2020 Preferredrx
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NH Healthy Families Preferred Drug List (PDL) Is the List of Covered Drugs
Pharmacy Program NH Healthy Families is committed to providing appropriate, high quality, and cost effective drug therapy to all NH Healthy Families members. NH Healthy Families works with providers and pharmacists to ensure that medications used to treat a variety of conditions and diseases are covered. NH Healthy Families covers prescription medications and certain over-the-counter (OTC) medications when ordered by a practitioner. The pharmacy program does not cover all medications. Some medications require prior authorization (PA) or have limitations on age, dosage, and maximum quantities. Preferred Drug List The NH Healthy Families Preferred Drug List (PDL) is the list of covered drugs. The PDL applies to drugs members can receive at retail pharmacies. The NH Healthy Families PDL is continually evaluated by the NH Healthy Families Pharmacy and Therapeutics (P&T) Committee to promote the appropriate and cost- effective use of medications. The Committee is composed of the NH Healthy Families Medical Director, NH Healthy Families Pharmacy Director, and several New Hampshire physicians, pharmacists, and other healthcare professionals. Pharmacy Benefit Manager NH Healthy Families works with Envolve Pharmacy Solutions to process pharmacy claims for prescribed drugs. Some drugs on the NH Healthy Families PDL may require PA, and Envolve Pharmacy Solutions is responsible for administering this process. Envolve Pharmacy Solutions is our Pharmacy Benefit Manager (PBM). Specialty Drugs NH Healthy Families contracts with a number of specialty pharmacies, such as AcariaHealth Specialty Pharmacy, to ensure members have adequate access to the specialty drugs they require. Specialty drugs, such as biopharmaceuticals and injectables, may require PA to be approved for payment by NH Healthy Families. -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Migraine Specialty Care Program Tm
MIGRAINE SPECIALTY CARE PROGRAM TM Phone: 833-796-6470 • Fax: 844-841-3401 Community Led Specialty Pharmacy Care 1 PATIENT INFORMATION: 2 PRESCRIBER INFORMATION: Name: ___________________________________________________ Name: ___________________________________________________ Address: _________________________________________________ Address: _________________________________________________ City: _________________________ State: ____ Zip: ____________ City: _________________________ State: ____ Zip: ____________ Phone: ___________________ Alt. Phone: ____________________ Phone: _____________________ Fax: _______________________ Email: ____________________________________________________ NPI: ________________________ DEA: _______________________ DOB: ___________ Gender: M F Caregiver: _____________ Tax I.D.: __________________________________________________ Height: ________ Weight: ________ Allergies: ________________ Office Contact: __________________ Phone: __________________ 3 STATEMENT OF MEDICAL NECESSITY: (Please Attach All Medical Documentation) Prior Failed Indicate Drug Name v10.0_060821 Length of Symptoms: ___________________________ ICD-10: _________________________ Treatments: and Length of Treatment: Other diagnosis _______________ Number of Migraine Days per month: ________________ Preventative: Headache Days per month: _________________ Migraine Hours per day: __________________ ACE-I/ARBs ___________________ Patient has been evaluated and does not have medication overuse headache? No Yes Antiepileptics ___________________ -

Medicines That Affect Fluid Balance in the Body
the bulk of stools by getting them to retain liquid, which encourages the Medicines that affect fluid bowels to push them out. balance in the body Osmotic laxatives e.g. Lactulose, Macrogol - these soften stools by increasing the amount of water released into the bowels, making them easier to pass. Older people are at higher risk of dehydration due to body changes in the ageing process. The risk of dehydration can be increased further when Stimulant laxatives e.g. Senna, Bisacodyl - these stimulate the bowels elderly patients are prescribed medicines for chronic conditions due to old speeding up bowel movements and so less water is absorbed from the age. stool as it passes through the bowels. Some medicines can affect fluid balance in the body and this may result in more water being lost through the kidneys as urine. Stool softener laxatives e.g. Docusate - These can cause more water to The medicines that can increase risk of dehydration are be reabsorbed from the bowel, making the stools softer. listed below. ANTACIDS Antacids are also known to cause dehydration because of the moisture DIURETICS they require when being absorbed by your body. Drinking plenty of water Diuretics are sometimes called 'water tablets' because they can cause you can reduce the dry mouth, stomach cramps and dry skin that is sometimes to pass more urine than usual. They work on the kidneys by increasing the associated with antacids. amount of salt and water that comes out through the urine. Diuretics are often prescribed for heart failure patients and sometimes for patients with The major side effect of antacids containing magnesium is diarrhoea and high blood pressure. