. The history of my discoveries of the different types of cervical mucus is given. In considering my microbiological investigations I suspected the existence of different types of crypts and cervical mucus and in 1959 1 proved the existence of these different types. The method of examining viscosity by nuclear magnetic resonance was applied to microsamples of mucus extracted 1 outside of several crypts. -

The Effectiveness and Safety of the Early Follicular Phase Full-Dose Down
The effectiveness and safety of the early follicular phase full-dose down- regulation protocol for controlled ovarian hyperstimulation: a randomized, paralleled controlled, multicenter trial 2018-12-29 Background Since the first “tube baby”, Louise Brown, was born in the United Kingdom in 1978, many infertile couples have been benefitted from in vitro fertilization and embryo transfer (IVF-ET) and intracytoplasmic sperm injection (ICSI). It is reported that there are over 5 million babies born with the help of assisted reproductive technology (ART). According to the 2015 national data published by Human Fertility and Embryology Authority (HFEA, 48,147 women received 61,726 IVF/ICSI cycles and gave birth to 17,041 newborns [1]. In the United States, 169,602 IVF/ICSI cycles were performed in 2014 and 68,791 tubal babies were born [2]. China has a huge population base, and therefore has a substantial number of infertile couples. Although a late starter, China is developing rapidly in ART and playing a more and more important role in the area of reproductive medicine. In spite of the continuous development in ART, so far, the overall success rate of IVF/ICSI is still hovering around 25-40%. The live birth rate per stimulated cycle is 25.6% in the UK in 2015, fluctuating from 1.9% in women aged 45 and elder to 32.2% in women younger than 35 years old [1]. The IVF/ICSI success rate in 2014 in the US is similar [2]. In China, according to the data submitted by 115 reproductive medicine centers on the ART data reporting system developed by Chinese Society of Reproductive Medicine, the delivery rate is about 40% [3]. -

Women's Menstrual Cycles
1 Women’s Menstrual Cycles About once each month during her reproductive years, a woman has a few days when a bloody fluid leaves her womb and passes through her vagina and out of her body. This normal monthly bleeding is called menstruation, or a menstrual period. Because the same pattern happens each month, it is called the menstrual cycle. Most women bleed every 28 days. But some bleed as often as every 20 days or as seldom as every 45 days. Uterus (womb) A woman’s ovaries release an egg once a month. If it is Ovary fertilized she may become pregnant. If not, her monthly bleeding will happen. Vagina Menstruation is a normal part of women’s lives. Knowing how the menstrual cycle affects the body and the ways menstruation changes over a woman’s lifetime can let you know when you are pregnant, and help you detect and prevent health problems. Also, many family planning methods work best when women and men know more about the menstrual cycle (see Family Planning). 17 December 2015 NEW WHERE THERE IS NO DOCTOR: ADVANCE CHAPTERS 2 CHAPTER 24: WOMEN’S MENSTRUAL CYCLES Hormones and the menstrual cycle In women, the hormones estrogen and progesterone are produced mostly in the ovaries, and the amount of each one changes throughout the monthly cycle. During the first half of the cycle, the ovaries make mostly estrogen, which causes the lining of the womb to thicken with blood and tissue. The body makes the lining so a baby would have a soft nest to grow in if the woman became pregnant that month. -
Menstrual Health Glossary Key Words and Acronyms in the Field, from UNICEF + WHO
Menstrual Health Glossary Key words and acronyms in the field, from UNICEF + WHO Menstruation or menses is the natural bodily process of releasing blood and associated matter from the uterus through the vagina as part of the menstrual cycle.¹ A menstruator is a person who menstruates and therefore has menstrual health and hygiene needs – including girls, women, transgender and non-binary persons.¹ Menarche is the onset of menstruation, the time when a girl has her first menstrual period.¹ Menstrual hygiene materials are the products used to catch menstrual flow, such as pads, cloths, tampons or cups. These may also be referred to as menstrual materials or period products.¹ Menstrual Health Glossary Key words and acronyms in the field, from UNICEF + WHO Menstrual supplies are other supportive items needed for MHH, such as body and laundry soap, underwear and pain relief items.¹ Menstrual Hygiene Management (MHM) refers to management of hygiene associated with the menstrual process.¹ Adequate MHM involves: Knowledge and awareness about the menstrual process. Menstrual hygiene materials such as washable pads, disposable pads, tampons, and cups,WASH infrastructure such as Safe, clean, convenient, and private spaces for changing, washing, and/or disposing of menstrual hygiene materials. Adequate amounts of clean water and soap. Supportive social environments that enable menstruators to manage their periods with dignity and confidence. Policies and systems that create positive norms and dismantle limitations associated with menstruation.² Menstrual -
![Oogenesis [PDF]](https://docslib.b-cdn.net/cover/2902/oogenesis-pdf-452902.webp)
Oogenesis [PDF]
Oogenesis Dr Navneet Kumar Professor (Anatomy) K.G.M.U Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Development of ovum (oogenesis) • Maturation of follicle • Fate of ovum and follicle Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Site – ovary • Duration – 7th week of embryo –primordial germ cells • -3rd month of fetus –oogonium • - two million primary oocyte • -7th month of fetus primary oocyte +primary follicle • - at birth primary oocyte with prophase of • 1st meiotic division • - 40 thousand primary oocyte in adult ovary • - 500 primary oocyte attain maturity • - oogenesis completed after fertilization Dr Navneet Kumar Dr NavneetKumar Professor Professor (Anatomy) Anatomy KGMU Lko K.G.M.U Development of ovum Oogonium(44XX) -In fetal ovary Primary oocyte (44XX) arrest till puberty in prophase of 1st phase meiotic division Secondary oocyte(22X)+Polar body(22X) 1st phase meiotic division completed at ovulation &enter in 2nd phase Ovum(22X)+polarbody(22X) After fertilization Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Dr Navneet Kumar Dr ProfessorNavneetKumar (Anatomy) Professor K.G.M.UAnatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Primordial follicle -Follicular cells Primary follicle -Zona pallucida -Granulosa cells Secondary follicle Antrum developed Ovarian /Graafian follicle - Theca interna &externa -Membrana granulosa -Antrial -
Variability in the Length of Menstrual Cycles Within and Between Women - a Review of the Evidence Key Points
Variability in the Length of Menstrual Cycles Within and Between Women - A Review of the Evidence Key Points • Mean cycle length ranges from 27.3 to 30.1 days between ages 20 and 40 years, follicular phase length is 13-15 days, and luteal phase length is less variable and averages 13-14 days1-3 • Menstrual cycle lengths vary most widely just after menarche and just before menopause primarily as cycles are anovulatory 1 • Mean length of follicular phase declines with age3,11 while luteal phase remains constant to menopause8 • The variability in menstrual cycle length is attributable to follicular phase length1,11 Introduction Follicular and luteal phase lengths Menstrual cycles are the re-occurring physiological – variability of menstrual cycle changes that happen in women of reproductive age. Menstrual cycles are counted from the first day of attributable to follicular phase menstrual flow and last until the day before the next onset of menses. It is generally assumed that the menstrual cycle lasts for 28 days, and this assumption Key Points is typically applied when dating pregnancy. However, there is variability between and within women with regard to the length of the menstrual cycle throughout • Follicular phase length averages 1,11,12 life. A woman who experiences variations of less than 8 13-15 days days between her longest and shortest cycle is considered normal. Irregular cycles are generally • Luteal phase length averages defined as having 8 to 20 days variation in length of 13-14 days1-3 cycle, whereas over 21 days variation in total cycle length is considered very irregular. -

