Innovation Matters: Pioneering Innovation Today for Health Impact
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dr. Rajiv Shah
Dr. Rajiv Shah leads the efforts of nearly 10,000 staff in more than 70 countries around the world to advance USAID’s mission of ending ex- treme poverty and promoting resilient, democratic societies. Under Dr. Shah’s leadership, USAID has applied innovative technologies Dr. Rajiv Shah and engaged the private sector to solve the world’s most intractable de- velopment challenges. This new model of development brings together an Administrator increasingly diverse community—from large companies to local civil soci- ety groups to communities of faith—to deliver meaningful results. Dr. Shah leads President Obama’s landmark Feed the Future and Power Africa initiatives and has refocused America’s global health partnerships to end preventable child death. Feed the Future, alone, has improved nu- trition for 12 million children and empowered more than 7 million farmers with climate-smart tools they need to grow their way out of extreme pov- erty. In April 2014, USAID launched the U.S. Global Development Lab to harness the expertise of the world’s brightest scientists, students, and entrepreneurs. At the same time, the newly formed Private Capital Group for Development forges a more strategic relationship between private capital and development. Dr. Shah also manages the U.S. Government’s humanitarian response to catastrophic crises around the world, from the devastating 2010 Haiti earthquake to Typhoon Haiyan in the Philippines to the Ebola epidemic in West Africa. Through an extensive set of reforms called “USAID Forward,” Dr. Shah has worked with the United States Congress to transform USAID into the world’s premier development Agency that prioritizes public-private part- nerships, innovation, and meaningful results. -

Global Philanthropy Forum Conference April 18–20 · Washington, Dc
GLOBAL PHILANTHROPY FORUM CONFERENCE APRIL 18–20 · WASHINGTON, DC 2017 Global Philanthropy Forum Conference This book includes transcripts from the plenary sessions and keynote conversations of the 2017 Global Philanthropy Forum Conference. The statements made and views expressed are solely those of the authors and do not necessarily reflect the views of GPF, its participants, World Affairs or any of its funders. Prior to publication, the authors were given the opportunity to review their remarks. Some have made minor adjustments. In general, we have sought to preserve the tone of these panels to give the reader a sense of the Conference. The Conference would not have been possible without the support of our partners and members listed below, as well as the dedication of the wonderful team at World Affairs. Special thanks go to the GPF team—Suzy Antounian, Bayanne Alrawi, Laura Beatty, Noelle Germone, Deidre Graham, Elizabeth Haffa, Mary Hanley, Olivia Heffernan, Tori Hirsch, Meghan Kennedy, DJ Latham, Jarrod Sport, Geena St. Andrew, Marla Stein, Carla Thorson and Anna Wirth—for their work and dedication to the GPF, its community and its mission. STRATEGIC PARTNERS Newman’s Own Foundation USAID The David & Lucile Packard The MasterCard Foundation Foundation Anonymous Skoll Foundation The Rockefeller Foundation Skoll Global Threats Fund Margaret A. Cargill Foundation The Walton Family Foundation Horace W. Goldsmith Foundation The World Bank IFC (International Finance SUPPORTING MEMBERS Corporation) The Leona M. and Harry B. Helmsley Charitable Trust MEMBERS Conrad N. Hilton Foundation Anonymous Humanity United Felipe Medina IDB Omidyar Network Maja Kristin Sall Family Foundation MacArthur Foundation Qatar Foundation International Charles Stewart Mott Foundation The Global Philanthropy Forum is a project of World Affairs. -
Brookings Blum Roundtable
BROOKINGS BLUM ROUNDTABLE FROM AID TO GLOBAL DEVELOPMENT COOPERATION ASPEN, COLORADO AUGUST 3 –5, 2011 Tuesday, August 2, 2011 Arrival and Check-In ROUNDTABLE LOCATION: Lauder Room Koch Seminar Building Aspen Meadows Resort 845 Meadows Road Aspen, Colorado 81611 Telephone: +1-970-925-4240 +1-800-452-4240 1 Wednesday, August 3, 2011 8:00 a.m. – 8:30 a.m. Breakfast Meadows Restaurant 8:40 a.m. – 9:00 a.m. Welcome Lauder Room Koch Seminar Building OPENING REMARKS Richard C. Blum, Blum Capital Partners, LP and Founder of the Blum Center for Developing Economies at Berkeley Mark Suzman, Global Development Program, Bill & Melinda Gates Foundation Kemal Derviş, Global Economy and Development, Brookings STATEMENT OF PURPOSE, SCENE SETTER, AND COMMENTS ON THE AGENDA Homi Kharas, Brookings 9:00 a.m. – 10:30 a.m. Session I Lauder Room Koch Seminar Building REFRAMING DEVELOPMENT COOPERATION Moderator: Walter Isaacson, Aspen Institute In almost any discussion of international development, foreign aid takes center stage. But while aid can certainly be a catalyst for development, it does not work in isolation. Participants will discuss the key objectives of development cooperation, consider what measures of development cooperation are most valuable for recipients, and explore an effective balance of roles and responsibilities - including both public and private players - in today’s evolving development landscape. Introductory Remarks: Owen Barder, Center for Global Development Donald Kaberuka, African Development Bank Group Ananya Roy, University of California, Berkeley Elizabeth Littlefield, Overseas Private Investment Corporation 10:30 a.m. – 10:50 a.m. Break 2 Wednesday, August 3, 2011 10:50 a.m. -