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Systematic Review of Tranexamic Acid Adverse Reactions
arm Ph ac f ov l o i a g n il r a n u c o e J Journal of Pharmacovigilance Calapai et al., J Pharmacovigilance 2015, 3:4 ISSN: 2329-6887 DOI: 10.4172/2329-6887.1000171 Review Open Access Systematic Review of Tranexamic Acid Adverse Reactions Gioacchino Calapai2*, Sebastiano Gangemi1, Carmen Mannucci2, Paola Lucia Minciullo1, Marco Casciaro1, Fabrizio Calapai3, Maria Righi4 and Michele Navarra5 1Operative Unit of Allergy and Clinical Immunology, Department of Clinical and Experimental Medicine, University of Messina, Italy 2Department of Clinical and Experimental Medicine, University of Messina, Italy 3Centro Studi Pharma.Ca, Messina, Italy 4Department of Biomedical Sciences and Morphological and Functional Images, University of Messina, Italy 5Department of Drug Sciences and Health Products, University of Messina, Italy *Corresponding author: Gioacchino Calapai, Department of Clinical and Experimental Medicine, University of Messina, Via Consolare Valeria 5, 98125 Messina, Italy, Tel: +39 090 2213646; Fax: +39 090 221; E-mail: [email protected] Received date: July 06, 2015; Accepted date: July 14, 2015; Published date: July 20, 2015 Copyright: © 2015 Calapai G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Background Tranexamic acid is a synthetic lysine derivate that exerts its antifibrinolytic effect by reversible blocking lysine binding sites on plasminogen preventing fibrin degradation. It is widely used for haemorrhage or risk of haemorrhage in increased fibrinolysis or fibrinogenolysis. Aim The aim of our work was to review the literature regarding the best evidence on tranexamic adverse reactions and to describe them according to the apparatus involved. -

DDT Cover/Back April 2006.Qx
March 2007 Vol 7 No 3 www.drugdeliverytech.com IN THIS ISSUE INTERVIEW WITH DPT’S PRESIDENT MR. PAUL JOHNSON In Situ Gel Systems 30 Mitan Gokulgandhi, BPharm Dharmesh M. Modi, MPharm COX-II Microspheres 38 Lakshmi Sivasubramanian Madhumathi Seshadri Undermining CEO’s 82 John A. Bermingham FEATURING Parkinson’s Disease 59 Steven Damon Yogi R. Patel The science & business of specialty pharma, biotechnology, and drug delivery Specialty Pharma Indices 64 Dr. Barath Christopher Avani Amin, Josef Bossart, PhD Shankar Robinson, PhD Drug Delivery’s PhD Current Status of Clinical Trials Increasing New Ways to Non-Invasive In Asia 68 Importance to Partner With Insulin Delivery Ames Gross, MBA Big Pharma & the Federal Technologies Specialty Pharma Government Momoko Hirose March 2007 Vol 7 No 3 PUBLISHER/PRESIDENT Ralph Vitaro EXECUTIVE EDITORIAL DIRECTOR Dan Marino, MSc [email protected] CREATIVE DIRECTOR Shalamar Q. Eagel CONTROLLER Debbie Carrillo CONTRIBUTING EDITORS Cindy H. Dubin Debra Bingham Jason McKinnie TECHNICAL OPERATIONS Mark Newland EDITORIAL SUPPORT Nicholas D. Vitaro ADMINISTRATIVE SUPPORT Kathleen Kenny Corporate/Editorial Office 219 Changebridge Road, Montville, NJ 07045 Tel: (973)299-1200 Fax: (973) 299-7937 www.drugdeliverytech.com Advertising Sales Offices East & Midwest Victoria Geis - Account Executive Cheryl S. Stratos - Account Executive 103 Oronoco Street, Suite 200 Alexandria, VA 22314 Tel: (703) 212-7735 Fax: (703) 548-3733 E-mail: [email protected] E-mail: [email protected] West Coast Warren -

Adverse Reactions to Hallucinogenic Drugs. 1Rnstttutton National Test
