Immunology of the Allergic Response 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Genetic Basis of Interindividual Variability in the Course of Infection
Human genetic basis of interindividual variability in the course of infection Jean-Laurent Casanovaa,b,c,d,e,1 aSt. Giles Laboratory of Human Genetics of Infectious Diseases, Rockefeller Branch, The Rockefeller University, New York, NY 10065; bHoward Hughes Medical Institute, New York, NY 10065; cLaboratory of Human Genetics of Infectious Diseases, Necker Branch, Inserm U1163, Necker Hospital for Sick Children, 75015 Paris, France; dImagine Institute, Paris Descartes University, 75015 Paris, France; and ePediatric Hematology and Immunology Unit, Assistance Publique–Hôpitaux de Paris, Necker Hospital for Sick Children, 75015 Paris, France This contribution is part of the special series of Inaugural Articles by members of the National Academy of Sciences elected in 2015. Contributed by Jean-Laurent Casanova, November 2, 2015 (sent for review September 15, 2015; reviewed by Max D. Cooper and Richard A. Gatti) The key problem in human infectious diseases was posed at the immunity (cell-autonomous mechanisms), then of cell-extrinsic turn of the 20th century: their pathogenesis. For almost any given innate immunity (phagocytosis of pathogens by professional cells), virus, bacterium, fungus, or parasite, life-threatening clinical disease and, finally, of cell-extrinsic adaptive immunity (somatic di- develops in only a small minority of infected individuals. Solving this versification of antigen-specific cells). Understanding the patho- infection enigma is important clinically, for diagnosis, prognosis, genesis of infectious diseases, particularly -

Allergens Immunoglobulin E (Ige) Antibodies
Allergens − Immunoglobulin E (IgE) Antibodies Single Allergen IgE Antibody This test is principally useful to confirm the allergen specificity in patients with clinically documented allergic disease. Therefore, requests for these tests should be made after a careful and comprehensive medical history is taken. Utilized in this manner, a single allergen immunoglobulin E (IgE) antibody test is cost-effective. A positive result may indicate that allergic signs and symptoms are caused by exposure to the specific allergen. Multi-allergen IgE Antibodies Profile Tests A number of related allergens are grouped together for ordering convenience. Each is tested individually and reported. Sample volume requirements are the same as if the tests were ordered individually. Panel Tests A pooled allergen reagent is used for each panel; therefore, the panel is reported with a single qualitative class result and concentration. The multi-allergen IgE antibody panel, combined with measurement of IgE in serum, is an appropriate first-order test for allergic disease. Positive results indicate the possibility of allergic disease induced by one or more allergens present in the multi-allergen panel. Negative results may rule out allergy, except in rare cases of allergic disease induced by exposure to a single allergen. Panel testing requires less specimen volume and less cost for ruling out allergic response; however, individual (single) allergen responses cannot be identified. In cases of a positive panel test, follow-up testing must be performed to differentiate between individual allergens in the panel. Note: Only 1 result is generated for each panel. Panels may be ordered with or without concurrent measurement of total IgE. -

ALLERGIC REACTIONS/ANAPHYLAXIS Connie J
Northwest Community EMS System Paramedic Education Program ALLERGIC REACTIONS/ANAPHYLAXIS Connie J. Mattera, M.S., R.N., EMT-P Reading assignments Text-Vol.1 pp. 235, 1272-1276 SOP: Allergic Reactions/ Anaphylactic Shock Assumed knowledge: Drugs: Epinephrine 1:1,000, 1:10,000; albuterol, ipratropium, dopamine, glucagon KNOWLEDGE OBJECTIVES Upon reading the assigned text assignments and completion of the class and homework questions, each participant will independently do the following with at least an 80% degree of accuracy and no critical errors: 1. Define allergic reaction. 2. Describe the incidence, morbidity and mortality of allergic reactions and anaphylaxis. 3. Identify risk factors that predispose a patient to anaphylaxis. 4. Explain the physiology of the immune system following exposure to an allergen including activation of histamine receptors and the formation of antibodies. 5. Discuss the pathophysiology of allergic reactions and anaphylaxis. 6. Describe the common modes by which allergens enter the body. 7. Compare and contrast natural and acquired and active vs. passive immunity. 8. Identify antigens most frequently associated with anaphylaxis. 9. Differentiate the clinical presentation and severity of risk for a mild, moderate and severe allergic reaction with an emphasis on recognizing an anaphylactic reaction. 10. Integrate the pathophysiologic principles of anaphylaxis with treatment priorities. 11. Sequence care per SOP for patients with mild, moderate and severe allergic reactions. CJM: S14 NWC EMSS Paramedic Education Program ALLERGIC REACTIONS/ANAPHYLAXIS Connie J. Mattera, M.S., R.N., EMT-P I. Immune system A. Principal body system involved in allergic reactions. Others include the cutaneous, cardiovascular, respiratory, nervous, and gastrointestinal systems. -
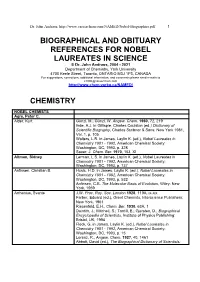
Biographical References for Nobel Laureates
Dr. John Andraos, http://www.careerchem.com/NAMED/Nobel-Biographies.pdf 1 BIOGRAPHICAL AND OBITUARY REFERENCES FOR NOBEL LAUREATES IN SCIENCE © Dr. John Andraos, 2004 - 2021 Department of Chemistry, York University 4700 Keele Street, Toronto, ONTARIO M3J 1P3, CANADA For suggestions, corrections, additional information, and comments please send e-mails to [email protected] http://www.chem.yorku.ca/NAMED/ CHEMISTRY NOBEL CHEMISTS Agre, Peter C. Alder, Kurt Günzl, M.; Günzl, W. Angew. Chem. 1960, 72, 219 Ihde, A.J. in Gillispie, Charles Coulston (ed.) Dictionary of Scientific Biography, Charles Scribner & Sons: New York 1981, Vol. 1, p. 105 Walters, L.R. in James, Laylin K. (ed.), Nobel Laureates in Chemistry 1901 - 1992, American Chemical Society: Washington, DC, 1993, p. 328 Sauer, J. Chem. Ber. 1970, 103, XI Altman, Sidney Lerman, L.S. in James, Laylin K. (ed.), Nobel Laureates in Chemistry 1901 - 1992, American Chemical Society: Washington, DC, 1993, p. 737 Anfinsen, Christian B. Husic, H.D. in James, Laylin K. (ed.), Nobel Laureates in Chemistry 1901 - 1992, American Chemical Society: Washington, DC, 1993, p. 532 Anfinsen, C.B. The Molecular Basis of Evolution, Wiley: New York, 1959 Arrhenius, Svante J.W. Proc. Roy. Soc. London 1928, 119A, ix-xix Farber, Eduard (ed.), Great Chemists, Interscience Publishers: New York, 1961 Riesenfeld, E.H., Chem. Ber. 1930, 63A, 1 Daintith, J.; Mitchell, S.; Tootill, E.; Gjersten, D., Biographical Encyclopedia of Scientists, Institute of Physics Publishing: Bristol, UK, 1994 Fleck, G. in James, Laylin K. (ed.), Nobel Laureates in Chemistry 1901 - 1992, American Chemical Society: Washington, DC, 1993, p. 15 Lorenz, R., Angew. -

Neoantigen Prevents Allergic Sensitization to a Initial High-Dose Nasal Allergen Exposure
Initial High-Dose Nasal Allergen Exposure Prevents Allergic Sensitization to a Neoantigen This information is current as Marc A. Riedl, Elliot M. Landaw, Andrew Saxon and David of September 28, 2021. Diaz-Sanchez J Immunol 2005; 174:7440-7445; ; doi: 10.4049/jimmunol.174.11.7440 http://www.jimmunol.org/content/174/11/7440 Downloaded from References This article cites 45 articles, 15 of which you can access for free at: http://www.jimmunol.org/content/174/11/7440.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 28, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2005 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Initial High-Dose Nasal Allergen Exposure Prevents Allergic Sensitization to a Neoantigen1 Marc A. Riedl,2* Elliot M. Landaw,† Andrew Saxon,* and David Diaz-Sanchez* Primary allergic sensitization—IgE formation after Ag exposure—is fundamental in the development of allergic respiratory disease. -