Press Release: UN Secretary General Appoints SUN Lead Group
UNITED NATIONS PRESS RELEASE For immediate release UN Secretary-General Appoints 27 Global Leaders to Head Worldwide Effort to Address Child Malnutrition Heads of State and Other High- Level Representatives to Focus on Improving Nutrition as Key to Progress in Health and Development United Nations, New York, 10 April 2012 – The global Scaling Up Nutrition (SUN) Movement continues to gain momentum today with the convening of 27 leaders committed to advancing the strength and security of nations by improving maternal and child nutrition. This influential group, appointed by UN Secretary-General Ban Ki-moon to represent the many countries, organizations and sectors working to improve nutrition, will serve as strategic guides for this global Movement. “Never before have so many leaders, from so many countries and fields, agreed to work together to improve nutrition,” said Secretary-General Ban Ki-moon. “The Scaling Up Nutrition Movement gives all of us, including the UN, an opportunity to support countries in their efforts to end hunger and malnutrition.” The members of the Lead Group include Heads of State from countries that have prioritized efforts to scale up nutrition, as well as representatives of the donor, civil society, business and UN system organizations that are aligning resources to help SUN countries drive progress. Members of the Lead Group are listed below: additional Members may be invited to join later. The Group’s role is to ensure that the countries at the heart of the Movement are supported as they work to create tangible and sustainable improvements in nutrition. In addition to providing strategic oversight, the Lead Group will help to mobilize support and strengthen both coordination and accountability within the Movement. -

Dr. Rajiv J. Shah, MD, Msc Qualifications & Biography
Dr. Rajiv J. Shah, MD, MSc Qualifications & Biography DR. SHAH IS A RESPECTED LEADER WITH A PROVEN TRACK RECORD IN GLOBAL DEVELOPMENT WITH DEEP EXPERIENCE IN MANY SECTORS, INCLUDING HEALTH, AGRICULTURE, WATER, AND FINANCIAL SERVICES: • He has led and worked with many of the initiatives that are defining best practice in the field of development - The Global Alliance for Vaccines and Immunization, The Global Fund for AIDS, TB and Malaria and The Alliance for a Green Revolution for Africa (AGRA) to name a few. With respect to AGRA in particular, Dr. Shah helped create the organization, build the board, recruit leadership and oversee operations. • He has worked around the world (especially in Africa and Asia), and has deep content and operational experience in global health, agriculture and food security and financial services for the poor. Raj helped launch the Global Development program at the Bill & Melinda Gates Foundation and directly managed the foundation’s nearly $1.3 billion portfolio of investments in agricultural development. He also was the founding director of the Foundation’s Financial Services to the Poor portfolio and held numerous leadership roles within the Foundation Global Health program. Dr. Shah has also helped lead and is an important contributor to President Obama’s global food security initiative. • He has worked closely with many organizations who are key partners to the USAID and its mission. These include the Global Fund for AIDS, TB and Malaria, the Global Alliance for Vaccines and Immunization (GAVI) and a range of innovative public-private partnerships in a variety of sectors in global development. -

