Platelet Factor 4 Binds to Interleukin 8 Receptors and Activates Neutrophils When Its N Terminus Is Modified with Glu-Leu-Arg
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanisms of Immunothrombosis in Vaccine-Induced Thrombotic Thrombocytopenia (VITT) Compared to Natural SARS-Cov-2 Infection
Journal of Autoimmunity 121 (2021) 102662 Contents lists available at ScienceDirect Journal of Autoimmunity journal homepage: www.elsevier.com/locate/jautimm Mechanisms of Immunothrombosis in Vaccine-Induced Thrombotic Thrombocytopenia (VITT) Compared to Natural SARS-CoV-2 Infection Dennis McGonagle a,b, Gabriele De Marco a, Charles Bridgewood a,* a Leeds Institute of Rheumatic and Musculoskeletal Medicine (LIRMM), University of Leeds, Leeds, UK b National Institute for Health Research (NIHR) Leeds Biomedical Research Centre (BRC), Leeds Teaching Hospitals, Leeds, UK ARTICLE INFO ABSTRACT Keywords: Herein, we consider venous immunothrombotic mechanisms in SARS-CoV-2 infection and anti-SARS-CoV-2 DNA COVID-19 pneumonia related thrombosis vaccination. Primary SARS-CoV-2 infection with systemic viral RNA release (RNAaemia) contributes to innate Vaccine induced thrombotic thrombocytopenia immune coagulation cascade activation, with both pulmonary and systemic immunothrombosis - including (VITT) venous territory strokes. However, anti-SARS-CoV-2 adenoviral-vectored-DNA vaccines -initially shown for the Heparin induced thrombocytopenia (HIT) ChAdOx1 vaccine-may rarely exhibit autoimmunity with autoantibodies to Platelet Factor-4 (PF4) that is termed DNA-PF4 interactions. VITT model Vaccine-Induced Thrombotic Thrombocytopenia (VITT), an entity pathophysiologically similar to Heparin- Induced Thrombocytopenia (HIT). The PF4 autoantigen is a polyanion molecule capable of independent in teractions with negatively charged bacterial cellular wall, heparin and DNA molecules, thus linking intravascular innate immunity to both bacterial cell walls and pathogen-derived DNA. Crucially, negatively charged extra cellular DNA is a powerful adjuvant that can break tolerance to positively charged nuclear histone proteins in many experimental autoimmunity settings, including SLE and scleroderma. Analogous to DNA-histone inter actons, positively charged PF4-DNA complexes stimulate strong interferon responses via Toll-Like Receptor (TLR) 9 engagement. -

Expression of Inflammation-Related Genes Is Altered in Gastric Tissue of Patients with Advanced Stages of NAFLD
Hindawi Publishing Corporation Mediators of Inflammation Volume 2013, Article ID 684237, 10 pages http://dx.doi.org/10.1155/2013/684237 Clinical Study Expression of Inflammation-Related Genes Is Altered in Gastric Tissue of Patients with Advanced Stages of NAFLD Rohini Mehta,1,2 Aybike Birerdinc,1,2 Arpan Neupane,1,2 Amirhossein Shamsaddini,1,2 Arian Afendy,1,3 Hazem Elariny,1,3 Vikas Chandhoke,2 Ancha Baranova,1,2 and Zobair M. Younossi1,3 1 Betty and Guy Beatty Obesity and Liver Program, Inova Health System, Falls Church, VA 22042, USA 2 Center for the Study of Chronic Metabolic Diseases, School of Systems Biology, College of Science, George Mason University, Fairfax, VA 22030, USA 3 Center for Liver Diseases and Department of Medicine, Inova Fairfax Hospital, Falls Church, VA 22042, USA Correspondence should be addressed to Zobair M. Younossi; [email protected] Received 15 December 2012; Revised 12 February 2013; Accepted 14 February 2013 Academic Editor: David Bernardo Ordiz Copyright © 2013 Rohini Mehta et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Obesity is associated with chronic low-grade inflammation perpetuated by visceral adipose. Other organs, particularly stomach and intestine, may also overproduce proinflammatory molecules. We examined the gene expression patterns in gastric tissue of morbidly obese patients with nonalcoholic fatty liver disease (NAFLD) and compared the changes in gene expression in different histological forms of NAFLD. Stomach tissue samples from 20 morbidly obese NAFLD patients who were undergoing sleeve gastrectomy were profiled using qPCR for 84 genes encoding inflammatory cytokines, chemokines, their receptors, and other components of inflammatory cascades. -

