Targeting a Key Role of Platelet-Neutrophil Interaction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model
Downloaded from http://www.jimmunol.org/ by guest on September 25, 2021 T + is online at: average * The Journal of Immunology , 34 of which you can access for free at: 2016; 197:1477-1488; Prepublished online 1 July from submission to initial decision 4 weeks from acceptance to publication 2016; doi: 10.4049/jimmunol.1600589 http://www.jimmunol.org/content/197/4/1477 Molecular Profile of Tumor-Specific CD8 Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. Waugh, Sonia M. Leach, Brandon L. Moore, Tullia C. Bruno, Jonathan D. Buhrman and Jill E. Slansky J Immunol cites 95 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2016/07/01/jimmunol.160058 9.DCSupplemental This article http://www.jimmunol.org/content/197/4/1477.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 25, 2021. The Journal of Immunology Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. -

Characterization of FLT3-Itdmut Acute Myeloid Leukemia
Travaglini et al. Blood Cancer Journal (2020) 10:85 https://doi.org/10.1038/s41408-020-00352-9 Blood Cancer Journal ARTICLE Open Access Characterization of FLT3-ITDmut acute myeloid leukemia: molecular profiling of leukemic precursor cells Serena Travaglini1, Daniela Francesca Angelini 2, Valentina Alfonso1, Gisella Guerrera2,SerenaLavorgna1, Mariadomenica Divona1, Anna Maria Nardozza1, Maria Irno Consalvo1, Emiliano Fabiani1,MarcoDeBardi 2, Benedetta Neri3,FabioForghieri4, Francesco Marchesi5, Giovangiacinto Paterno1, Raffaella Cerretti1, Eva Barragan 6, Valentina Fiori7,SabrinaDominici7, Maria Ilaria Del Principe1, Adriano Venditti 1, Luca Battistini2, William Arcese1, Francesco Lo-Coco1, Maria Teresa Voso 1,2 and Tiziana Ottone1,2 Abstract Acute myeloid leukemia (AML) with FLT3-ITD mutations (FLT3-ITDmut) remains a therapeutic challenge, with a still high relapse rate, despite targeted treatment with tyrosine kinase inhibitors. In this disease, the CD34/CD123/CD25/CD99+ leukemic precursor cells (LPCs) phenotype predicts for FLT3-ITD-positivity. The aim of this study was to characterize the distribution of FLT3-ITD mutation in different progenitor cell subsets to shed light on the subclonal architecture of FLT3-ITDmut AML. Using high-speed cell sorting, we sequentially purified LPCs and CD34+ progenitors in samples from patients with FLT3-ITDmut AML (n = 12). A higher FLT3-ITDmut load was observed within CD34/CD123/CD25/CD99+ LPCs, as compared to CD34+ progenitors (CD123+/−,CD25−,CD99low/−)(p = 0.0005) and mononuclear cells (MNCs) (p < 0.0001). This was associated with significantly increased CD99 mean fluorescence intensity in LPCs. 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; Significantly higher FLT3-ITDmut burden was also observed in LPCs of AML patients with a small FLT3-ITDmut clones at diagnosis. -

Propranolol-Mediated Attenuation of MMP-9 Excretion in Infants with Hemangiomas
Supplementary Online Content Thaivalappil S, Bauman N, Saieg A, Movius E, Brown KJ, Preciado D. Propranolol-mediated attenuation of MMP-9 excretion in infants with hemangiomas. JAMA Otolaryngol Head Neck Surg. doi:10.1001/jamaoto.2013.4773 eTable. List of All of the Proteins Identified by Proteomics This supplementary material has been provided by the authors to give readers additional information about their work. © 2013 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 10/01/2021 eTable. List of All of the Proteins Identified by Proteomics Protein Name Prop 12 mo/4 Pred 12 mo/4 Δ Prop to Pred mo mo Myeloperoxidase OS=Homo sapiens GN=MPO 26.00 143.00 ‐117.00 Lactotransferrin OS=Homo sapiens GN=LTF 114.00 205.50 ‐91.50 Matrix metalloproteinase‐9 OS=Homo sapiens GN=MMP9 5.00 36.00 ‐31.00 Neutrophil elastase OS=Homo sapiens GN=ELANE 24.00 48.00 ‐24.00 Bleomycin hydrolase OS=Homo sapiens GN=BLMH 3.00 25.00 ‐22.00 CAP7_HUMAN Azurocidin OS=Homo sapiens GN=AZU1 PE=1 SV=3 4.00 26.00 ‐22.00 S10A8_HUMAN Protein S100‐A8 OS=Homo sapiens GN=S100A8 PE=1 14.67 30.50 ‐15.83 SV=1 IL1F9_HUMAN Interleukin‐1 family member 9 OS=Homo sapiens 1.00 15.00 ‐14.00 GN=IL1F9 PE=1 SV=1 MUC5B_HUMAN Mucin‐5B OS=Homo sapiens GN=MUC5B PE=1 SV=3 2.00 14.00 ‐12.00 MUC4_HUMAN Mucin‐4 OS=Homo sapiens GN=MUC4 PE=1 SV=3 1.00 12.00 ‐11.00 HRG_HUMAN Histidine‐rich glycoprotein OS=Homo sapiens GN=HRG 1.00 12.00 ‐11.00 PE=1 SV=1 TKT_HUMAN Transketolase OS=Homo sapiens GN=TKT PE=1 SV=3 17.00 28.00 ‐11.00 CATG_HUMAN Cathepsin G OS=Homo -

Downloaded in Aug 2019
ARTICLE https://doi.org/10.1038/s41467-021-24473-2 OPEN IL-15 and PIM kinases direct the metabolic programming of intestinal intraepithelial lymphocytes Olivia J. James1, Maud Vandereyken1, Julia M. Marchingo 2, Francois Singh1, Susan E. Bray3, Jamie Wilson4, ✉ Andrew G. Love1 & Mahima Swamy 1 1234567890():,; Intestinal intraepithelial lymphocytes (IEL) are an abundant population of tissue-resident T cells that protect and maintain the intestinal barrier. IEL respond to epithelial cell-derived IL-15, which is complexed to the IL-15 receptor α chain (IL-15/Rα). IL-15 is essential both for maintaining IEL homeostasis and inducing IEL responses to epithelial stress, which has been associated with Coeliac disease. Here, we apply quantitative mass spectrometry to IL-15/Rα- stimulated IEL to investigate how IL-15 directly regulates inflammatory functions of IEL. IL-15/ Rα drives IEL activation through cell cycle regulation, upregulation of metabolic machinery and expression of a select repertoire of cell surface receptors. IL-15/Rα selectively upregu- lates the Ser/Thr kinases PIM1 and PIM2, which are essential for IEL to proliferate, grow and upregulate granzyme B in response to inflammatory IL-15. Notably, IEL from patients with Coeliac disease have high PIM expression. Together, these data indicate PIM kinases as important effectors of IEL responses to inflammatory IL-15. 1 MRC Protein Phosphorylation and Ubiquitylation Unit, University of Dundee, Dundee, UK. 2 Division of Cell Signalling and Immunology, School of Life Sciences, University of Dundee, Dundee, UK. 3 NHS Research Scotland, Tayside Tissue Biorepository, University of Dundee, Dundee, UK. 4 Department of ✉ Pathology, NHS Tayside, Ninewells Hospital, Dundee, UK. -

Single-Cell RNA Sequencing Demonstrates the Molecular and Cellular Reprogramming of Metastatic Lung Adenocarcinoma
ARTICLE https://doi.org/10.1038/s41467-020-16164-1 OPEN Single-cell RNA sequencing demonstrates the molecular and cellular reprogramming of metastatic lung adenocarcinoma Nayoung Kim 1,2,3,13, Hong Kwan Kim4,13, Kyungjong Lee 5,13, Yourae Hong 1,6, Jong Ho Cho4, Jung Won Choi7, Jung-Il Lee7, Yeon-Lim Suh8,BoMiKu9, Hye Hyeon Eum 1,2,3, Soyean Choi 1, Yoon-La Choi6,10,11, Je-Gun Joung1, Woong-Yang Park 1,2,6, Hyun Ae Jung12, Jong-Mu Sun12, Se-Hoon Lee12, ✉ ✉ Jin Seok Ahn12, Keunchil Park12, Myung-Ju Ahn 12 & Hae-Ock Lee 1,2,3,6 1234567890():,; Advanced metastatic cancer poses utmost clinical challenges and may present molecular and cellular features distinct from an early-stage cancer. Herein, we present single-cell tran- scriptome profiling of