The Controversy Over USAID Procurement Reform
AP PHOTO/WALLY SANTANA PHOTO/WALLY AP Is Local Spending Better? The Controversy over USAID Procurement Reform By Casey Dunning November 2013 WWW.AMERICANPROGRESS.ORG Is Local Spending Better? The Controversy over USAID Procurement Reform By Casey Dunning November 2013 Contents 1 Introduction and summary 4 The evolution of USAID’s efforts 28 Tracking the results of USAID’s local procurement reform 31 Recommendations to cement local procurement reform at USAID 36 Conclusion 37 About the author & Acknowledgements 38 Appendix: USAID country presence 39 Endnotes Introduction and summary Procurement reform is not a topic that usually quickens the pulse. But efforts at the U.S. Agency for International Development, or USAID, to utilize other countries’ local governments and organizations to carry out its programs on the ground have triggered a debate that will ultimately affect millions of lives in the years to come. Over the past three years, USAID has undertaken an initiative to direct more of its projects around the globe to local partners in the countries in which it works. The agency has referred to these ongoing reforms under a series of different names, including implementation and procurement reform, or IPR; sustainable partner- ships; and local solutions. Despite the evolving nomenclature, the basic premise of the effort has remained the same: USAID is seeking to directly work with and build the capacity of local governments, civil society, and the private sector in the countries in which it operates. USAID maintains that such a shift will make devel- opment efforts more effective, more enduring, and less costly. USAID began these reforms after recognizing that it was extraordinarily depen- dent on large American for-profit contactors and nongovernmental organi- zations, or NGOs, to carry out its work. -

United G20 Must Pave the Way for Robust Post- COVID-19 Recovery
ISSUE BRIEF United G20 Must Pave the Way for Robust Post- COVID-19 Recovery NOVEMBER 2020 PHIL THORNTON he world is facing unprecedented health and economic crises that require a global solution. Governments have again locked down their economies to contain the mounting death toll from the second wave of the COVID-19 Tpandemic. With this response well underway, now is the time to move into a recovery effort. This will require a coordinated response to the health emergency and a global growth plan that is based on synchronized monetary, fiscal, and debt relief policies. Failure to act will risk a substantial shock to the postwar order established by the United States and its allies more than seventy years ago. The most effective global forum for coordinating this recovery effort is the Group of 20 (G20), which led the way out of the global financial crisis (GFC) in 2009, the closest parallel we have to the current catastrophe. Eleven years ago, world leaders used the G20 meeting in London as the forum to deliver a unified response and a massive fiscal stimulus that helped stem economic free fall and prevented the recession from becoming a second Great Depression. A decade on, it is clear that the G20 is the only body with the clout to save the This report is written and published in global economy. This does not mean that the G20 should be the only forum for accordance with the Atlantic Council actions for its member states. The United States, for example, should also work Policy on Intellectual Independence. -

