Immunogenicity Is Preferentially Induced in Sparse Dendritic Cell
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanisms of Immunothrombosis in Vaccine-Induced Thrombotic Thrombocytopenia (VITT) Compared to Natural SARS-Cov-2 Infection
Journal of Autoimmunity 121 (2021) 102662 Contents lists available at ScienceDirect Journal of Autoimmunity journal homepage: www.elsevier.com/locate/jautimm Mechanisms of Immunothrombosis in Vaccine-Induced Thrombotic Thrombocytopenia (VITT) Compared to Natural SARS-CoV-2 Infection Dennis McGonagle a,b, Gabriele De Marco a, Charles Bridgewood a,* a Leeds Institute of Rheumatic and Musculoskeletal Medicine (LIRMM), University of Leeds, Leeds, UK b National Institute for Health Research (NIHR) Leeds Biomedical Research Centre (BRC), Leeds Teaching Hospitals, Leeds, UK ARTICLE INFO ABSTRACT Keywords: Herein, we consider venous immunothrombotic mechanisms in SARS-CoV-2 infection and anti-SARS-CoV-2 DNA COVID-19 pneumonia related thrombosis vaccination. Primary SARS-CoV-2 infection with systemic viral RNA release (RNAaemia) contributes to innate Vaccine induced thrombotic thrombocytopenia immune coagulation cascade activation, with both pulmonary and systemic immunothrombosis - including (VITT) venous territory strokes. However, anti-SARS-CoV-2 adenoviral-vectored-DNA vaccines -initially shown for the Heparin induced thrombocytopenia (HIT) ChAdOx1 vaccine-may rarely exhibit autoimmunity with autoantibodies to Platelet Factor-4 (PF4) that is termed DNA-PF4 interactions. VITT model Vaccine-Induced Thrombotic Thrombocytopenia (VITT), an entity pathophysiologically similar to Heparin- Induced Thrombocytopenia (HIT). The PF4 autoantigen is a polyanion molecule capable of independent in teractions with negatively charged bacterial cellular wall, heparin and DNA molecules, thus linking intravascular innate immunity to both bacterial cell walls and pathogen-derived DNA. Crucially, negatively charged extra cellular DNA is a powerful adjuvant that can break tolerance to positively charged nuclear histone proteins in many experimental autoimmunity settings, including SLE and scleroderma. Analogous to DNA-histone inter actons, positively charged PF4-DNA complexes stimulate strong interferon responses via Toll-Like Receptor (TLR) 9 engagement. -

Critical Role of CXCL4 in the Lung Pathogenesis of Influenza (H1N1) Respiratory Infection
ARTICLES Critical role of CXCL4 in the lung pathogenesis of influenza (H1N1) respiratory infection L Guo1,3, K Feng1,3, YC Wang1,3, JJ Mei1,2, RT Ning1, HW Zheng1, JJ Wang1, GS Worthen2, X Wang1, J Song1,QHLi1 and LD Liu1 Annual epidemics and unexpected pandemics of influenza are threats to human health. Lung immune and inflammatory responses, such as those induced by respiratory infection influenza virus, determine the outcome of pulmonary pathogenesis. Platelet-derived chemokine (C-X-C motif) ligand 4 (CXCL4) has an immunoregulatory role in inflammatory diseases. Here we show that CXCL4 is associated with pulmonary influenza infection and has a critical role in protecting mice from fatal H1N1 virus respiratory infection. CXCL4 knockout resulted in diminished viral clearance from the lung and decreased lung inflammation during early infection but more severe lung pathology relative to wild-type mice during late infection. Additionally, CXCL4 deficiency decreased leukocyte accumulation in the infected lung with markedly decreased neutrophil infiltration into the lung during early infection and extensive leukocyte, especially lymphocyte accumulation at the late infection stage. Loss of CXCL4 did not affect the activation of adaptive immune T and B lymphocytes during the late stage of lung infection. Further study revealed that CXCL4 deficiency inhibited neutrophil recruitment to the infected mouse lung. Thus the above results identify CXCL4 as a vital immunoregulatory chemokine essential for protecting mice against influenza A virus infection, especially as it affects the development of lung injury and neutrophil mobilization to the inflamed lung. INTRODUCTION necrosis factor (TNF)-a, interleukin (IL)-6, and IL-1b, to exert Influenza A virus (IAV) infections cause respiratory diseases in further antiviral innate immune effects.2 Meanwhile, the innate large populations worldwide every year and result in seasonal immune cells act as antigen-presenting cells and release influenza epidemics and unexpected pandemic. -