metastatic lung adenocarcinoma, the most prevalent histological lung cancer type diagnosed at stage IV in over 40% of all cases. From 208,506 cells populating the normal tissues or early to metastatic stage cancer in 44 patients, we identify a cancer cell subtype deviating from the normal differentiation trajectory and dominating the metastatic stage. In all stages, the stromal and immune cell dynamics reveal ontological and functional changes that create a pro-tumoral and immunosuppressive microenvironment. Normal resident myeloid cell populations are gradually replaced with monocyte-derived macrophages and dendritic cells, along with T-cell exhaustion. This extensive single-cell analysis enhances our understanding of molecular and cellular dynamics in metastatic lung cancer and reveals potential diagnostic and therapeutic targets in cancer-microenvironment interactions. 1 Samsung Genome Institute, Samsung Medical Center, Seoul 06351, Korea. -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

CD29 Identifies IFN-Γ–Producing Human CD8+ T Cells With
+ CD29 identifies IFN-γ–producing human CD8 T cells with an increased cytotoxic potential Benoît P. Nicoleta,b, Aurélie Guislaina,b, Floris P. J. van Alphenc, Raquel Gomez-Eerlandd, Ton N. M. Schumacherd, Maartje van den Biggelaarc,e, and Monika C. Wolkersa,b,1 aDepartment of Hematopoiesis, Sanquin Research, 1066 CX Amsterdam, The Netherlands; bLandsteiner Laboratory, Oncode Institute, Amsterdam University Medical Center, University of Amsterdam, 1105 AZ Amsterdam, The Netherlands; cDepartment of Research Facilities, Sanquin Research, 1066 CX Amsterdam, The Netherlands; dDivision of Molecular Oncology and Immunology, Oncode Institute, The Netherlands Cancer Institute, 1066 CX Amsterdam, The Netherlands; and eDepartment of Molecular and Cellular Haemostasis, Sanquin Research, 1066 CX Amsterdam, The Netherlands Edited by Anjana Rao, La Jolla Institute for Allergy and Immunology, La Jolla, CA, and approved February 12, 2020 (received for review August 12, 2019) Cytotoxic CD8+ T cells can effectively kill target cells by producing therefore developed a protocol that allowed for efficient iso- cytokines, chemokines, and granzymes. Expression of these effector lation of RNA and protein from fluorescence-activated cell molecules is however highly divergent, and tools that identify and sorting (FACS)-sorted fixed T cells after intracellular cytokine + preselect CD8 T cells with a cytotoxic expression profile are lacking. staining. With this top-down approach, we performed an un- + Human CD8 T cells can be divided into IFN-γ– and IL-2–producing biased RNA-sequencing (RNA-seq) and mass spectrometry cells. Unbiased transcriptomics and proteomics analysis on cytokine- γ– – + + (MS) analyses on IFN- and IL-2 producing primary human producing fixed CD8 T cells revealed that IL-2 cells produce helper + + + CD8 Tcells. -

Mechanisms of Immunothrombosis in Vaccine-Induced Thrombotic Thrombocytopenia (VITT) Compared to Natural SARS-Cov-2 Infection
Journal of Autoimmunity 121 (2021) 102662 Contents lists available at ScienceDirect Journal of Autoimmunity journal homepage: www.elsevier.com/locate/jautimm Mechanisms of Immunothrombosis in Vaccine-Induced Thrombotic Thrombocytopenia (VITT) Compared to Natural SARS-CoV-2 Infection Dennis McGonagle a,b, Gabriele De Marco a, Charles Bridgewood a,* a Leeds Institute of Rheumatic and Musculoskeletal Medicine (LIRMM), University of Leeds, Leeds, UK b National Institute for Health Research (NIHR) Leeds Biomedical Research Centre (BRC), Leeds