1 Testimony of Dr. Rajiv Shah Administrator, U.S. Agency
TESTIMONY OF DR. RAJIV SHAH ADMINISTRATOR, U.S. AGENCY FOR INTERNATIONAL DEVELOPMENT FY 2013 BUDGET REQUEST HOUSE APPROPRIATIONS COMMITTEE, SUBCOMMITTEE ON STATE, FOREIGN OPERATIONS, AND RELATED PROGRAMS WASHINGTON, DC MARCH 6, 2012 Thank you Chairwoman Granger, Ranking Member Lowey, and members of the Committee. I am honored to join you to discuss the President’s fiscal year 2013 budget request for USAID. Two years ago, President Obama and Secretary Clinton called for elevating development as a key part of America’s national security and foreign policy. Through both the Presidential Policy Directive on Global Development and the Quadrennial Diplomacy and Development Review, they made the case that the work USAID’s development experts do around the globe was just as vital to America’s global engagement as that of our military and diplomats. The President’s FY 2013 budget request enables USAID to meet the development challenges of our time. It allows us to respond to the dramatic political transformations in the Middle East and North Africa. It helps us focus on our national security priorities in frontline states like Afghanistan, Iraq and Pakistan. And it strengthens economic prosperity, both at home and abroad. This budget also allows us to transform the way we do development. It helps countries feed, treat and educate their people while strengthening their capacity to own those responsibilities for themselves. It helps our development partners increase stability and counter violent extremism. It supports those who struggle for self-determination and democracy and empowers women and girls. And it helps channel development assistance in new directions—toward private sector engagement, scientific research and innovative technologies. -

20110614 Shah Transcript
Department of International Development and International Growth Centre (IGC) public lecture Delivering Meaningful Results in Global Development: A lecture by Dr Raj Shah, Administrator of USAID London School of Economics Tuesday 14 June, 2011 Check against delivery http://www.usaid.gov/press/speeches/2011/sp110614.html WELCOME: Purna Sen, Head of Human Rights, The Commonwealth Secretariat PURNA SEN: Good morning. Good to see you all here. I'm Purna Sen; I'll be chairing the session this morning where we're absolutely delighted to be able to welcome Dr. Rajiv Shah to the LSE. Now, I explained to Dr. Shah this morning that I have a very long bio for him, but I won't go through it all. And I have his permission to miss some bits out. But let me tell you a little about him, and then a little about what he's going to speak to us about this morning. Dr. Shah is the 16th administrator of the U.S. Agency for International Development, a post he took up in December 2009. Previously, he had been an undersecretary for research, education and economics and chief scientist as the U.S. Department of Agriculture. And he was also director of agricultural development at the Global Development Program in the Bill and Melinda Gates Foundation. Prior to that, he was the health care policy advisor for the Gore 2000 presidential campaign and a member of the Pennsylvania government – Governor Ed Rendell's transition committee on health. He is co-founder of the Health Systems Analytics and Project IMPACT for South Asian Americans. -