Inflammatory Modulation of Hematopoietic Stem Cells by Magnetic Resonance Imaging
Electronic Supplementary Material (ESI) for RSC Advances. This journal is © The Royal Society of Chemistry 2014 Inflammatory modulation of hematopoietic stem cells by Magnetic Resonance Imaging (MRI)-detectable nanoparticles Sezin Aday1,2*, Jose Paiva1,2*, Susana Sousa2, Renata S.M. Gomes3, Susana Pedreiro4, Po-Wah So5, Carolyn Ann Carr6, Lowri Cochlin7, Ana Catarina Gomes2, Artur Paiva4, Lino Ferreira1,2 1CNC-Center for Neurosciences and Cell Biology, University of Coimbra, Coimbra, Portugal, 2Biocant, Biotechnology Innovation Center, Cantanhede, Portugal, 3King’s BHF Centre of Excellence, Cardiovascular Proteomics, King’s College London, London, UK, 4Centro de Histocompatibilidade do Centro, Coimbra, Portugal, 5Department of Neuroimaging, Institute of Psychiatry, King's College London, London, UK, 6Cardiac Metabolism Research Group, Department of Physiology, Anatomy & Genetics, University of Oxford, UK, 7PulseTeq Limited, Chobham, Surrey, UK. *These authors contributed equally to this work. #Correspondence to Lino Ferreira ([email protected]). Experimental Section Preparation and characterization of NP210-PFCE. PLGA (Resomers 502 H; 50:50 lactic acid: glycolic acid) (Boehringer Ingelheim) was covalently conjugated to fluoresceinamine (Sigma- Aldrich) according to a protocol reported elsewhere1. NPs were prepared by dissolving PLGA (100 mg) in a solution of propylene carbonate (5 mL, Sigma). PLGA solution was mixed with perfluoro- 15-crown-5-ether (PFCE) (178 mg) (Fluorochem, UK) dissolved in trifluoroethanol (1 mL, Sigma). This solution was then added to a PVA solution (10 mL, 1% w/v in water) dropwise and stirred for 3 h. The NPs were then transferred to a dialysis membrane and dialysed (MWCO of 50 kDa, Spectrum Labs) against distilled water before freeze-drying. Then, NPs were coated with protamine sulfate (PS). -

Development and Validation of a Protein-Based Risk Score for Cardiovascular Outcomes Among Patients with Stable Coronary Heart Disease
Supplementary Online Content Ganz P, Heidecker B, Hveem K, et al. Development and validation of a protein-based risk score for cardiovascular outcomes among patients with stable coronary heart disease. JAMA. doi: 10.1001/jama.2016.5951 eTable 1. List of 1130 Proteins Measured by Somalogic’s Modified Aptamer-Based Proteomic Assay eTable 2. Coefficients for Weibull Recalibration Model Applied to 9-Protein Model eFigure 1. Median Protein Levels in Derivation and Validation Cohort eTable 3. Coefficients for the Recalibration Model Applied to Refit Framingham eFigure 2. Calibration Plots for the Refit Framingham Model eTable 4. List of 200 Proteins Associated With the Risk of MI, Stroke, Heart Failure, and Death eFigure 3. Hazard Ratios of Lasso Selected Proteins for Primary End Point of MI, Stroke, Heart Failure, and Death eFigure 4. 9-Protein Prognostic Model Hazard Ratios Adjusted for Framingham Variables eFigure 5. 9-Protein Risk Scores by Event Type This supplementary material has been provided by the authors to give readers additional information about their work. Downloaded From: https://jamanetwork.com/ on 10/02/2021 Supplemental Material Table of Contents 1 Study Design and Data Processing ......................................................................................................... 3 2 Table of 1130 Proteins Measured .......................................................................................................... 4 3 Variable Selection and Statistical Modeling ........................................................................................ -

