Treatment After Accidental Injection With
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Using Rheology Measurement As a Potentially Predictive Tool for Solder Paste Transfer Efficiency and Print Volume Consistency
USING RHEOLOGY MEASUREMENT AS A POTENTIALLY PREDICTIVE TOOL FOR SOLDER PASTE TRANSFER EFFICIENCY AND PRINT VOLUME CONSISTENCY Mitch Holtzer, Karen Tellefsen and Westin Bent Alpha Assembly Solutions South Plainfield, NJ, USA [email protected] ABSTRACT Commercially available solder pastes use an upper and Industry standards such as J-STD-005 and JIS Z 3284-1994 lower limit for viscosity. Generally, this viscosity is call for the use of viscosity measurement(s) as a quality measured at one shear rate, typically the shear associated assurance test method for solder paste. Almost all solder with a spiral viscometer rotating at 10 revolutions per paste produced and sold use a viscosity range at a single minute (RPM). If the powder contained in solder paste is shear rate as part of the pass fail criteria for shipment and dissolved by the acid activator in the solder paste flux, the customer acceptance respectively. viscosity of the solder paste will quickly increase. If the viscosity increases more than 20 to 30% above the upper As had been reported many times, an estimated 80% of the limit of the specification, poor printing results will be highly defects associated with the surface mount technology likely. The solder paste will not roll evenly over the stencil process involve defects created during the printing process. and apertures in the stencil will remain unfilled, causing Viscosity at a single shear rate could predict a fatal flaw in skips in the paste printing pattern. the printability of a solder paste sample. However, false positive single shear rate viscosity readings are not The purpose of the study was to determine if there is a unknown. -

Migraine Specialty Care Program Tm
MIGRAINE SPECIALTY CARE PROGRAM TM Phone: 833-796-6470 • Fax: 844-841-3401 Community Led Specialty Pharmacy Care 1 PATIENT INFORMATION: 2 PRESCRIBER INFORMATION: Name: ___________________________________________________ Name: ___________________________________________________ Address: _________________________________________________ Address: _________________________________________________ City: _________________________ State: ____ Zip: ____________ City: _________________________ State: ____ Zip: ____________ Phone: ___________________ Alt. Phone: ____________________ Phone: _____________________ Fax: _______________________ Email: ____________________________________________________ NPI: ________________________ DEA: _______________________ DOB: ___________ Gender: M F Caregiver: _____________ Tax I.D.: __________________________________________________ Height: ________ Weight: ________ Allergies: ________________ Office Contact: __________________ Phone: __________________ 3 STATEMENT OF MEDICAL NECESSITY: (Please Attach All Medical Documentation) Prior Failed Indicate Drug Name v10.0_060821 Length of Symptoms: ___________________________ ICD-10: _________________________ Treatments: and Length of Treatment: Other diagnosis _______________ Number of Migraine Days per month: ________________ Preventative: Headache Days per month: _________________ Migraine Hours per day: __________________ ACE-I/ARBs ___________________ Patient has been evaluated and does not have medication overuse headache? No Yes Antiepileptics ___________________ -

Dispensing Solder Paste with a Noflex™ Linear Drive System
AIRFREE™ WHITE PAPER LDS9000 VS. AUGER VALVE DISPENSERS Dispensing Solder Paste with a NoFlex™ Linear Drive System By: Scott Beebe, President of Fishman Corporation While the limitations of pneumatics in dispensing solder paste are well understood, higher board densities and smaller dot sizes are also challenging the performance abilities of more advanced types of dispensers, such as auger valves. AirFreeTM Linear Drive technology offers promising benefits, including significant savings in material cost and high repeatability without concern for viscosity and the volume of paste remaining in the syringe. The process of dispensing solder paste began with pneumatics. Whether a hand-held gun, or an automated workstation, whether a diaphragm, spool, needle, or piston, such dispensers depend on a column of air under pressure to force material through a dispensing tip and onto a substrate. Heat, moisture, fluctuations in air pressure, contamination, changes in viscosity... all undermine the ability of air-driven dispensers to deliver prescribed amounts of solder paste consistently, especially in the small amounts required by high density electronic circuitry (typically, less than a milligram). While pneumatic dispensers were at one time the only method available for hand-held and automatic dispensing of solder paste, the demand for precise volume control and repeatability led to the development of alternative solutions in dispensing, the most notable being the auger valve. Unfortunately, auger valves have limitations. Linear Drive technology, however, isunique, in that the amount of solder paste delivered—dot after dot after dot—is consistent, by design, and is unaffected by either changes in viscosity (Figure 1) or the amount of paste left in the syringe.* Moreover, cost savings can be substantial due to the ability to pre-package syringes with larger amounts of paste than is possible with other types of dispensers. -