Critical Role of CXCL4 in the Lung Pathogenesis of Influenza (H1N1) Respiratory Infection
ARTICLES Critical role of CXCL4 in the lung pathogenesis of influenza (H1N1) respiratory infection L Guo1,3, K Feng1,3, YC Wang1,3, JJ Mei1,2, RT Ning1, HW Zheng1, JJ Wang1, GS Worthen2, X Wang1, J Song1,QHLi1 and LD Liu1 Annual epidemics and unexpected pandemics of influenza are threats to human health. Lung immune and inflammatory responses, such as those induced by respiratory infection influenza virus, determine the outcome of pulmonary pathogenesis. Platelet-derived chemokine (C-X-C motif) ligand 4 (CXCL4) has an immunoregulatory role in inflammatory diseases. Here we show that CXCL4 is associated with pulmonary influenza infection and has a critical role in protecting mice from fatal H1N1 virus respiratory infection. CXCL4 knockout resulted in diminished viral clearance from the lung and decreased lung inflammation during early infection but more severe lung pathology relative to wild-type mice during late infection. Additionally, CXCL4 deficiency decreased leukocyte accumulation in the infected lung with markedly decreased neutrophil infiltration into the lung during early infection and extensive leukocyte, especially lymphocyte accumulation at the late infection stage. Loss of CXCL4 did not affect the activation of adaptive immune T and B lymphocytes during the late stage of lung infection. Further study revealed that CXCL4 deficiency inhibited neutrophil recruitment to the infected mouse lung. Thus the above results identify CXCL4 as a vital immunoregulatory chemokine essential for protecting mice against influenza A virus infection, especially as it affects the development of lung injury and neutrophil mobilization to the inflamed lung. INTRODUCTION necrosis factor (TNF)-a, interleukin (IL)-6, and IL-1b, to exert Influenza A virus (IAV) infections cause respiratory diseases in further antiviral innate immune effects.2 Meanwhile, the innate large populations worldwide every year and result in seasonal immune cells act as antigen-presenting cells and release influenza epidemics and unexpected pandemic. -

Lung Neutrophilic Recruitment and IL-8/IL-17A Tissue Expression in COVID-19
PERSPECTIVE published: 30 March 2021 doi: 10.3389/fimmu.2021.656350 Lung Neutrophilic Recruitment and IL-8/IL-17A Tissue Expression in COVID-19 Marina Luise Viola Azevedo 1, Aline Cristina Zanchettin 2, Caroline Busatta Vaz de Paula 1, Jarbas da Silva Motta Ju´ nior 3, Mineia Alessandra Scaranello Malaquias 1, Sonia Mara Raboni 4,Pl´ınio Cezar Neto 1, Rafaela Chiuco Zeni 1, Amanda Prokopenko 1, N´ıcolas Henrique Borges 1, Thiago Mateus Godoy 1, Ana Paula Kubaski Benevides 1, Edited by: Daiane Gavlik de Souza 4, Cristina Pellegrino Baena 3, Cleber Machado-Souza 2* Remi Cheynier, and Lucia de Noronha 1* INSERM U1016 Institut Cochin, France 1 Laboratory of Experimental Pathology, Postgraduate Program of Health Sciences, School of Medicine, Pontifícia 2 Reviewed by: Universidade Católica do Paraná, Curitiba, Brazil, Postgraduate Program in Biotechnology Applied to Child and Adolescent Health, Faculdades Pequeno Príncipe, Instituto de Pesquisa Pele´ Pequeno Pr´ıncipe, Curitiba, Brazil, 3 Hospital Marcelino Dominique Schols, Champagnat, Postgraduate Program of Health Sciences, School of Medicine, Pontifícia Universidade Católica do Paraná, KU