The Rhesus Factor and Disease Prevention
THE RHESUS FACTOR AND DISEASE PREVENTION The transcript of a Witness Seminar held by the Wellcome Trust Centre for the History of Medicine at UCL, London, on 3 June 2003 Edited by D T Zallen, D A Christie and E M Tansey Volume 22 2004 ©The Trustee of the Wellcome Trust, London, 2004 First published by the Wellcome Trust Centre for the History of Medicine at UCL, 2004 The Wellcome Trust Centre for the History of Medicine at University College London is funded by the Wellcome Trust, which is a registered charity, no. 210183. ISBN 978 0 85484 099 1 Histmed logo images courtesy Wellcome Library, London. Design and production: Julie Wood at Shift Key Design 020 7241 3704 All volumes are freely available online at: www.history.qmul.ac.uk/research/modbiomed/wellcome_witnesses/ Please cite as : Zallen D T, Christie D A, Tansey E M. (eds) (2004) The Rhesus Factor and Disease Prevention. Wellcome Witnesses to Twentieth Century Medicine, vol. 22. London: Wellcome Trust Centre for the History of Medicine at UCL. CONTENTS Illustrations and credits v Witness Seminars: Meetings and publications;Acknowledgements vii E M Tansey and D A Christie Introduction Doris T Zallen xix Transcript Edited by D T Zallen, D A Christie and E M Tansey 1 References 61 Biographical notes 75 Glossary 85 Index 89 Key to cover photographs ILLUSTRATIONS AND CREDITS Figure 1 John Walker-Smith performs an exchange transfusion on a newborn with haemolytic disease. Photograph provided by Professor John Walker-Smith. Reproduced with permission of Memoir Club. 13 Figure 2 Radiograph taken on day after amniocentesis for bilirubin assessment and followed by contrast (1975). -

Bourne Lecture
“One Medicine: the Continuum of Medicine, Veterinary Medicine and Biomedical Science”. Bourne Lecture. 12th February 2007. St Georges Medical School , Grenada. Ian McConnell , Professor of Veterinary Science, Department of Veterinary Medicine, University of Cambridge, England, United Kingdom. Introduction. Chancellor, Provost , Ladies and Gentlemen. Thank you , Provost, for your generous introduction. It is indeed an honour to be invited to give this years Bourne lecture in memory of Geoffrey Bourne . Geoffrey Bourne , your first Vice Chancellor who as an educator and scientist who had the vision to create here in this marvellous country of Grenada a most remarkable medical school which later evolved under the leadership of Keith Taylor, as Vice Chancellor, into what is today- a thriving and confident young University. St George’s University is an internationally recognised institution of higher education which has set a dynamic global perspective and can rightly claim to be a stratgically important landmark of learning in the West Indies. In this lecture I am going to address the topic of “ One Medicine”. I have chosen this as a topic because it seems appropriate to the St. George’s Medical School and the close relationship it has with the veterinary school. The development of the veterinary school owes much to the foresight and drive of Peter Bourne, who as Vice Chancellor, fostered the development of veterinary medicine. In the long history of both the Medical and the Veterinary Professions and the education of undergraduates in both there has always been a healthy interaction between medicine, veterinary medicine as well as biomedical science. The co-location of a medical school with a veterinary school which you have here is one way to promote this interaction . -