DDT Cover/Back April 2006.Qx
March 2007 Vol 7 No 3 www.drugdeliverytech.com IN THIS ISSUE INTERVIEW WITH DPT’S PRESIDENT MR. PAUL JOHNSON In Situ Gel Systems 30 Mitan Gokulgandhi, BPharm Dharmesh M. Modi, MPharm COX-II Microspheres 38 Lakshmi Sivasubramanian Madhumathi Seshadri Undermining CEO’s 82 John A. Bermingham FEATURING Parkinson’s Disease 59 Steven Damon Yogi R. Patel The science & business of specialty pharma, biotechnology, and drug delivery Specialty Pharma Indices 64 Dr. Barath Christopher Avani Amin, Josef Bossart, PhD Shankar Robinson, PhD Drug Delivery’s PhD Current Status of Clinical Trials Increasing New Ways to Non-Invasive In Asia 68 Importance to Partner With Insulin Delivery Ames Gross, MBA Big Pharma & the Federal Technologies Specialty Pharma Government Momoko Hirose March 2007 Vol 7 No 3 PUBLISHER/PRESIDENT Ralph Vitaro EXECUTIVE EDITORIAL DIRECTOR Dan Marino, MSc [email protected] CREATIVE DIRECTOR Shalamar Q. Eagel CONTROLLER Debbie Carrillo CONTRIBUTING EDITORS Cindy H. Dubin Debra Bingham Jason McKinnie TECHNICAL OPERATIONS Mark Newland EDITORIAL SUPPORT Nicholas D. Vitaro ADMINISTRATIVE SUPPORT Kathleen Kenny Corporate/Editorial Office 219 Changebridge Road, Montville, NJ 07045 Tel: (973)299-1200 Fax: (973) 299-7937 www.drugdeliverytech.com Advertising Sales Offices East & Midwest Victoria Geis - Account Executive Cheryl S. Stratos - Account Executive 103 Oronoco Street, Suite 200 Alexandria, VA 22314 Tel: (703) 212-7735 Fax: (703) 548-3733 E-mail: [email protected] E-mail: [email protected] West Coast Warren -
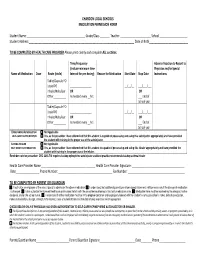
Medication Permission Form
CHARDON LOCAL SCHOOLS MEDICATION PERMISSION FORM Student Name :__________________________________________ Grade/Class _______ Teacher :______________________ School ____________________ Student Address:____________________________________________________________________________ Date of Birth____________________________ TO BE COMPLETED BY HEALTH CARE PROVIDER Please print clearly and complete ALL sections. Time/Frequency Adverse Reaction to Report to (Include minimum time Physician and/or Special Name of Medication Dose Route (circle) Interval for prn dosing) Reason for Medication Start Date Stop Date Instructions Tablet/Capsule PO Liquid PO _________________ __/__/__ ___/___/___ Inhaler/Nebulizer OR OR Other__________ As needed every __hrs. ___ End of School year Tablet/Capsule PO Liquid PO _________________ __/__/__ ___/___/___ Inhaler/Nebulizer OR OR Other__________ As needed every __hrs ___ End of School year EPINEPHRINE AUTOINJECTOR Not Applicable SELF -CARRY AUTHORIZATION Yes, as the prescriber I have determined that this student is capable of possessing and using this autoinjector appropriately and have provided the student with training in the proper use of the autoinjector. ASTHMA INHALER Not Applicable SELF -CARRY AUTHORIZATION Yes, as the prescriber I have determined that this student to capable of possessing and using this inhaler appropriately and have provided the student with training in the proper use of the inhaler. Reminder note for prescriber: ORC 3313.718 requires backup epinephrine autoinjector and best practice recommends backup asthma inhaler Health Care Provider Name _______________________________________ Health Care Provider Signature: ______________________________________ Date_________________ Phone Number: _______________________________________ Fax Number: _________________________________________ TO BE COMPLETED BY PARENT OR GUARDIAN I authorize an employee of the school board to administer the above medication. I understand that additional parent/prescriber signed statements will be necessary if the dosage of medication is changed. -

