DIAZEPAM AUTOINJECTOR Rx Only
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Migraine Specialty Care Program Tm
MIGRAINE SPECIALTY CARE PROGRAM TM Phone: 833-796-6470 • Fax: 844-841-3401 Community Led Specialty Pharmacy Care 1 PATIENT INFORMATION: 2 PRESCRIBER INFORMATION: Name: ___________________________________________________ Name: ___________________________________________________ Address: _________________________________________________ Address: _________________________________________________ City: _________________________ State: ____ Zip: ____________ City: _________________________ State: ____ Zip: ____________ Phone: ___________________ Alt. Phone: ____________________ Phone: _____________________ Fax: _______________________ Email: ____________________________________________________ NPI: ________________________ DEA: _______________________ DOB: ___________ Gender: M F Caregiver: _____________ Tax I.D.: __________________________________________________ Height: ________ Weight: ________ Allergies: ________________ Office Contact: __________________ Phone: __________________ 3 STATEMENT OF MEDICAL NECESSITY: (Please Attach All Medical Documentation) Prior Failed Indicate Drug Name v10.0_060821 Length of Symptoms: ___________________________ ICD-10: _________________________ Treatments: and Length of Treatment: Other diagnosis _______________ Number of Migraine Days per month: ________________ Preventative: Headache Days per month: _________________ Migraine Hours per day: __________________ ACE-I/ARBs ___________________ Patient has been evaluated and does not have medication overuse headache? No Yes Antiepileptics ___________________ -

DDT Cover/Back April 2006.Qx
March 2007 Vol 7 No 3 www.drugdeliverytech.com IN THIS ISSUE INTERVIEW WITH DPT’S PRESIDENT MR. PAUL JOHNSON In Situ Gel Systems 30 Mitan Gokulgandhi, BPharm Dharmesh M. Modi, MPharm COX-II Microspheres 38 Lakshmi Sivasubramanian Madhumathi Seshadri Undermining CEO’s 82 John A. Bermingham FEATURING Parkinson’s Disease 59 Steven Damon Yogi R. Patel The science & business of specialty pharma, biotechnology, and drug delivery Specialty Pharma Indices 64 Dr. Barath Christopher Avani Amin, Josef Bossart, PhD Shankar Robinson, PhD Drug Delivery’s PhD Current Status of Clinical Trials Increasing New Ways to Non-Invasive In Asia 68 Importance to Partner With Insulin Delivery Ames Gross, MBA Big Pharma & the Federal Technologies Specialty Pharma Government Momoko Hirose March 2007 Vol 7 No 3 PUBLISHER/PRESIDENT Ralph Vitaro EXECUTIVE EDITORIAL DIRECTOR Dan Marino, MSc [email protected] CREATIVE DIRECTOR Shalamar Q. Eagel CONTROLLER Debbie Carrillo CONTRIBUTING EDITORS Cindy H. Dubin Debra Bingham Jason McKinnie TECHNICAL OPERATIONS Mark Newland EDITORIAL SUPPORT Nicholas D. Vitaro ADMINISTRATIVE SUPPORT Kathleen Kenny Corporate/Editorial Office 219 Changebridge Road, Montville, NJ 07045 Tel: (973)299-1200 Fax: (973) 299-7937 www.drugdeliverytech.com Advertising Sales Offices East & Midwest Victoria Geis - Account Executive Cheryl S. Stratos - Account Executive 103 Oronoco Street, Suite 200 Alexandria, VA 22314 Tel: (703) 212-7735 Fax: (703) 548-3733 E-mail: [email protected] E-mail: [email protected] West Coast Warren -
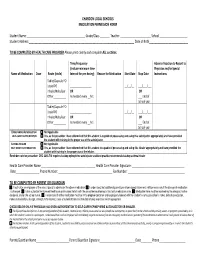
Medication Permission Form
CHARDON LOCAL SCHOOLS MEDICATION PERMISSION FORM Student Name :__________________________________________ Grade/Class _______ Teacher :______________________ School ____________________ Student Address:____________________________________________________________________________ Date of Birth____________________________ TO BE COMPLETED BY HEALTH CARE PROVIDER Please print clearly and complete ALL sections. Time/Frequency Adverse Reaction to Report to (Include minimum time Physician and/or Special Name of Medication Dose Route (circle) Interval for prn dosing) Reason for Medication Start Date Stop Date Instructions Tablet/Capsule PO Liquid PO _________________ __/__/__ ___/___/___ Inhaler/Nebulizer OR OR Other__________ As needed every __hrs. ___ End of School year Tablet/Capsule PO Liquid PO _________________ __/__/__ ___/___/___ Inhaler/Nebulizer OR OR Other__________ As needed every __hrs ___ End of School year EPINEPHRINE AUTOINJECTOR Not Applicable SELF -CARRY AUTHORIZATION Yes, as the prescriber I have determined that this student is capable of possessing and using this autoinjector appropriately and have provided the student with training in the proper use of the autoinjector. ASTHMA INHALER Not Applicable SELF -CARRY AUTHORIZATION Yes, as the prescriber I have determined that this student to capable of possessing and using this inhaler appropriately and have provided the student with training in the proper use of the inhaler. Reminder note for prescriber: ORC 3313.718 requires backup epinephrine autoinjector and best practice recommends backup asthma inhaler Health Care Provider Name _______________________________________ Health Care Provider Signature: ______________________________________ Date_________________ Phone Number: _______________________________________ Fax Number: _________________________________________ TO BE COMPLETED BY PARENT OR GUARDIAN I authorize an employee of the school board to administer the above medication. I understand that additional parent/prescriber signed statements will be necessary if the dosage of medication is changed. -