Chimeric Antigen Receptor (CAR) T Cell Therapy for Metastatic Melanoma: Challenges and Road Ahead
cells Review Chimeric Antigen Receptor (CAR) T Cell Therapy for Metastatic Melanoma: Challenges and Road Ahead Tahereh Soltantoyeh 1,†, Behnia Akbari 1,† , Amirali Karimi 2, Ghanbar Mahmoodi Chalbatani 1 , Navid Ghahri-Saremi 1, Jamshid Hadjati 1, Michael R. Hamblin 3,4 and Hamid Reza Mirzaei 1,* 1 Department of Medical Immunology, School of Medicine, Tehran University of Medical Sciences, Tehran 1417613151, Iran; [email protected] (T.S.); [email protected] (B.A.); [email protected] (G.M.C.); [email protected] (N.G.-S.); [email protected] (J.H.) 2 School of Medicine, Tehran University of Medical Sciences, Tehran 1417613151, Iran; [email protected] 3 Laser Research Centre, Faculty of Health Science, University of Johannesburg, Doornfontein 2028, South Africa; [email protected] 4 Radiation Biology Research Center, Iran University of Medical Sciences, Tehran 1449614535, Iran * Correspondence: [email protected]; Tel.: +98-21-64053268; Fax: +98-21-66419536 † Equally contributed as first author. Abstract: Metastatic melanoma is the most aggressive and difficult to treat type of skin cancer, with a survival rate of less than 10%. Metastatic melanoma has conventionally been considered very difficult to treat; however, recent progress in understanding the cellular and molecular mechanisms involved in the tumorigenesis, metastasis and immune escape have led to the introduction of new therapies. Citation: Soltantoyeh, T.; Akbari, B.; These include targeted molecular therapy and novel immune-based approaches such as immune Karimi, A.; Mahmoodi Chalbatani, G.; checkpoint blockade (ICB), tumor-infiltrating lymphocytes (TILs), and genetically engineered T- Ghahri-Saremi, N.; Hadjati, J.; lymphocytes such as chimeric antigen receptor (CAR) T cells. -

Chemokines and Their Receptors in Rheumatoid Arthritis
ARTHRITIS & RHEUMATISM Vol. 52, No. 3, March 2005, pp 710–721 DOI 10.1002/art.20932 © 2005, American College of Rheumatology REVIEW Chemokines and Their Receptors in Rheumatoid Arthritis Future Targets? Alisa E. Koch Introduction tem was introduced in 2000, in which chemokines are considered as chemokine ligands, and each chemokine Rheumatoid arthritis (RA) is a chronic inflam- has been assigned a designation of CXCL, CCL, XCL, matory disease leading to joint destruction (1). In RA, or CX3CL1 (Figure 1) (10–12). In this report, both the migration of leukocytes into the synovial tissue (ST) former and new nomenclature are noted. occurs. These leukocytes and other cells in the ST, particularly RA ST fibroblasts, produce mediators of CXC chemokines have 2 conserved cysteines inflammation, including chemokines (1). Chemokines, separated by 1 unconserved amino acid (9,13) (Figure currently numbering more than 50, are chemotactic 1). CXC chemokines classically were thought to be cytokines that are important in recruitment of leuko- involved in the chemotaxis of neutrophils. Many chemo- cytes and angiogenesis. They exert chemotactic activity kines may have arisen from reduplication of ancestral toward a variety of cell types (2–7). Some chemokines, genes (13). Hence, CXC chemokines that act on neutro- particularly CXC chemokines containing the ELR motif, phils are clustered on chromosome 4q12–13 (13). How- are angiogenic. The last few years have seen a rapid ever, some genes of more newly discovered CXC che- development of studies aimed at targeting proinflamma- mokines that recruit lymphocytes tend to be located tory chemokines or their receptors in RA and animal away from the major clusters (13). -