Making Dry Eyes Ancient History: Egypt, Mesopotamia, India, China, Greece and Rome
Making Dry Eyes Ancient History: Egypt, Mesopotamia, India, China, Greece and Rome Cheryl Lynn Bergin, OD Author’s Bio Dr. Bergin teaches Anatomy and Physiology at St. Louis Community College. She writes about systemic nutrition, ocular nutrition and the ocular effects of eating disorders. She is a member of the Optometric (Ocular) Nutrition and Optometric Historical Societies. Photo by Stan Trampe ________________________________________________________________________________ Dry eyes are not a new condition, but one might think that the case. A literature search for “dry eye” rarely reveals anything before 1970. One must be an ocular archeologist to discover how the ancients treated “irritated” eyes, dried by the harsh conditions of the desert sun and sand. EGYPT: In 1872, Georg Ebers, a German Egyptologist and novelist, discovered a collection of Egyptian medicinal recipes later called the Ebers Papyrus. The papyrus also contains ancient ophthalmic treatments. Ebers selected the important chapters on ocular diseases, translated them and added explanatory remarks. Written between 1553 and 1550 BC (1,000 years before Hippocrates), this is the oldest book on medicine (perhaps the medical textbook of ancient Egypt). It is similar to the Greek manuscripts about folk medicine that can be found among the collection of Galen and Oribasius, as well as among the manuscripts of Dioscorides. According to Ebers Papyrus, “The water within,” i.e., tear fluid and mucous secretion, is treated with incense, myrrh, and lead salt.”6,9 EGYPTIAN EYE MAKE-UP: Liz Taylor as Cleopatra16 The ancient Egyptian’s eye make-up was not just stunning, it was functional. It helped alleviate irritation from the sun’s glare off the desert sand and even prevented eye infections. -

The Role of Epinephrine in the Treatment of Anaphylaxis Anne K
The Role of Epinephrine in the Treatment of Anaphylaxis Anne K. Ellis, MD, and James H. Day, MD, FRCP(C) Address Beneficial Effects of Epinephrine Division of Allergy, Kingston General Hospital, 76 Stuart Street, in Anaphylaxis Kingston, ON K7L 2V7, Canada. Epinephrine is both an alpha (α) and a beta (β) adrener- E-mail: [email protected] gic receptor agonist. Through α-adrenergic stimulation, Current Allergy and Asthma Reports 2003, 3:11–14 epinephrine increases peripheral vascular resistance, Current Science Inc. ISSN 1529-7322 Copyright © 2003 by Current Science Inc. improving blood pressure and coronary artery perfusion, reversing peripheral vasodilation, and decreasing angioedema and urticaria [5]. β-1 adrenergic stimulation Epinephrine is the cornerstone of anaphylaxis manage- has positive inotropic and chronotropic effects on the ment. Its administration should be immediate upon evi- myocardium, and β-2 adrenergic effects include bron- dence of the occurrence of anaphylaxis. Delays in chodilation [6]. β-adrenergic receptors also increase administration may be fatal. The most appropriate admin- intracellular cyclic adenosine monophosphate (cAMP) istration is 0.3 to 0.5 mL of 1:1000 dilution intramuscu- production in mast cells and basophils, which inhibits larly for adults and 0.01 mg/kg for children, given in the further inflammatory mediator release [7,8]. lateral thigh. Patients with known anaphylactic reactivity should be prescribed an epinephrine auto-injector to be carried at all times for treatment of potential recur- Dosage and Routes of Administration rences. Education of the patient or parent regarding the for Epinephrine proper use of this tool is paramount. Some discrepancy exists in the literature concerning the appropriate dosage of epinephrine for anaphylaxis. -