Infertility Investigations for Women
Infertility investigations for women Brooke Building Gynaecology Department 0161 206 5224 © G21031001W. Design Services, Salford Royal NHS Foundation Trust, All Rights Reserved 2021. Document for issue as handout. Unique Identifier: SURG08(21). Review date: May 2023. This booklet is aimed for women undergoing fertility LH (Luteinising Hormone) Progesterone investigations. Its’ aim is to Oligomenorrhoea - When the provide you with some useful periods are occurring three In women, luteinising hormone Progesterone is a female information regarding your or four times a year (LH) is linked to ovarian hormone produced by the hormone production and egg ovaries after ovulation. It investigations. Irregular cycle - Periods that maturation. LH is used to causes the endometrial lining vary in length We hope you !nd this booklet measure a woman’s ovarian of the uterus to get thicker, helpful. The following blood tests are reserve (egg supply). making it receptive for a used to investigate whether You will be advised to have some It causes the follicles to grow, fertilised egg. ovulation (production of an egg) or all of the following tests: mature and release the eggs Progesterone levels increase is occurring each month and also for fertilisation. It reaches its after ovulation, reaching a to help determine which fertility Hormone blood tests highest level (the LH surge) in maximum level seven days treatments to offer. Follicular bloods tests the middle of the menstrual before the start of the next cycle 48 hours prior to ovulation period. The progesterone test is These routine blood tests are FSH (Follicle Stimulating i.e. days 12-14 of a 28 day cycle. -
Understanding Your Menstrual Cycle If You're Trying to Conceive
IS MY PERIOD NORMAL? Understanding Your Menstrual Cycle If You’re Trying to Conceive More than 70% 11% 95% of women have or more of of U.S. women start irregular menstrual American women their periods by cycles as menopause suffer from age 16. approaches. endometriosis.1 10% 12% of U.S. women are of women have affected by PCOS trouble getting or (polycystic ovary staying pregnant.3 syndrome).2 Fortunately, your menstrual cycle can tell you a lot about your fertility if you know what to look for. TYPES OF MENSTRUAL CYCLES Only 15% of About Normal = women have 30% of women are fertile only during 21 to 35 days the “perfect” the “normal” fertility 28-day cycle. window—between days 10 and 17 of the menstrual cycle. Day 1 Period starts (aka menses) 27 28 1 2 26 3 25 4 24 5 Day 15-28 23 6 Day 2-14 Luteal phase; Follicular phase; progesterone** 22 WHAT’S NORMAL? 7 FSH released, (follicle- uterine lining 21 8 stimulating matures Give or take a few days, hormone) and a normal cycle looks like this: estrogen released, 20 9 ovulation* begins 19 10 18 11 17 12 16 15 14 13 *ovulation: the process of an ovum (egg) being released from the ovary; occurs 10-14 days before menses. **progesterone: a steroid hormone that tells the uterus to prepare for pregnancy At least 30% of women have an “irregular” cycle either short, long or inconsistent. Short = Long = < 21 days > 35 days May be a sign of: May be a sign of: Hormonal imbalance Hormonal imbalance Ovaries with fewer eggs Lack of ovulation Approach of menopause Other fertility issues Reduced fertility4 Increased risk of miscarriage SIGNS TO WATCH FOR Your menstrual cycle provides valuable clues about your body’s reproductive health.