Leuven, Belgium Curitiba, Brazil, 4 Virology Laboratory, Universidade Federal do Paraná, Hospital de Cl´ınicas, Curitiba, Brazil Harm Maarsingh, Palm Beach Atlantic University, United States The new SARS-CoV-2 virus differs from the pandemic Influenza A virus H1N1 subtype *Correspondence: (H1N1pmd09) how it induces a pro-inflammatory response in infected patients. This study Lucia de Noronha [email protected] aims to evaluate the involvement of SNPs and tissue expression of IL-17A and the Cleber Machado-Souza neutrophils recruitment in post-mortem lung samples from patients who died of severe [email protected] forms of COVID-19 comparing to those who died by H1N1pdm09. -

Evolutionary Divergence and Functions of the Human Interleukin (IL) Gene Family Chad Brocker,1 David Thompson,2 Akiko Matsumoto,1 Daniel W
UPDATE ON GENE COMPLETIONS AND ANNOTATIONS Evolutionary divergence and functions of the human interleukin (IL) gene family Chad Brocker,1 David Thompson,2 Akiko Matsumoto,1 Daniel W. Nebert3* and Vasilis Vasiliou1 1Molecular Toxicology and Environmental Health Sciences Program, Department of Pharmaceutical Sciences, University of Colorado Denver, Aurora, CO 80045, USA 2Department of Clinical Pharmacy, University of Colorado Denver, Aurora, CO 80045, USA 3Department of Environmental Health and Center for Environmental Genetics (CEG), University of Cincinnati Medical Center, Cincinnati, OH 45267–0056, USA *Correspondence to: Tel: þ1 513 821 4664; Fax: þ1 513 558 0925; E-mail: [email protected]; [email protected] Date received (in revised form): 22nd September 2010 Abstract Cytokines play a very important role in nearly all aspects of inflammation and immunity. The term ‘interleukin’ (IL) has been used to describe a group of cytokines with complex immunomodulatory functions — including cell proliferation, maturation, migration and adhesion. These cytokines also play an important role in immune cell differentiation and activation. Determining the exact function of a particular cytokine is complicated by the influence of the producing cell type, the responding cell type and the phase of the immune response. ILs can also have pro- and anti-inflammatory effects, further complicating their characterisation. These molecules are under constant pressure to evolve due to continual competition between the host’s immune system and infecting organisms; as such, ILs have undergone significant evolution. This has resulted in little amino acid conservation between orthologous proteins, which further complicates the gene family organisation. Within the literature there are a number of overlapping nomenclature and classification systems derived from biological function, receptor-binding properties and originating cell type. -

Inflammatory Modulation of Hematopoietic Stem Cells by Magnetic Resonance Imaging
Electronic Supplementary Material (ESI) for RSC Advances. This journal is © The Royal Society of Chemistry 2014 Inflammatory modulation of hematopoietic stem cells by Magnetic Resonance Imaging (MRI)-detectable nanoparticles Sezin Aday1,2*, Jose Paiva1,2*, Susana Sousa2, Renata S.M. Gomes3, Susana Pedreiro4, Po-Wah So5, Carolyn Ann Carr6, Lowri Cochlin7, Ana Catarina Gomes2, Artur Paiva4, Lino Ferreira1,2 1CNC-Center for Neurosciences and Cell Biology, University of Coimbra, Coimbra, Portugal, 2Biocant, Biotechnology Innovation Center, Cantanhede, Portugal, 3King’s BHF Centre of Excellence, Cardiovascular Proteomics, King’s College London, London, UK, 4Centro de Histocompatibilidade do Centro, Coimbra, Portugal, 5Department of Neuroimaging, Institute of Psychiatry, King's College London, London, UK, 6Cardiac Metabolism Research Group, Department of Physiology, Anatomy & Genetics, University of Oxford, UK, 7PulseTeq Limited, Chobham, Surrey, UK. *These