Instructions For
Instructions for Use Please see page 2 Instructions for Use Please see page 3 SIMPONI® (SIM-po-nee) (golimumab) SIMPONI® (SIM-po-nee) (golimumab) SmartJect® autoinjector Prefilled Syringe SINGLE-DOSE Important Important If your doctor decides that you or a caregiver may be able to give your SIMPONI® injections at home, you should SIMPONI® comes as a single-dose prefilled syringe containing one 50 mg or one 100 mg dose. Each SIMPONI® prefilled receive training on the right way to prepare and inject SIMPONI® using SmartJect®. syringe can only be used one time. Throw away (dispose of) the used prefilled syringe (See Step 3) after one dose, even Do not try to inject SIMPONI® yourself until you have been shown the right way to give the injections by your doctor if there is medicine left in it. Do not reuse your SIMPONI® prefilled syringe. or nurse. If your healthcare provider decides that you or a caregiver may be able to give your injections of SIMPONI® at home, Please read this Instructions for Use before using SIMPONI® SmartJect® and each time you get a refill. There may be you should receive training on the right way to prepare and inject SIMPONI® using the prefilled syringe before new information. This leaflet does not take the place of talking with your doctor about your medical condition or attempting to inject. Do not try to inject yourself until you have been shown the right way to give the injections by your your treatment. healthcare provider. Read this Instructions for Use before using your SIMPONI® prefilled syringe and each time you get a refill. -

New Autoinjector Technology for the Delivery of Subcutaneous Methotrexate in the Treatment of Rheumatoid Arthritis
Expert Review of Medical Devices ISSN: 1743-4440 (Print) 1745-2422 (Online) Journal homepage: http://www.tandfonline.com/loi/ierd20 New autoinjector technology for the delivery of subcutaneous methotrexate in the treatment of rheumatoid arthritis Michael Schiff, Jonathan Jaffe, Bruce Freundlich & Patrick Madsen To cite this article: Michael Schiff, Jonathan Jaffe, Bruce Freundlich & Patrick Madsen (2014) New autoinjector technology for the delivery of subcutaneous methotrexate in the treatment of rheumatoid arthritis, Expert Review of Medical Devices, 11:5, 447-455, DOI: 10.1586/17434440.2014.929492 To link to this article: http://dx.doi.org/10.1586/17434440.2014.929492 Published online: 17 Jun 2014. Submit your article to this journal Article views: 112 View related articles View Crossmark data Citing articles: 1 View citing articles Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ierd20 Download by: [Rosa Weiss] Date: 14 February 2017, At: 10:26 Device Profile New autoinjector technology for the delivery of subcutaneous methotrexate in the treatment of rheumatoid arthritis Expert Rev. Med. Devices 11(5), 447–455 (2014) Michael Schiff*1, Methotrexate (MTX) is the cornerstone of treatment for rheumatoid arthritis (RA), and is Jonathan Jaffe2, widely used both as first-line therapy and as an important component of long-term therapy. Bruce Freundlich3,4 Although subcutaneous MTX is typically delivered orally, parenteral administration offers benefits with respect to tolerability and systemic exposure, and may be an underutilized and Patrick Madsen5 treatment option. The RA patient population presents specific challenges for safe and 1 Department of Rheumatology, accurate administration of parenteral therapies, because of common symptoms of joint pain University of Colorado, Denver, CO, USA and limited manual dexterity. -