Guideline (S2k) on Acute Therapy and Management of Anaphylaxis: 2021 Update
guidelines Allergo J Int (2021) 30:1–25 https://doi.org/10.1007/s40629-020-00158-y Guideline (S2k) on acute therapy and management of anaphylaxis: 2021 update S2k-Guideline of the German Society for Allergology and Clinical Immunology (DGAKI), the Medical Association of German Allergologists (AeDA), the Society of Pediatric Allergology and Environmental Medicine (GPA), the German Academy of Allergology and Environmental Medicine (DAAU), the German Professional Association of Pediatricians (BVKJ), the Society for Neonatology and Pediatric Intensive Care (GNPI), the German Society of Dermatology (DDG), the Austrian Society for Allergology and Immunology (ÖGAI), the Swiss Society for Allergy and Immunology (SGAI), the German Society of Anaesthesiology and Intensive Care Medicine (DGAI), the German Society of Pharmacology (DGP), the German Respiratory Society (DGP), the patient organization German Allergy and Asthma Association (DAAB), the German Working Group of Anaphylaxis Training and Education (AGATE) Johannes Ring · Kirsten Beyer · Tilo Biedermann · Andreas Bircher · Matthias Fischer · Thomas Fuchs · Axel Heller · Florian Hoffmann · Isidor Huttegger · Thilo Jakob · Ludger Klimek · Matthias V. Kopp · Claudia Kugler · Lars Lange · Oliver Pfaar · Ernst Rietschel · Franziska Rueff · Sabine Schnadt · Roland Seifert · Britta Stöcker · Regina Treudler · Christian Vogelberg · Thomas Werfel · Margitta Worm · Helmut Sitter · Knut Brockow Published online: 28 January 2021 © The Author(s) 2021 Keywords Anaphylaxis · Food allergy · Drug LT Leukotriene -

Instructions For
Instructions for Use Please see page 2 Instructions for Use Please see page 3 SIMPONI® (SIM-po-nee) (golimumab) SIMPONI® (SIM-po-nee) (golimumab) SmartJect® autoinjector Prefilled Syringe SINGLE-DOSE Important Important If your doctor decides that you or a caregiver may be able to give your SIMPONI® injections at home, you should SIMPONI® comes as a single-dose prefilled syringe containing one 50 mg or one 100 mg dose. Each SIMPONI® prefilled receive training on the right way to prepare and inject SIMPONI® using SmartJect®. syringe can only be used one time. Throw away (dispose of) the used prefilled syringe (See Step 3) after one dose, even Do not try to inject SIMPONI® yourself until you have been shown the right way to give the injections by your doctor if there is medicine left in it. Do not reuse your SIMPONI® prefilled syringe. or nurse. If your healthcare provider decides that you or a caregiver may be able to give your injections of SIMPONI® at home, Please read this Instructions for Use before using SIMPONI® SmartJect® and each time you get a refill. There may be you should receive training on the right way to prepare and inject SIMPONI® using the prefilled syringe before new information. This leaflet does not take the place of talking with your doctor about your medical condition or attempting to inject. Do not try to inject yourself until you have been shown the right way to give the injections by your your treatment. healthcare provider. Read this Instructions for Use before using your SIMPONI® prefilled syringe and each time you get a refill. -

Mutasem Rawas.Qalaji
FORMULATION AND ASSESSMENT OF FAST- DISINTEGRATING SUBLINGUAL EPINEPHRINE TABLETS FOR TI.IE POTENTIAI- EMERGENCY TREATMENT OF ANAPHYLAXIS By MUTASEM RAWAS.QALAJI A THESIS SUBMITTED TO THE FACULTY OF GRADUATE STUDIES IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY FACULTY OF PHARMACY UNIVERSITY OF MANITOBA WINNIPEG, MANITOBA, CANADA JUNE, 2006 THE UNIVERSITY OF MANITOBA FACULTY OF GRADUATE STUDIES COPYRIGHT PERMISSION Formulation and Assessment of Fast-Disintegrating Sublingual Epinephrine Tablets for the Potential Emergency Treatment of Anaphylaxis By Mutasem Rawas-Qalaji A Thesis/Practicum submitted to the Faculty of Graduate Studies of The University of Manitoba in partial fïlfitlment of the requirement of the degree of Doctor of Philosophy Mutasem Rawas-Qalaji @ 2006 Permission has been granted to the Library of the University of Manitoba to lend or sell copies of this thesis/practicum, to the National Library of Canada to microfilm this thesis and to lend or sell copies of the film, and to University Microfilms Inc. to publish an abstract of this thesis/practicum. This reproduction or copy of this thesis has been made available by authority of the copyright owner solely for the purpose of private study and research, and may only be reproduced and copied as permitted by copyright laws or with express written authorization from the copyright o\ilner. DEDICATION To my father Mohamad Rawas-ealaji and my mother wedad Duqsi (in memoriam) lwould like to dedicate this work. ABSTRACT Objectives; To formulate, characterize, and evaluate the stability of sublingual (sL) epinephrine (E) tablets that are bioequivatent to E 0.3 mg intramuscular injection (lM) for the feasibility of SL E administration for the potential out-of-hospital emergency treatment of anaphylaxis. -