authors contributed equally to this work. #Correspondence to Lino Ferreira ([email protected]). Experimental Section Preparation and characterization of NP210-PFCE. PLGA (Resomers 502 H; 50:50 lactic acid: glycolic acid) (Boehringer Ingelheim) was covalently conjugated to fluoresceinamine (Sigma- Aldrich) according to a protocol reported elsewhere1. NPs were prepared by dissolving PLGA (100 mg) in a solution of propylene carbonate (5 mL, Sigma). PLGA solution was mixed with perfluoro- 15-crown-5-ether (PFCE) (178 mg) (Fluorochem, UK) dissolved in trifluoroethanol (1 mL, Sigma). This solution was then added to a PVA solution (10 mL, 1% w/v in water) dropwise and stirred for 3 h. The NPs were then transferred to a dialysis membrane and dialysed (MWCO of 50 kDa, Spectrum Labs) against distilled water before freeze-drying. Then, NPs were coated with protamine sulfate (PS). -

Development and Validation of a Protein-Based Risk Score for Cardiovascular Outcomes Among Patients with Stable Coronary Heart Disease
Supplementary Online Content Ganz P, Heidecker B, Hveem K, et al. Development and validation of a protein-based risk score for cardiovascular outcomes among patients with stable coronary heart disease. JAMA. doi: 10.1001/jama.2016.5951 eTable 1. List of 1130 Proteins Measured by Somalogic’s Modified Aptamer-Based Proteomic Assay eTable 2. Coefficients for Weibull Recalibration Model Applied to 9-Protein Model eFigure 1. Median Protein Levels in Derivation and Validation Cohort eTable 3. Coefficients for the Recalibration Model Applied to Refit Framingham eFigure 2. Calibration Plots for the Refit Framingham Model eTable 4. List of 200 Proteins Associated With the Risk of MI, Stroke, Heart Failure, and Death eFigure 3. Hazard Ratios of Lasso Selected Proteins for Primary End Point of MI, Stroke, Heart Failure, and Death eFigure 4. 9-Protein Prognostic Model Hazard Ratios Adjusted for Framingham Variables eFigure 5. 9-Protein Risk Scores by Event Type This supplementary material has been provided by the authors to give readers additional information about their work. Downloaded From: https://jamanetwork.com/ on 10/02/2021 Supplemental Material Table of Contents 1 Study Design and Data Processing ......................................................................................................... 3 2 Table of 1130 Proteins Measured .......................................................................................................... 4 3 Variable Selection and Statistical Modeling ........................................................................................ -

Chimeric Antigen Receptor (CAR) T Cell Therapy for Metastatic Melanoma: Challenges and Road Ahead
cells Review Chimeric Antigen Receptor (CAR) T Cell Therapy for Metastatic Melanoma: Challenges and Road Ahead Tahereh Soltantoyeh 1,†, Behnia Akbari 1,† , Amirali Karimi 2, Ghanbar Mahmoodi Chalbatani 1 , Navid Ghahri-Saremi 1, Jamshid Hadjati 1, Michael R. Hamblin 3,4 and Hamid Reza Mirzaei 1,* 1 Department of Medical Immunology, School of Medicine, Tehran University of Medical Sciences, Tehran 1417613151, Iran; [email protected] (T.S.); [email protected] (B.A.); [email protected] (G.M.C.); [email protected] (N.G.