From Syringe to Autoinjector
Volume 40 Number 6 Blow-Fill-Seal Data Integrity Using Modular JUNE 2016 Volume 40 Number 6 PLUS: Technology Training Construction PHARMACEUTICAL TECHNOLOGY From Syringe to JUNE 2016 2016 JUNE Autoinjector Building a Better Self-Injection Solution PharmTech.com PEER-REVIEWED Qualifying Personnel to Visually Inspect Cleaned Equipment, Part II SINGLE -USE SYSTEMS FORMULATION API SYNTHESIS & MANUFACTURING Integrating Single-Use Systems Customizing HPMC Adoption of Continuous Processing Advancing Drug Delivery Through Superior Polymer Design Safe and effective delivery of today’s complex drug molecules is increasingly a function of collaboration between polymer experts and pharmaceutical product development teams. Acting on enabling science, producing superior polymer excipient technology, and creating systems for optimum bioavailability, Ashland works alongside formulators to advance drug- specific delivery platforms. Explore how you can solve intricate drug formulation and development challenges with polymer expertise from Ashland. Visit us at Ashland.com/pharmaceutical Come visit us at Booth 610 Ashland [email protected] www.ashland.com/pharmaceutical ®Registered trademark, Ashland or its subsidiaries, registered in various countries ™Trademark, Ashland or its subsidiaries, registered in various countries ©2016, Ashland AD-13475.1 “Off-the-shelf solutions? No thank you. After all, our customers are something special.” Daniel Drossel Mechanical Engineering Technician (Design department) Each customer has its very own special requirements. That’s why we, at Optima, manufacture fi lling lines that are fi ne-tuned to our clients’ particular needs while off ering the benefi ts of an integrated and complete line: The complete machine package including high-precision functionalities, backed by consistent documentation and supported by an optimized and tailored software solution – in addition to a central point of contact who is passionate about your every concern… We are experts in special solutions, after all. -
Access Tier 4 PPO Prescription Drug List CDI Version
Pharmacy | PDL | California 2021 California Access Large Group 4-Tier PPO Prescription Drug List Please note: This Prescription Drug List (PDL) is accurate as of September 1, 2021 and is subject to change after this date. All previous versions of this PDL are no longer in effect. Your estimated coverage and copay/coinsurance may vary based on the benefit plan you choose and the effective date of the plan. This PDL can also be accessed online at myuhc.com > Pharmacy Information > Prescription Drug Lists > California plans > Large Group - Access. Plan-specific coverage documents may be accessed online at uhc.com/statedruglists > Large Group Plans > California. If you are a UnitedHealthcare member, please register or log on to myuhc.com, or call the toll-free number on your health plan ID card to find pharmacy information specific to your benefit plan. This PDL is applicable to the following health insurance products offered by UnitedHealthcare: • Navigate • Navigate Plus • Choice • Choice Plus • Select • Select Plus • Core • Core Essential • Options PPO • Non-Differential PPO Updated 7/13/2021 8/21 © 2021 United HealthCare Services, Inc. All Rights Reserved. WF4335930-A Contents At UnitedHealthcare, we want to help you better understand your medication options. ................................................. 3 How do I use my PDL? .................................................. 4 What are tiers? ........................................................ 5 When does the PDL change? ............................................. 5 Utilization Management Programs ......................................... 6 Your Right to Request Access to a Non-formulary Drug ....................... 6 Requesting a Prior Authorization or Step Therapy Exception ................... 7 How do I locate and fill a prescription through a retail network pharmacy? . 7 How do I locate and fill a prescription through the mail order pharmacy? . -