Xii World Asthma, Allergy & Copd Forum
XII WORLD ASTHMA, ALLERGY & COPD FORUM Saint Petersburg, Russia June 29–July 2, 2019 SAINT PETERSBURG SAINT PROGRAM World Immunopathology XIII WORLD ASTHMA, Organization (WIPO) ALLERGY & COPD FORUM Saint-Petersburg, Russia July 2–5, 2020 General Information St. Pet The World Immunopathology Organization (WIPO) is a professional, non-profit organization. WIPO was created in December 2002, at the I World Congress on Immunopathology in Singapore. During these years, WIPO successfully organized many international congresses and regional and national meetings throughout See you in Saint Petersburg in 2020! the world all promoting basic and clinical research and giving an opportunity for exchanging ideas. WIPO is aimed at collecting and disseminating scientific information and providing training and continuous education in various fields of immunopathology. Aims and Mission Nowadays, immunopathology has become a multidisciplinary problem. The WIPO global mission is to promote through education and research activities worldwide: – basic and clinical research in experimental and clinical immunology, allergy and asthma, autoimmunity, immunodeficiency, AIDS, immunobiotechnology, – prevention and treatment of different manifestations of immunopathology—immune-associated disorders, – excellence in patient care in this very important area of medicine and to establish communication between specialists in various fields of medical science and practice. e We encourage to join WIPO national and regional societies as well as individual members—doctors -

Allergy Markers in Respiratory Epidemiology
Copyright #ERS Journals Ltd 2001 Eur Respir J 2001; 17: 773±790 European Respiratory Journal Printed in UK ± all rights reserved ISSN 0903-1936 SERIES "CONTRIBUTIONS FROM THE EUROPEAN RESPIRATORY MONOGRAPHS" Edited by M. Decramer and A. Rossi Number 1 in thisSeries Allergy markers in respiratory epidemiology S. Baldacci*, E. Omenaas#, M.P. Oryszczyn} Allergy markers in respiratory epidemiology. S. Baldacci. #ERS Journals Ltd 2001. *Institute of Clinical Physiology, Pisa, ABSTRACT: Assessing allergy by measurement of serum immunoglobulin Ig) E Italy. #Dept of Thoracic Medicine, University of Bergen, Bergen, Norw- antibodies is fast and safe to perform. Serum antibodies can preferably be assessed in } patients with dermatitis and in those who regularly use antihistamines and other ay. INSERM U472, Villejuif, France. pharmacological agents that reduce skin sensitivity. Correspondence: S. Baldacci, Istituto di Skin tests represent the easiest tool to obtain quick and reliable information for the Fisiologia Clinica, CNR, Via Trieste diagnosis of respiratory allergic diseases. It is the technique more widely used, speci®c 41, 56126 Pisa, Italy. and reasonably sensitive for most applications as a marker of atopy. Fax: 39 50503596 Measurement of serum IgE antibodies and skin-prick testing may give complimentary information and can be applied in clinical and epidemiological settings. Keywords: Atopy, eosinophilia, epide- Peripheral blood eosinophilia is less used, but is important in clinical practice to miology, general population, immuno- demonstrate the allergic aetiology of disease, to monitor its clinical course and to globulin E, skin test reactivity address the choice of therapy. In epidemiology, hypereosinophilia seems to re¯ect an Received: December 11 2000 in¯ammatory reaction in the airways, which may be linked to obstructive air¯ow Accepted after revision December 15 limitation. -