-S.); [email protected] (J.H.) 2 School of Medicine, Tehran University of Medical Sciences, Tehran 1417613151, Iran; [email protected] 3 Laser Research Centre, Faculty of Health Science, University of Johannesburg, Doornfontein 2028, South Africa; [email protected] 4 Radiation Biology Research Center, Iran University of Medical Sciences, Tehran 1449614535, Iran * Correspondence: [email protected]; Tel.: +98-21-64053268; Fax: +98-21-66419536 † Equally contributed as first author. Abstract: Metastatic melanoma is the most aggressive and difficult to treat type of skin cancer, with a survival rate of less than 10%. Metastatic melanoma has conventionally been considered very difficult to treat; however, recent progress in understanding the cellular and molecular mechanisms involved in the tumorigenesis, metastasis and immune escape have led to the introduction of new therapies. Citation: Soltantoyeh, T.; Akbari, B.; These include targeted molecular therapy and novel immune-based approaches such as immune Karimi, A.; Mahmoodi Chalbatani, G.; checkpoint blockade (ICB), tumor-infiltrating lymphocytes (TILs), and genetically engineered T- Ghahri-Saremi, N.; Hadjati, J.; lymphocytes such as chimeric antigen receptor (CAR) T cells. -

Chemokines and Their Receptors in Rheumatoid Arthritis
ARTHRITIS & RHEUMATISM Vol. 52, No. 3, March 2005, pp 710–721 DOI 10.1002/art.20932 © 2005, American College of Rheumatology REVIEW Chemokines and Their Receptors in Rheumatoid Arthritis Future Targets? Alisa E. Koch Introduction tem was introduced in 2000, in which chemokines are considered as chemokine ligands, and each chemokine Rheumatoid arthritis (RA) is a chronic inflam- has been assigned a designation of CXCL, CCL, XCL, matory disease leading to joint destruction (1). In RA, or CX3CL1 (Figure 1) (10–12). In this report, both the migration of leukocytes into the synovial tissue (ST) former and new nomenclature are noted. occurs. These leukocytes and other cells in the ST, particularly RA ST fibroblasts, produce mediators of CXC chemokines have 2 conserved cysteines inflammation, including chemokines (1). Chemokines, separated by 1 unconserved amino acid (9,13) (Figure currently numbering more than 50, are chemotactic 1). CXC chemokines classically were thought to be cytokines that are important in recruitment of leuko- involved in the chemotaxis of neutrophils. Many chemo- cytes and angiogenesis. They exert chemotactic activity kines may have arisen from reduplication of ancestral toward a variety of cell types (2–7). Some chemokines, genes (13). Hence, CXC chemokines that act on neutro- particularly CXC chemokines containing the ELR motif, phils are clustered on chromosome 4q12–13 (13). How- are angiogenic. The last few years have seen a rapid ever, some genes of more newly discovered CXC che- development of studies aimed at targeting proinflamma- mokines that recruit lymphocytes tend to be located tory chemokines or their receptors in RA and animal away from the major clusters (13). -

QUANTITATIVE DETERMINATION of HUMAN INTERLEUKIN-8 Human
QUANTITATIVE DETERMINATION NEW PRODUCT OF HUMAN INTERLEUKIN-8 Human Interleukin-8 ELISA Sensitivity (0.5 pg/ml) Very good analytical characteristics Validated for human serum, plasma (EDTA, citrate, heparin) and saliva samples Preliminary population data CYTOKINES, CHEMOKINES AND RELATED MOLECULES IMMUNE RESPONSE, INFECTION AND INFLAMMATION ONCOLOGY ∙ PERIODONTITIS ∙ SEPSIS HUMAN INTERLEUKIN-8 ELISA Introduction Interleukin (IL)-8, a member of the C-X-C chemokine gastric, lung, melanoma, mesothelioma, ovarian, prostate, subfamily, is a key mediator of inflammation. It is a product renal, and thyroid) and hematological malignancies (AML, of the CXCL8 gene mapped to chromosome 4, namely CLL, Hodgkin’s lymphoma) [7]. Similarly, a close association 4q.12-q12. It is 3211 bp in length and contains 4 exons. between high serum IL-8 expression and disease progression The protein is initially produced as a precursor peptide of has been shown in several clinical studies of breast, colon, 99 amino acids which then undergoes cleavage to create ovarian, and prostate cancers, as well as in melanoma [7]. several active IL-8 isoforms, the predominant variants In various cancers, high IL-8 levels have been identified as a consist of 77 and/or 72 amino