Diazepam Autoinjector
C-IV DIAZEPAM AUTOINJECTOR DESCRIPTION Rx Only Diazepam injection is a sterile solution packaged within a device that delivers its entire 2 mL contents automatically upon activation. Each mL contains 5 mg diazepam compounded with 40% propylene glycol, 10% ethyl alcohol, 5% sodium benzoate and benzoic acid as buffers, and 1.5% benzyl alcohol as preservative. Diazepam is a benzodiazepine derivative. Chemically, diazepam is 7-chloro- 1,3- dihydro-1-methyl-5-phenyl-2H-1, 4-benzodiazepin-2-one.It is a colorless crystalline compound, insoluble in water and has a molecular weight of 284.74. Its structural formula is as follows: CH 3 O N Cl N CLINICAL PHARMACOLOGY In animals, diazepam appears to act on parts of the limbic system, the thalamus and hypothalamus, and induces calming effects. Diazepam, unlike chlorpromazine and reserpine, has no demonstrable peripheral autonomic blocking action, nor does it produce extrapyramidal side effects. However, animals treated with diazepam do have a transient ataxia at higher doses. Diazepam was found to have transient car- diovascular depressor effects in dogs. Long-term experiments in rats revealed no disturbances of endocrine function. Injections into animals have produced localized irritation of tissue surrounding injection sites and some thickening of veins after intra- venous use. Pharmacokinetics (autoinjector): A study performed in 24 healthy male subjects comparing the I.M. Injection of 10 mg of diazepam in the mid-anterior/lateral thigh by the autoinjector versus 10 mg I.M.by a syringe (operated manually) indicates that the mean percent availability of the drug from the autoinjector is 100% of that obtained from the syringe. -

Amphetamine Extended-Release Orally Disintegrating Tablets (Adzenys XR-ODT)
2.0 CONTACT HOURS 2.0 CONTACT HOURS 6 Abstract: In 2016, the FDA approved several new drugs for use in primary care. These drugs include amphetamine extended-release orally disintegrating tablets (Adzenys XR-ODT), elbasvir and grazoprevir (Zepatier), emtricitabine and tenofovir alafenamide (Descovy), glycopyrrolate and formoterol (Bevespi Aerosphere), insulin degludec injection (Tresiba), and ixekizumab (Taltz). By Lindsy Meadowcraft, PharmD, BCACP, CDE; Geoffrey Mospan, PharmD, BCPS; Taylor Morrisette; Katie Smart; and Melissa Janis of its kind, Adzenys XR-ODT is an extended-release orally ▼ ADHD disintegrating tablet (XR-ODT) that received FDA-approval in January 2016.2,3 This Schedule II drug is manufactured by Amphetamine extended-release Neos Therapeutics, Inc.3 orally disintegrating tablets ■ Indications (Adzenys XR-ODT) Adzenys XR-ODT is indicated in patients age 6 and older for the treatment of ADHD.3 Attention-defi cit hyperactivity disorder (ADHD) is one of the most common neurodevelopmental childhood disorders, of- ■ Mechanism of action ten continuing through adolescence and adulthood.1 The fi rst Adzenys XR-ODT contains immediate-release and central nervous system (CNS) stimulant and amphetamine delayed-release amphetamine. Amphetamines are sympa- Keywords: ADHD, attention-defi cit hyperactivity disorder, chronic obstructive pulmonary disease, COPD, diabetes mellitus, FDA drug approvals, hepatitis C, HIV, new drugs, plaque psoriasis Illustration Oksana Pasishnychenko / Istosk © 20 The Nurse Practitioner • Vol. 41, No. 12 www.tnpj.com Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved. Drug updates and approvals thomimetic amines that stimulate the CNS by increasing ■ Pharmacokinetics the amount of norepinephrine and dopamine within the Adzenys XR-ODT absorption is not affected by food; how- neurons.3 ever, alcohol can potentially increase amphetamine release. -