Allergy – What’S in a Name?
HISTORY OF ENT Allergy – what’s in a name? BY KATHERINE CONROY llergy is defined as an “abnormal immune reaction to an ordinarily harmless substance” [1], however Athe meaning of the word has taken many forms since its introduction in 1906 by Austrian Paediatrician and Immunologist, Clemens von Pirquet [2]. Combining his observations on the paediatric wards, where infectious diseases, vaccinations and diphtheria serum sickness were commonplace, and his knowledge of immune reactions in the laboratory, von Pirquet devised the term ‘allergy’, roughly translating as ‘different reaction’ in Greek. It grouped together illnesses such as asthma, hay fever and eczema, and placed them on the same spectrum as acquired immunity from vaccinations and reactions to therapeutic toxins. His conclusions were extrapolated by Charles Mantoux to develop his tuberculin test two years later. Unfortunately, this theory linking Clemens von Pirquet with a patient. Image courtesy of Wellcome Collection - https://wellcomecollection.org/works/yd78ffbn immunity and hypersensitivity, and von Piquet’s subsequent inference that antibodies could be both protective and also include morbidity – as governments References 1. AAAAI. The American Academy of Allergy, Asthma harmful, was dismissed by many of his peers, realised the economic cost of chronic illness. Allergy became a clinical specialty in its & Immunology. www.aaaai.org/conditions-and- who instead supported French Physiologist, treatments/conditions-dictionary/allergy Last Charles Richet. Richet’s work on reinjection own right, with dedicated clinics, journals accessed October 2020. of dogs with sea anemone toxins showed and professional organisations in the 2. Jackson M. Allergy, The History of a Modern Malady. that a small, second dose could induce a interwar years. -

Genetic Testing
GENETIC TESTING The transcript of a Witness Seminar held by the Wellcome Trust Centre for the History of Medicine at UCL, London, on 13 July 2001 Edited by D A Christie and E M Tansey Volume 17 2003 CONTENTS Illustrations v Introduction Professor Peter Harper vii Acknowledgements ix Witness Seminars: Meetings and publications xi E M Tansey and D A Christie Transcript Edited by D A Christie and E M Tansey 1 References 73 Biographical notes 91 Glossary 105 Index 115 ILLUSTRATIONS Figure 1 Triploid cells in a human embryo, 1961. 20 Figure 2 The use of FISH with DNA probes from the X and Y chromosomes to sex human embryos. 62 v vi INTRODUCTION Genetic testing is now such a widespread and important part of medicine that it is hard to realize that it has almost all emerged during the past 30 years, with most of the key workers responsible for the discoveries and development of the field still living and active. This alone makes it a suitable subject for a Witness Seminar but there are others that increase its value, notably the fact that a high proportion of the critical advances took place in the UK; not just the basic scientific research, but also the initial applications in clinical practice, particularly those involving inherited disorders. To see these topics discussed by the people who were actually involved in their creation makes fascinating reading; for myself it is tinged with regret at having been unable to attend and contribute to the seminar, but with some compensation from being able to look at the contributions more objectively than can a participant. -

ÖGAI Symposium 2015 50 Years of B-Lymphocytes
ÖGAI Symposium 2015 50 Years of B-Lymphocytes Delineation of the Thymic and Bursal Lymphoid Systems in the Chicken. Cooper, MD, Peterson RD, Good RA Pediatric Res.Lab. of the Variety Club Heart Hospital, Univ. of Minnesota, Minn., USA Nature, 1965, 205:143-6 December 11-12, 2015 College of Physicians in Vienna, Billrothhaus 1090 Vienna, Frankgasse 8 PROGRAMME ABSTRACTS Welcome Dear guests, dear colleagues and friends, We cordially welcome you to the symposium ‘50 Years of B-Lymphocytes’ which is organized by the Austrian Society for Allergology and Immunology, ÖGAI, in Vienna, from December 11-12, 2015. With this symposium we are celebrating the discovery of B-lymphocytes, which play a key role in the defense against pathogens, tumors, and environmental factors potentially harming human beings. The understanding of B lymphocytes and antibodies produced by these cells is also crucial for the understanding of the large variety of diseases such as allergies, autoimmune diseases, immunodeficiencies and other immune-mediated diseases. The symposium will take place in the historical building of the College of Physicians in Vienna, the Billroth-Haus. The program consists of plenary lectures, given by outstanding international scientists, selected oral presentations by members of the Austrian Society for Allergology and Immunology, ÖGAI, and five poster sessions, which offer early career scientists to present their cutting edge research. On the occasion of this meeting the Austrian Society for Allergology and Immunology is proud to award the Clemens von Pirquet medal to Prof. Gabriel Pauli from Strasbourg, France, and the Karl Landsteiner Medal to Prof. Lorenzo Moretta from Rome, Italy.