acids residues [1, 2]. IL-8 is prognostic factor and as a possible treatment target through expressed by several cell types such as activated monocytes inhibition of IL-8 production and/or blockage of IL-8 receptors and macrophages, T cells, neutrophils, NK cells and also [8]. endothelial cells, wide variety of epithelial cells and fibroblasts [3]. Interleukin-8 is a multifunctional mediator associated with inflammation where it plays a key role in recruitment of Interleukin 8 (IL-8/CXCL8), also known as neutrophil leukocytes to sites of infection or tissue injury [4]. -

CXCL4/Platelet Factor 4 Is an Agonist of CCR1 and Drives Human Monocyte Migration
This is a repository copy of CXCL4/Platelet Factor 4 is an agonist of CCR1 and drives human monocyte migration. White Rose Research Online URL for this paper: https://eprints.whiterose.ac.uk/132464/ Version: Published Version Article: Fox, James Martin orcid.org/0000-0002-2473-7029, Kausar, Fahima, Day, Amy et al. (7 more authors) (2018) CXCL4/Platelet Factor 4 is an agonist of CCR1 and drives human monocyte migration. Scientific Reports. 9466. ISSN 2045-2322 Reuse This article is distributed under the terms of the Creative Commons Attribution (CC BY) licence. This licence allows you to distribute, remix, tweak, and build upon the work, even commercially, as long as you credit the authors for the original work. More information and the full terms of the licence here: https://creativecommons.org/licenses/ Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ www.nature.com/scientificreports OPEN CXCL4/Platelet Factor 4 is an agonist of CCR1 and drives human monocyte migration Received: 10 March 2016 James M. Fox 1,3, Fahima Kausar1, Amy Day1, Michael Osborne1, Khansa Hussain1, Accepted: 5 June 2018 Anja Mueller1,4, Jessica Lin1, Tomoko Tsuchiya 2, Shiro Kanegasaki2 & James E. Pease1 Published: xx xx xxxx Activated platelets release micromolar concentrations of the chemokine CXCL4/Platelet Factor-4. Deposition of CXCL4 onto the vascular endothelium is involved in atherosclerosis, facilitating monocyte arrest and recruitment by an as yet, unidentified receptor. -
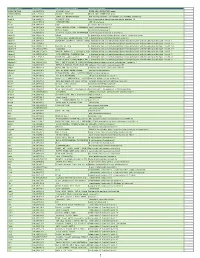
Myeloid Innate Immunity Mouse Vapril2018
Official Symbol Accession Alias / Previous Symbol Official Full Name 2810417H13Rik NM_026515.2 p15(PAF), Pclaf RIKEN cDNA 2810417H13 gene 2900026A02Rik NM_172884.3 Gm449, LOC231620 RIKEN cDNA 2900026A02 gene Abcc8 NM_011510.3 SUR1, Sur, D930031B21Rik ATP-binding cassette, sub-family C (CFTR/MRP), member 8 Acad10 NM_028037.4 2410021P16Rik acyl-Coenzyme A dehydrogenase family, member 10 Acly NM_134037.2 A730098H14Rik ATP citrate lyase Acod1 NM_008392.1 Irg1 aconitate decarboxylase 1 Acot11 NM_025590.4 Thea, 2010309H15Rik, 1110020M10Rik,acyl-CoA Them1, thioesterase BFIT1 11 Acot3 NM_134246.3 PTE-Ia, Pte2a acyl-CoA thioesterase 3 Acox1 NM_015729.2 Acyl-CoA oxidase, AOX, D130055E20Rikacyl-Coenzyme A oxidase 1, palmitoyl Adam19 NM_009616.4 Mltnb a disintegrin and metallopeptidase domain 19 (meltrin beta) Adam8 NM_007403.2 CD156a, MS2, E430039A18Rik, CD156a disintegrin and metallopeptidase domain 8 Adamts1 NM_009621.4 ADAM-TS1, ADAMTS-1, METH-1, METH1a disintegrin-like and metallopeptidase (reprolysin type) with thrombospondin type 1 motif, 1 Adamts12 NM_175501.2 a disintegrin-like and metallopeptidase (reprolysin type) with thrombospondin type 1 motif, 12 Adamts14 NM_001081127.1 Adamts-14, TS14 a disintegrin-like and metallopeptidase (reprolysin type) with thrombospondin type 1 motif, 14 Adamts17 NM_001033877.4 AU023434 a disintegrin-like and metallopeptidase (reprolysin type) with thrombospondin type 1 motif, 17 Adamts2 NM_001277305.1 hPCPNI, ADAM-TS2, a disintegrin and ametalloproteinase disintegrin-like and with metallopeptidase thrombospondin