Strengthening USAID: a Timeline of Recent Events
Strengthening USAID: A Timeline of Recent Events May 31, 2011 - Agricultural development has historically been a significant component of U.S. foreign aid. While in the 1980s 25 percent of U.S. foreign aid went to agriculture, that number dropped to six percent by 1990 and was a meager one percent by 2008.1 As U.S. support for agricultural development has declined, so has the capacity of USAID to deliver agricultural assistance. In 1997, USAID ceased to be an independent agency with the Administrator reporting to the President and was folded into the State Department.2 In 2006, the Secretary of State created a Foreign Assistance Bureau within the State Department (State/F) to more closely align the USAID budget and activities with the State Department’s diplomacy objectives, ending USAID’s budget autonomy. While President G.W. Bush increased the foreign aid budget significantly, the aims of USAID’s development work were anchored in the President’s National Security Strategy. Furthermore, President Bush’s signature development initiatives, such as President’s Emergency Plan for AIDS Relief (PEPFAR) and the Millennium Challenge Corporation (MCC), were placed outside of USAID. Yet the events of the past two years show that the tide may be turning. On the agricultural assistance front, President Obama’s inaugural promise - “To the people of poor nations, we pledge to work alongside you to make your farms flourish…” - launched a renewal of the global agricultural development agenda. This assurance has translated into a series of policy actions: at the G-8 meeting in L’Aquila, Italy, in July 2009, the United States pledged to invest $3.5 billion in food security and agricultural development over three years; the initiative to fulfill this pledge, Feed the Future, was formally launched by the Secretary of State in May 2010 and was highlighted as a signature program when President Obama issued the first-ever Presidential Policy Directive (PPD) for Global Development in September 2010. -
990-PF Or Section 4947(A)(1) Trust Treated As Private Foundation | Do Not Enter Social Security Numbers on This Form As It May Be Made Public
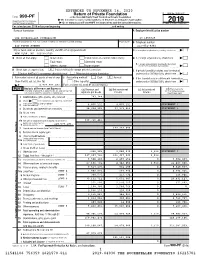
EXTENDED TO NOVEMBER 16, 2020 Return of Private Foundation OMB No. 1545-0047 Form 990-PF or Section 4947(a)(1) Trust Treated as Private Foundation | Do not enter social security numbers on this form as it may be made public. Department of the Treasury 2019 Internal Revenue Service | Go to www.irs.gov/Form990PF for instructions and the latest information. Open to Public Inspection For calendar year 2019 or tax year beginning , and ending Name of foundation A Employer identification number THE ROCKEFELLER FOUNDATION 13-1659629 Number and street (or P.O. box number if mail is not delivered to street address) Room/suite B Telephone number 420 FIFTH AVENUE 212-852-8361 City or town, state or province, country, and ZIP or foreign postal code C If exemption application is pending, check here ~ | NEW YORK, NY 10018-2702 G Check all that apply: Initial return Initial return of a former public charity D 1. Foreign organizations, check here ~~ | Final return Amended return 2. Foreign organizations meeting the 85% test, Address change Name change check here and attach computation ~~~~ | X H Check type of organization: Section 501(c)(3) exempt private foundation E If private foundation status was terminated Section 4947(a)(1) nonexempt charitable trust Other taxable private foundation under section 507(b)(1)(A), check here ~ | X I Fair market value of all assets at end of year J Accounting method: Cash Accrual F If the foundation is in a 60-month termination (from Part II, col. (c), line 16) Other (specify) under section 507(b)(1)(B), check here ~ | | $ 4,929,907,452. -

Rwanda One Health Steering Committee
Republic of Rwanda MINISTRY OF HEALTH ONE HEALTH STRATEGIC PLAN (2014-2018) “No single individual, discipline, sector or ministry can pre-empt and solve complex “health” problems” Rwanda One Health Country Steering Committee. Rubavu, 7th February 2013 Foreword Today, the world is facing numerous challenges that require multi sector and global solutions. One of these challenges is the occurrence and spread of infectious diseases that emerge or re-emerge and have an effect on humans, ecosystem interfaces, wild and domesticated animals. This is mainly attributed to several factors including the exponential growth in human and livestock populations, rapid urbanization, rapidly changing farming systems, closer interaction between livestock and wildlife, forest encroachment, changes in ecosystems, the globalization of trade of animals and their products.. Worldwide, lessons learnt from the prevention and control of Highly Pathogenic Avian Influenza H5N1 highlighted the need to shift to an integrative and holistic approach such as the One Health approach. With increased global human activity on the environment and the global movement of people, increased trading of animals and their products, Rwanda is susceptible to the occurrence and spread of emerging and re-emerging infectious diseases that can have a disastrous on the socio-economic growth. To overcome this challenge, the Ministry of Health in collaboration with other stakeholders developed the Rwanda One Health strategic plan. The One Health Strategic plan reflects shared commitments to enhance collaboration between environmental, animal (wildlife and domestic) and human health, and strengthening the new one health workforce capacity through higher institutions of learning. The strategy also outlines interventions to be undertaken by government institutions and other partners to enhance existing structures and pool together additional resources to prevent and control zoonotic diseases and other events of public health importance.