EMS System for Metropolitan Oklahoma City and Tulsa 2021 Medical Control Board Treatment Protocols
EMS System for Metropolitan Oklahoma City and Tulsa 2021 Medical Control Board Treatment Protocols Approved 9/9/20, Effective 1/15/21, replaces all prior versions 16O – EPINEPHRINE AUTOINJECTOR (EPIPEN®, Auvi-Q®) EMT EMT-INTERMEDIATE 85 ADVANCED EMT PARAMEDIC Class: Vasoconstrictor, Bronchodilator (Catecholamine) Actions/Pharmacodynamics: Stimulates alpha receptors in the peripheral vasculature, producing vasoconstriction-related increases in systemic blood pressure. Stimulates beta-1 receptors in the myocardium, producing increases in heart rate, myocardial contraction, and as a result, cardiac output. Stimulates beta-2 receptors in the lower respiratory tract smooth musculature, producing bronchodilation. Indications: Dyspnea - Asthma (Severe - Refractory to Inhaler/Nebulization) (3C) Acute Allergic Reactions (Anaphylaxis) (8D) Snakebites (Anaphylaxis) (8E) Bee/Wasp Stings (Anaphylaxis) (8F) Contraindications: None in indications above. Pharmacokinetics: Onset of action within 5-10 minutes after IM administration. Duration of effect may range upwards of 30 minutes intramuscularly. Adverse/Side Effects: Restlessness, anxiety, generalized tremors, headache, dizziness, chest pain, palpitations, hypertension, premature ventricular contractions, tachycardia. Pulsatile patients ages 35 years or greater, particularly those with known coronary artery disease, receiving epinephrine should have ECG monitoring initiated and continued as soon as an ECG monitor is available. Safety in pregnancy not firmly established, though when clinically indicated the benefits outweigh risks and should not deter clinically necessary usage. Dosage: Dyspnea - Asthma (Severe - Refractory to Inhaler/Nebulization) - Adult (3C) Acute Allergic Reactions (Anaphylaxis) - Adult (8D) Snakebites (Anaphylaxis) - Adult (8E) Bee/Wasp Stings (Anaphylaxis) - Adult (8F) Adult Epinephrine Autoinjector (0.3 mg of Epinephrine 1mg/mL 1:1000) IM lateral thigh **OLMC Order required if pt ≥ 50 years old, heart illness history, or blood pressure > 140/90 mmHg. -

Hospital Corpsman, Nurse, Or Physician
CHAPTER 4 EMERGENCY MEDICAL CARE PROCEDURES For a Navy Corpsman, the terms “first aid” and against the potential damage caused by premature “emergency medical procedures” relate to the transportation. If you decide to move the victim, do it professional care of the sick and injured before in-depth quickly and gently to a safe location where proper first medical attention can be obtained. Appropriate care aid can be administered. procedures may range from providing an encouraging 3. In a multivictim situation, limit your word to performing a dramatic struggle to draw a person preliminary survey to observing for airway patency, back from the brink of death. Always remember, however, that first aid measures are temporary breathing, and circulation, the ABCs of basic life expedients to save life, to prevent further injury, and to support. Remember, irreversible brain damage can preserve resistance and vitality. These measures are occur within 4 to 6 minutes if breathing has stopped. not meant to replace proper medical diagnosis and Bleeding from a severed artery can lethally drain the treatment procedures. Hospital Corpsmen will be able body in even less time. If both are present and you are to provide the competent care that makes the alone, quickly handle the major hemorrhage first, and difference between life or death, temporary or then work to get oxygen back into the system. Shock permanent injury, and rapid recovery or long-term may allow the rescuer a few minutes of grace but is no disability if they less deadly in the long run. • understand the relationship between first aid and 4. -

2020 Pharmacy Benefits
2020 Pharmacy Benefits 1 Table of Contents Prescription Drug Program ...................................................................................................................................................ii Generic Medications ..............................................................................................................................................................ii Step Therapy ............................................................................................................................................................................ii Prior Authorization Drugs ....................................................................................................................................................iii Once-Daily Medications ......................................................................................................................................................iii Quantity Limits .......................................................................................................................................................................iii Affordable Care Act...............................................................................................................................................................iii Medications Not Covered ....................................................................................................................................................iii Participating Pharmacies ......................................................................................................................................................iv