Teaching Hospitals, Leeds, UK ARTICLE INFO ABSTRACT Keywords: Herein, we consider venous immunothrombotic mechanisms in SARS-CoV-2 infection and anti-SARS-CoV-2 DNA COVID-19 pneumonia related thrombosis vaccination. Primary SARS-CoV-2 infection with systemic viral RNA release (RNAaemia) contributes to innate Vaccine induced thrombotic thrombocytopenia immune coagulation cascade activation, with both pulmonary and systemic immunothrombosis - including (VITT) venous territory strokes. However, anti-SARS-CoV-2 adenoviral-vectored-DNA vaccines -initially shown for the Heparin induced thrombocytopenia (HIT) ChAdOx1 vaccine-may rarely exhibit autoimmunity with autoantibodies to Platelet Factor-4 (PF4) that is termed DNA-PF4 interactions. VITT model Vaccine-Induced Thrombotic Thrombocytopenia (VITT), an entity pathophysiologically similar to Heparin- Induced Thrombocytopenia (HIT). The PF4 autoantigen is a polyanion molecule capable of independent in teractions with negatively charged bacterial cellular wall, heparin and DNA molecules, thus linking intravascular innate immunity to both bacterial cell walls and pathogen-derived DNA. Crucially, negatively charged extra cellular DNA is a powerful adjuvant that can break tolerance to positively charged nuclear histone proteins in many experimental autoimmunity settings, including SLE and scleroderma. Analogous to DNA-histone inter actons, positively charged PF4-DNA complexes stimulate strong interferon responses via Toll-Like Receptor (TLR) 9 engagement. -

Blood Flow Guides Sequential Support of Neutrophil Arrest and Diapedesis
RESEARCH ARTICLE Blood flow guides sequential support of neutrophil arrest and diapedesis by PILR-b 1 and PILR-a Yu-Tung Li, Debashree Goswami†, Melissa Follmer, Annette Artz, Mariana Pacheco-Blanco, Dietmar Vestweber* Vascular Cell Biology, Max Planck Institute of Molecular Biomedicine, Mu¨ nster, Germany Abstract Arrest of rapidly flowing neutrophils in venules relies on capturing through selectins and chemokine-induced integrin activation. Despite a long-established concept, we show here that gene inactivation of activating paired immunoglobulin-like receptor (PILR)-b1 nearly halved the efficiency of neutrophil arrest in venules of the mouse cremaster muscle. We found that this receptor binds to CD99, an interaction which relies on flow-induced shear forces and boosts chemokine-induced b2-integrin-activation, leading to neutrophil attachment to endothelium. Upon arrest, binding of PILR-b1 to CD99 ceases, shifting the signaling balance towards inhibitory PILR-a. This enables integrin deactivation and supports cell migration. Thus, flow-driven shear forces guide sequential signaling of first activating PILR-b1 followed by inhibitory PILR-a to prompt neutrophil arrest and then transmigration. This doubles the efficiency of selectin-chemokine driven neutrophil arrest by PILR-b1 and then supports transition to migration by PILR-a. DOI: https://doi.org/10.7554/eLife.47642.001 *For correspondence: [email protected] Present address: †Center for Global Infectious Disease Introduction Research, Seattle Childrens Host defense against pathogens depends on the recruitment of leukocytes to sites of infections Research Institute, Seattle, (Ley et al., 2007). Selectins capture leukocytes to the endothelial cell surface by binding to glyco- United States conjugates (McEver, 2015). -
IHC Test Menu
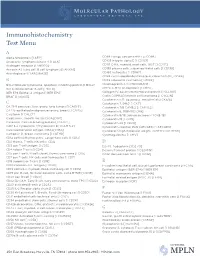