CXCL4/Platelet Factor 4 Is an Agonist of CCR1 and Drives Human Monocyte Migration
This is a repository copy of CXCL4/Platelet Factor 4 is an agonist of CCR1 and drives human monocyte migration. White Rose Research Online URL for this paper: https://eprints.whiterose.ac.uk/132464/ Version: Published Version Article: Fox, James Martin orcid.org/0000-0002-2473-7029, Kausar, Fahima, Day, Amy et al. (7 more authors) (2018) CXCL4/Platelet Factor 4 is an agonist of CCR1 and drives human monocyte migration. Scientific Reports. 9466. ISSN 2045-2322 Reuse This article is distributed under the terms of the Creative Commons Attribution (CC BY) licence. This licence allows you to distribute, remix, tweak, and build upon the work, even commercially, as long as you credit the authors for the original work. More information and the full terms of the licence here: https://creativecommons.org/licenses/ Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ www.nature.com/scientificreports OPEN CXCL4/Platelet Factor 4 is an agonist of CCR1 and drives human monocyte migration Received: 10 March 2016 James M. Fox 1,3, Fahima Kausar1, Amy Day1, Michael Osborne1, Khansa Hussain1, Accepted: 5 June 2018 Anja Mueller1,4, Jessica Lin1, Tomoko Tsuchiya 2, Shiro Kanegasaki2 & James E. Pease1 Published: xx xx xxxx Activated platelets release micromolar concentrations of the chemokine CXCL4/Platelet Factor-4. Deposition of CXCL4 onto the vascular endothelium is involved in atherosclerosis, facilitating monocyte arrest and recruitment by an as yet, unidentified receptor. -
Myeloid Innate Immunity Mouse Vapril2018
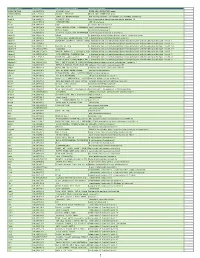
Official Symbol Accession Alias / Previous Symbol Official Full Name 2810417H13Rik NM_026515.2 p15(PAF), Pclaf RIKEN cDNA 2810417H13 gene 2900026A02Rik NM_172884.3 Gm449, LOC231620 RIKEN cDNA 2900026A02 gene Abcc8 NM_011510.3 SUR1, Sur, D930031B21Rik ATP-binding cassette, sub-family C (CFTR/MRP), member 8 Acad10 NM_028037.4 2410021P16Rik acyl-Coenzyme A dehydrogenase family, member 10 Acly NM_134037.2 A730098H14Rik ATP citrate lyase Acod1 NM_008392.1 Irg1 aconitate decarboxylase 1 Acot11 NM_025590.4 Thea, 2010309H15Rik, 1110020M10Rik,acyl-CoA Them1, thioesterase BFIT1 11 Acot3 NM_134246.3 PTE-Ia, Pte2a acyl-CoA thioesterase 3 Acox1 NM_015729.2 Acyl-CoA oxidase, AOX, D130055E20Rikacyl-Coenzyme A oxidase 1, palmitoyl Adam19 NM_009616.4 Mltnb a disintegrin and metallopeptidase domain 19 (meltrin beta) Adam8 NM_007403.2 CD156a, MS2, E430039A18Rik, CD156a disintegrin and metallopeptidase domain 8 Adamts1 NM_009621.4 ADAM-TS1, ADAMTS-1, METH-1, METH1a disintegrin-like and metallopeptidase (reprolysin type) with thrombospondin type 1 motif, 1 Adamts12 NM_175501.2 a disintegrin-like and metallopeptidase (reprolysin type) with thrombospondin type 1 motif, 12 Adamts14 NM_001081127.1 Adamts-14, TS14 a disintegrin-like and metallopeptidase (reprolysin type) with thrombospondin type 1 motif, 14 Adamts17 NM_001033877.4 AU023434 a disintegrin-like and metallopeptidase (reprolysin type) with thrombospondin type 1 motif, 17 Adamts2 NM_001277305.1 hPCPNI, ADAM-TS2, a disintegrin and ametalloproteinase disintegrin-like and with metallopeptidase thrombospondin -

Nouvelle Cuisine: Platelets Served with Inflammation
Th eJournal of Brief Reviews Immunology Nouvelle Cuisine: Platelets Served with Inflammation x { ‖ Rick Kapur,*,† Anne Zufferey,* Eric Boilard,‡ and John W. Semple*,†, , , Platelets are small cellular fragments with the pri- granules, endosomes, lysosomes, and mitochondria. The a mary physiological role of maintaining hemostasis. In and dense granules contain different cargos that are respon- addition to this well-described classical function, it is sible for the platelet’s ability to aggregate and activate the becoming increasingly clear that platelets have an in- coagulation cascade at the site of vessel injury. Platelets also timate connection with infection and inflammation. have a series of invaginated folded membranes that form the This stems from several platelet characteristics, includ- inner canalicular system, and this allows the platelet to sig- ing their ability to bind infectious agents and secrete nificantly increase surface area upon activation. What has many immunomodulatory cytokines and chemokines, become clear over the last 50 years is that, in addition to their as well as their expression of receptors for various im- primary role in hemostasis, platelets are multifunctional and mune effector and regulatory functions, such as TLRs, are key players in many other physiological and pathological which allow them to sense pathogen-associated molec- processes (e.g., wound repair, inflammatory processes, and the immune response) (2–8). ular patterns. Furthermore, platelets contain RNA that Interestingly, in many invertebrate life forms, a single cell type can be nascently translated under different environ- is responsible for multiple innate defense functions, including mental stresses, and they are able to release membrane hemostasis (9, 10). -