2019 Express Scripts National Preferred Formulary
The following is a list of the most commonly prescribed drugs. It represents an abbreviated version of the drug list (formulary) that is at the core of your prescription plan. The list is not all-inclusive and does not guarantee coverage. In addition to using this list, you are encouraged to ask your doctor to prescribe generic drugs whenever appropriate. 2019 Express Scripts PLEASE NOTE: Brand-name drugs may move to nonformulary status if a generic version becomes available during the year. Not all the drugs listed are covered by National Preferred Formulary all prescription plans; check your benefit materials for the specific drugs covered and the copayments for your prescription plan. For specific questions about your coverage, please call the phone number printed on your member ID card. KEY BD AUTOSHIELD clonidine enalapril GENOTROPIN [INJ] [INJ] - Injectable Drug DUO NEEDLES clopidogrel ENBREL [INJ] GENVOYA Brand-name drugs are listed BD ULTRAFINE clotrimazole/betamethasone enoxaparin [INJ] GILENYA in CAPITAL letters. INSULIN SYRINGES dipropionate ENSTILAR GILOTRIF Generic drugs are listed BD ULTRAFINE PEN NEEDLES COLCRYS ENTRESTO glimepiride in lower case letters. BELBUCA COMBIGAN EPCLUSA glipizide benazepril COMBIPATCH EPIDIOLEX glipizide ext-release A benzonatate COMBIVENT RESPIMAT EPIDUO FORTE GLUCAGEN [INJ] BEPREVE COPAXONE 40 MG [INJ] epinephrine autoinjector GLUCAGON [INJ] ABILIFY MAINTENA [INJ] BETASERON [INJ] CORLANOR (by Mylan) [INJ] glyburide ABSORICA BETHKIS COSENTYX [INJ] EPIPEN, EPIPEN JR [INJ] GLYXAMBI ACANYA BEVESPI -

Pharmacy Laws on Epinephrine Autoinjectors
Pharmacy Laws on Epinephrine Autoinjectors Updated 1/13/2020 Ohio has several laws intended to promote the accessibility of epinephrine autoinjectors. This document will provide a general overview of the following laws: . Section 4729.382 - Pharmacist's authority to dispense an epinephrine autoinjector by substitution. Section 4729.47 - Authority to dispense epinephrine without a prescription (FAQ starts on page 5 of this document). For questions regarding either provision, please review the following frequently asked questions. If you need additional information, the most expedient way to have your questions answered will be to e-mail the Board office by visiting: http://www.pharmacy.ohio.gov/contact.aspx. Section 4729.382 - Pharmacist's authority to dispense an epinephrine autoinjector by substitution. Section 4729.382 of the Ohio Revised Code expands a pharmacist’s ability to substitute epinephrine autoinjectors. NOTE: Nothing in this provision applies to the following: . Generic substitution of products deemed as being therapeutically equivalent in the FDA Orange Book and in accordance with section 4729.38 of the Revised Code; or . Obtaining a new verbal prescription from a prescriber for a different epinephrine autoinjector. Q1) Under what circumstances am I permitted to substitute the prescribed autoinjector? In addition to generic substitution (i.e. an AB rating in the Orange Book), epinephrine autoinjector substitution may occur if the form of epinephrine in the dispensed autoinjector, when compared to the form of the drug in the prescribed autoinjector, complies with all the following: 1. Is a pharmaceutical equivalent of the form of epinephrine in the type of autoinjector that was prescribed in that it contains identical amounts of the identical active ingredients, but not necessarily the same inactive ingredients.