Immunohistochemistry Test Menu A Alpha fetoprotein [I AFP] CD99 Ewings sarcoma PNET [I CD99] Anaplastic lymphoma kinase -1 [I ALK] CD103 Integrin alpha E [I CD103] Androgen receptor [I ANDRO]* CD117 C-Kit, myeloid, mast cells, GIST [I CD117] Annexin A1, hairy cell, B cell lymphoma [I ANXA1] CD138 plasma cells, subset epithelial cells [I CD138] Anti-Arginase-1 [I ARGINASE] CD163 histiocytes [I CD163] CDK4 cyclin-depdendent kinase-4, clone DCS-31 [I CDK4] B CDX2 colorectal carcinoma [I CDX2] BCL2 follicular lymphoma, apoptosis inhibiting protein [I BCL2] Chromogranin A [I CHROGRAN] BCL6 follicle center B-cell [I BCL6] CMYC C-MYC oncoprotein [I CMYC] BER EP4 Epithelial antigen [I BER EP4] Collagen IV, basement membrane protein [I CLLGIV] BRAF [I V600E] Cyclin D1/PRAD1 mantle cell lymphoma [I CYCLIN] Cytokeratin 5/6, squamous, mesothelial [I CK5/6] C Cytokeratin 7, 54kD [I CK7] CA 19-9 pancreas, liver, ovary, lung tumors [I CA19 9] Cytokeratin 7/8 CAM5.2 [I CAM 5.2] CA 125 epitheliod malignancies ovary, breast [I CA125] Cytokeratin 8, 35BH11 [I CK8] Calcitonin [I CALCT] Cytokeratin 8/18, adenocarcinoma [I CK8/18] Caldesmon, smooth muscle [I CALDSM] Cytokeratin 19 [I CK19] Calretinin; Calcium binding protein [I CALRT] Cytokeratin 20 [I CK20] CAM 5.2 Cytokeratin 7/Cytokeratin 8 [I CAM 5.2] Cytokeratin cocktail, PAN (AE1/AE3) [I AE1/AE3] Carcinoembryonic antigen (CEA) [I CEA] Cytokeratin high molecular weight; 34BE12 [I CK HMW] Cathepsin D, breast carcinoma [I CATHD] Cytomegalovirus [I CMV] CD1a cortical thymocyctes, Langerhans cells [I CD1a] -

Critical Role of CXCL4 in the Lung Pathogenesis of Influenza (H1N1) Respiratory Infection
ARTICLES Critical role of CXCL4 in the lung pathogenesis of influenza (H1N1) respiratory infection L Guo1,3, K Feng1,3, YC Wang1,3, JJ Mei1,2, RT Ning1, HW Zheng1, JJ Wang1, GS Worthen2, X Wang1, J Song1,QHLi1 and LD Liu1 Annual epidemics and unexpected pandemics of influenza are threats to human health. Lung immune and inflammatory responses, such as those induced by respiratory infection influenza virus, determine the outcome of pulmonary pathogenesis. Platelet-derived chemokine (C-X-C motif) ligand 4 (CXCL4) has an immunoregulatory role in inflammatory diseases. Here we show that CXCL4 is associated with pulmonary influenza infection and has a critical role in protecting mice from fatal H1N1 virus respiratory infection. CXCL4 knockout resulted in diminished viral clearance from the lung and decreased lung inflammation during early infection but more severe lung pathology relative to wild-type mice during late infection. Additionally, CXCL4 deficiency decreased leukocyte accumulation in the infected lung with markedly decreased neutrophil infiltration into the lung during early infection and extensive leukocyte, especially lymphocyte accumulation at the late infection stage. Loss of CXCL4 did not affect the activation of adaptive immune T and B lymphocytes during the late stage of lung infection. Further study revealed that CXCL4 deficiency inhibited neutrophil recruitment to the infected mouse lung. Thus the above results identify CXCL4 as a vital immunoregulatory chemokine essential for protecting mice against influenza A virus infection, especially as it affects the development of lung injury and neutrophil mobilization to the inflamed lung. INTRODUCTION necrosis factor (TNF)-a, interleukin (IL)-6, and IL-1b, to exert Influenza A virus (IAV) infections cause respiratory diseases in further antiviral innate immune effects.2 Meanwhile, the innate large populations worldwide every year and result in seasonal immune cells act as antigen-presenting cells and release influenza epidemics and unexpected pandemic.