DOCUMENT RESUME ED 034 696 SE 007 743 AUTROP Meyer, Roger E. , Fd. TITLE Adverse Reactions to Hallucinogenic Drugs. 1rNSTTTUTTON National Test. of Mental Health (DHEW), Bethesda, Md. PUB DATP Sep 67 NOTE 118p.; Conference held at the National Institute of Mental Health, Chevy Chase, Maryland, September 29, 1967 AVATLABLE FROM Superintendent of Documents, Government Printing Office, Washington, D. C. 20402 ($1.25). FDPS PRICE FDPS Price MFc0.50 HC Not Available from EDRS. DESCPTPTOPS Conference Reports, *Drug Abuse, Health Education, *Lysergic Acid Diethylamide, *Medical Research, *Mental Health IDENTIFIEPS Hallucinogenic Drugs ABSTPACT This reports a conference of psychologists, psychiatrists, geneticists and others concerned with the biological and psychological effects of lysergic acid diethylamide and other hallucinogenic drugs. Clinical data are presented on adverse drug reactions. The difficulty of determining the causes of adverse reactions is discussed, as are different methods of therapy. Data are also presented on the psychological and physiolcgical effects of L.S.D. given as a treatment under controlled medical conditions. Possible genetic effects of L.S.D. and other drugs are discussed on the basis of data from laboratory animals and humans. Also discussed are needs for futher research. The necessity to aviod scare techniques in disseminating information about drugs is emphasized. An aprentlix includes seven background papers reprinted from professional journals, and a bibliography of current articles on the possible genetic effects of drugs. (EB) National Clearinghouse for Mental Health Information VA-w. Alb alb !bAm I.S. MOMS Of NAM MON tMAN IONE Of NMI 105 NUNN NU IN WINES UAWAS RCM NIN 01 NUN N ONMININI 01011110 0. -
Medication Permission Form
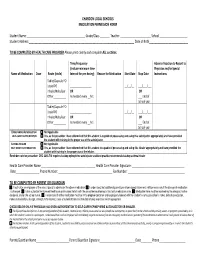
CHARDON LOCAL SCHOOLS MEDICATION PERMISSION FORM Student Name :__________________________________________ Grade/Class _______ Teacher :______________________ School ____________________ Student Address:____________________________________________________________________________ Date of Birth____________________________ TO BE COMPLETED BY HEALTH CARE PROVIDER Please print clearly and complete ALL sections. Time/Frequency Adverse Reaction to Report to (Include minimum time Physician and/or Special Name of Medication Dose Route (circle) Interval for prn dosing) Reason for Medication Start Date Stop Date Instructions Tablet/Capsule PO Liquid PO _________________ __/__/__ ___/___/___ Inhaler/Nebulizer OR OR Other__________ As needed every __hrs. ___ End of School year Tablet/Capsule PO Liquid PO _________________ __/__/__ ___/___/___ Inhaler/Nebulizer OR OR Other__________ As needed every __hrs ___ End of School year EPINEPHRINE AUTOINJECTOR Not Applicable SELF -CARRY AUTHORIZATION Yes, as the prescriber I have determined that this student is capable of possessing and using this autoinjector appropriately and have provided the student with training in the proper use of the autoinjector. ASTHMA INHALER Not Applicable SELF -CARRY AUTHORIZATION Yes, as the prescriber I have determined that this student to capable of possessing and using this inhaler appropriately and have provided the student with training in the proper use of the inhaler. Reminder note for prescriber: ORC 3313.718 requires backup epinephrine autoinjector and best practice recommends backup asthma inhaler Health Care Provider Name _______________________________________ Health Care Provider Signature: ______________________________________ Date_________________ Phone Number: _______________________________________ Fax Number: _________________________________________ TO BE COMPLETED BY PARENT OR GUARDIAN I authorize an employee of the school board to administer the above medication. I understand that additional parent/prescriber signed statements will be necessary if the dosage of medication is changed. -
Hydroxyzine Prescribing Information
Hydroxyzine Hydroxyzine Hydrochloride Hydrochloride Injection, USP Injection, USP (For Intramuscular Use Only) (For Intramuscular Use Only) Rx Only Rx Only DESCRIPTION: Hydroxyzine hydrochloride has the chemical name of (±)-2-[2-[4-( p-Chloro- a- phenylbenzyl)-1-piperazinyl]ethoxy]ethanol dihydrochloride and occurs as a white, odorless powder which is very soluble in water. It has the following structural formula: Molecular Formula: C 21 H27 ClN 2O2•2HCl Molecular Weight: 447.83 Hydroxyzine Hydrochloride Injection, USP is a sterile aqueous solution intended for intramuscular administration. Each mL contains: Hydroxyzine HCl 25 mg or 50 mg, Benzyl Alcohol 0.9%, and Water for Injection q.s. pH adjusted with Sodium Hydroxide and/or Hydrochloric Acid. CLINICAL PHARMACOLOGY: Hydroxyzine hydrochloride is unrelated chemically to phenothiazine, reserpine, and meprobamate. Hydroxyzine has demonstrated its clinical effectiveness in the chemotherapeutic aspect of the total management of neuroses and emotional disturbances manifested by anxiety, tension, agitation, apprehension or confusion. Hydroxyzine has been shown clinically to be a rapid-acting true ataraxic with a wide margin of safety. It induces a calming effect in anxious, tense, psychoneurotic adults and also in anxious, hyperkinetic children without impairing mental alertness. It is not a cortical depressant, but its action may be due to a suppression of activity in certain key regions of the subcortical area of the central nervous system. Primary skeletal muscle relaxation has been demonstrated experimentally. Hydroxyzine has been shown experimentally to have antispasmodic properties, apparently mediated through interference with the mechanism that responds to spasmogenic agents such as serotonin, acetylcholine, and histamine. Antihistaminic effects have been demonstrated experimentally and confirmed clinically. -