Human CXCL4/PF4 Immunoassay Quantikine
Quantikine® ELISA Human CXCL4/PF4 Immunoassay Catalog Number DPF40 For the quantitative determination of human Platelet Factor 4 (PF4) concentrations in cell culture supernates, serum, and platelet-poor plasma. This package insert must be read in its entirety before using this product. For research use only. Not for use in diagnostic procedures. TABLE OF CONTENTS SECTION PAGE INTRODUCTION ....................................................................................................................................................................1 PRINCIPLE OF THE ASSAY ..................................................................................................................................................2 LIMITATIONS OF THE PROCEDURE ................................................................................................................................2 TECHNICAL HINTS ................................................................................................................................................................2 MATERIALS PROVIDED & STORAGE CONDITIONS ..................................................................................................3 OTHER SUPPLIES REQUIRED ............................................................................................................................................3 PRECAUTIONS ........................................................................................................................................................................4 SAMPLE -

Rapid Internalization and Nuclear Translocation of CCL5 and CXCL4 in Endothelial Cells
International Journal of Molecular Sciences Article Rapid Internalization and Nuclear Translocation of CCL5 and CXCL4 in Endothelial Cells Annemiek Dickhout 1 , Dawid M. Kaczor 1 , Alexandra C. A. Heinzmann 1, Sanne L. N. Brouns 1, Johan W. M. Heemskerk 1, Marc A. M. J. van Zandvoort 2,3 and Rory R. Koenen 1,4,* 1 Department of Biochemistry, Cardiovascular Research Institute Maastricht, Maastricht University, 6229 ER Maastricht, The Netherlands; [email protected] (A.D.); [email protected] (D.M.K.); [email protected] (A.C.A.H.); [email protected] (S.L.N.B.); [email protected] (J.W.M.H.) 2 Department of Genetics and Cell Biology, Molecular Cell Biology, School for Oncology and Developmental Biology, Maastricht University, 6229 ER Maastricht, The Netherlands; [email protected] 3 Institute for Molecular Cardiovascular Research IMCAR, RWTH Aachen University, 52074 Aachen, Germany 4 Institute for Cardiovascular Prevention (IPEK), LMU Munich, 80336 Munich, Germany * Correspondence: [email protected] Abstract: The chemokines CCL5 and CXCL4 are deposited by platelets onto endothelial cells, induc- ing monocyte arrest. Here, the fate of CCL5 and CXCL4 after endothelial deposition was investigated. Human umbilical vein endothelial cells (HUVECs) and EA.hy926 cells were incubated with CCL5 or CXCL4 for up to 120 min, and chemokine uptake was analyzed by microscopy and by ELISA. Intracellular calcium signaling was visualized upon chemokine treatment, and monocyte arrest Citation: Dickhout, A.; Kaczor, D.M.; was evaluated under laminar flow. Whereas CXCL4 remained partly on the cell surface, all of the Heinzmann, A.C.A.; Brouns, S.L.N.; CCL5 was internalized into endothelial cells. -

Role of Platelet Cytoskeleton in Platelet Biomechanics
Review Article 337 Role of Platelet Cytoskeleton in Platelet Biomechanics: Current and Emerging Methodologies and Their Potential Relevance for the Investigation of Inherited Platelet Disorders Carlo Zaninetti1,2,3 Laura Sachs1 Raghavendra Palankar1 1 Department of Transfusion Medicine, Institute of Immunology and Address for correspondence Raghavendra Palankar, PhD, Transfusion Medicine, University Medicine Greifswald, Greifswald, Department of Transfusion Medicine, Institute of Immunology and Germany Transfusion Medicine Greifswald, University Medicine, Greifswald, 2 Department of Internal Medicine, University of Pavia and IRCCS 17489 Greifswald, Germany Policlinico San Matteo Foundation, Pavia, Italy (e-mail: [email protected]). 3 PhD Course of Experimental Medicine, University of Pavia, Pavia, Italy Hämostaseologie 2020;40:337–347. Abstract Cytoskeleton is composed of more than 100 proteins and represents a dynamic network of the cellular cytoplasm. Cytoskeletal functions include spatial organization of cellular components, structural connection of the cell with external environment, and biomechanical force generation. Cytoskeleton takes part, at different levels, in all phases of platelet biogenesis: megakaryocyte (MK) differentiation, MK maturation, and platelet formation. In addition, it also plays a major role in each stage of platelet function. Inherited platelet disorders (IPDs) are a group of rare diseases featured by low platelet count and/or impaired platelet function. Over the past decade, the investiga- tion of platelet biomechanics has become a major and highly relevant theme of research due to its implications at every stage of development of human life. The initial use of diverse biophysical techniques (e.g., micropipette aspiration, atomic force and scanning ion conductance microscopy, real-time deformability cytometry) started unraveling biomechanical features of platelets that are expected to provide new explanations for physiological and pathological mechanisms.