The Phytochemistry of Cherokee Aromatic Medicinal Plants
medicines Review The Phytochemistry of Cherokee Aromatic Medicinal Plants William N. Setzer 1,2 1 Department of Chemistry, University of Alabama in Huntsville, Huntsville, AL 35899, USA; [email protected]; Tel.: +1-256-824-6519 2 Aromatic Plant Research Center, 230 N 1200 E, Suite 102, Lehi, UT 84043, USA Received: 25 October 2018; Accepted: 8 November 2018; Published: 12 November 2018 Abstract: Background: Native Americans have had a rich ethnobotanical heritage for treating diseases, ailments, and injuries. Cherokee traditional medicine has provided numerous aromatic and medicinal plants that not only were used by the Cherokee people, but were also adopted for use by European settlers in North America. Methods: The aim of this review was to examine the Cherokee ethnobotanical literature and the published phytochemical investigations on Cherokee medicinal plants and to correlate phytochemical constituents with traditional uses and biological activities. Results: Several Cherokee medicinal plants are still in use today as herbal medicines, including, for example, yarrow (Achillea millefolium), black cohosh (Cimicifuga racemosa), American ginseng (Panax quinquefolius), and blue skullcap (Scutellaria lateriflora). This review presents a summary of the traditional uses, phytochemical constituents, and biological activities of Cherokee aromatic and medicinal plants. Conclusions: The list is not complete, however, as there is still much work needed in phytochemical investigation and pharmacological evaluation of many traditional herbal medicines. Keywords: Cherokee; Native American; traditional herbal medicine; chemical constituents; pharmacology 1. Introduction Natural products have been an important source of medicinal agents throughout history and modern medicine continues to rely on traditional knowledge for treatment of human maladies [1]. Traditional medicines such as Traditional Chinese Medicine [2], Ayurvedic [3], and medicinal plants from Latin America [4] have proven to be rich resources of biologically active compounds and potential new drugs. -

An Insidious Onset of Symptoms Neetu Sakkari, MD, and Tracey Criss, MD
Cases That Test Your Skills An insidious onset of symptoms Neetu Sakkari, MD, and Tracey Criss, MD Ms. S’s depression and anxiety have been well controlled by How would you medication, but after several months, she develops tremors, poor handle this case? Answer the challenge concentration, and confusion. What is causing her symptoms? questions at MDedge.com/ psychiatry and see how your colleagues responded CASE Tremors, increasing anxiety presentation and similarity to other syn- Ms. S, age 56, has a history of depression and dromes such as NMS, serotonin syndrome anxiety. Previously, she tried several selec- often is undiagnosed.5 tive serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibi- tors (SNRIs), which failed to treat her symp- TREATMENT Discontinue fluoxetine toms. Ms. S is switched from duloxetine, 120 Several months after the fluoxetine increase, mg/d, to fluoxetine, 20 mg/d, while continu- Ms. S’s physical symptoms emerge. Several ing bupropion, 150 mg/d, and gabapentin, weeks later, she notices significant hyper- 600 mg/d. She tolerates fluoxetine well, but 5 tension of 162/102 mm Hg by checking her months later, she requests a dosage increase blood pressure at home. She had no history because her depressive and anxious symp- of hypertension before taking fluoxetine. toms re-emerge. Fluoxetine is increased to She then tells her psychiatrist she has been 40 mg/d. experiencing confusion, shakiness, loss of balance, forgetfulness, joint pain, sweating, and fatigue, along with worsening anxiety. The authors’ observations The treatment team makes a diagnosis of The incidence of serotonin syndrome has serotonin syndrome and recommends dis- increased because of increasing use of sero- continuing fluoxetine and starting cyprohep- tonergic agents.1-3 Although the severity tadine, 4 mg initially, and then repeating the could range from benign to life-threatening, cyproheptadine dose in several hours if her the potential lethality combined with dif- symptoms do not resolve.