Polymorphisms in GP6, PEAR1A, MRVI1, PIK3CG, JMJD1C, and SHH Genes in Patients with Unstable Angina
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mediator of DNA Damage Checkpoint 1 (MDC1) Is a Novel Estrogen Receptor Co-Regulator in Invasive 6 Lobular Carcinoma of the Breast 7 8 Evelyn K
bioRxiv preprint doi: https://doi.org/10.1101/2020.12.16.423142; this version posted December 16, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. 1 Running Title: MDC1 co-regulates ER in ILC 2 3 Research article 4 5 Mediator of DNA damage checkpoint 1 (MDC1) is a novel estrogen receptor co-regulator in invasive 6 lobular carcinoma of the breast 7 8 Evelyn K. Bordeaux1+, Joseph L. Sottnik1+, Sanjana Mehrotra1, Sarah E. Ferrara2, Andrew E. Goodspeed2,3, James 9 C. Costello2,3, Matthew J. Sikora1 10 11 +EKB and JLS contributed equally to this project. 12 13 Affiliations 14 1Dept. of Pathology, University of Colorado Anschutz Medical Campus 15 2Biostatistics and Bioinformatics Shared Resource, University of Colorado Comprehensive Cancer Center 16 3Dept. of Pharmacology, University of Colorado Anschutz Medical Campus 17 18 Corresponding author 19 Matthew J. Sikora, PhD.; Mail Stop 8104, Research Complex 1 South, Room 5117, 12801 E. 17th Ave.; Aurora, 20 CO 80045. Tel: (303)724-4301; Fax: (303)724-3712; email: [email protected]. Twitter: 21 @mjsikora 22 23 Authors' contributions 24 MJS conceived of the project. MJS, EKB, and JLS designed and performed experiments. JLS developed models 25 for the project. EKB, JLS, SM, and AEG contributed to data analysis and interpretation. SEF, AEG, and JCC 26 developed and performed informatics analyses. MJS wrote the draft manuscript; all authors read and revised the 27 manuscript and have read and approved of this version of the manuscript. -

Genome-Wide Association Study Identifies Loci for Arterial Stiffness
www.nature.com/scientificreports OPEN Genome-wide association study identifes loci for arterial stifness index in 127,121 UK Biobank Received: 1 February 2019 Accepted: 5 June 2019 participants Published: xx xx xxxx Kenneth Fung1, Julia Ramírez 2, Helen R. Warren2,3, Nay Aung 1, Aaron M. Lee1, Evan Tzanis2,3, Stefen E. Petersen 1,3 & Patricia B. Munroe2,3 Arterial stifness index (ASI) is a non-invasive measure of arterial stifness using infra-red fnger sensors (photoplethysmography). It is a well-suited measure for large populations as it is relatively inexpensive to perform, and data can be acquired within seconds. These features raise interest in using ASI as a tool to estimate cardiovascular disease risk as prior work demonstrates increased arterial stifness is associated with elevated systolic blood pressure, and ASI is predictive of cardiovascular disease and mortality. We conducted genome-wide association studies (GWASs) for ASI in 127,121 UK Biobank participants of European-ancestry. Our primary analyses identifed variants at four loci reaching genome-wide signifcance (P < 5 × 10−8): TEX41 (rs1006923; P = 5.3 × 10−12), FOXO1 (rs7331212; P = 2.2 × 10−11), C1orf21 (rs1930290, P = 1.1 × 10−8) and MRVI1 (rs10840457, P = 3.4 × 10−8). Gene- based testing revealed three signifcant genes, the most signifcant gene was COL4A2 (P = 1.41 × 10−8) encoding type IV collagen. Other candidate genes at associated loci were also involved in smooth muscle tone regulation. Our fndings provide new information for understanding the development of arterial stifness. Arterial stifness measures have been reported as independent markers of vascular ageing1,2, hypertension3,4, car- diovascular disease (CVD)5,6 and mortality6,7. -

Supplementary Materials
Supplementary materials Supplementary Table S1: MGNC compound library Ingredien Molecule Caco- Mol ID MW AlogP OB (%) BBB DL FASA- HL t Name Name 2 shengdi MOL012254 campesterol 400.8 7.63 37.58 1.34 0.98 0.7 0.21 20.2 shengdi MOL000519 coniferin 314.4 3.16 31.11 0.42 -0.2 0.3 0.27 74.6 beta- shengdi MOL000359 414.8 8.08 36.91 1.32 0.99 0.8 0.23 20.2 sitosterol pachymic shengdi MOL000289 528.9 6.54 33.63 0.1 -0.6 0.8 0 9.27 acid Poricoic acid shengdi MOL000291 484.7 5.64 30.52 -0.08 -0.9 0.8 0 8.67 B Chrysanthem shengdi MOL004492 585 8.24 38.72 0.51 -1 0.6 0.3 17.5 axanthin 20- shengdi MOL011455 Hexadecano 418.6 1.91 32.7 -0.24 -0.4 0.7 0.29 104 ylingenol huanglian MOL001454 berberine 336.4 3.45 36.86 1.24 0.57 0.8 0.19 6.57 huanglian MOL013352 Obacunone 454.6 2.68 43.29 0.01 -0.4 0.8 0.31 -13 huanglian MOL002894 berberrubine 322.4 3.2 35.74 1.07 0.17 0.7 0.24 6.46 huanglian MOL002897 epiberberine 336.4 3.45 43.09 1.17 0.4 0.8 0.19 6.1 huanglian MOL002903 (R)-Canadine 339.4 3.4 55.37 1.04 0.57 0.8 0.2 6.41 huanglian MOL002904 Berlambine 351.4 2.49 36.68 0.97 0.17 0.8 0.28 7.33 Corchorosid huanglian MOL002907 404.6 1.34 105 -0.91 -1.3 0.8 0.29 6.68 e A_qt Magnogrand huanglian MOL000622 266.4 1.18 63.71 0.02 -0.2 0.2 0.3 3.17 iolide huanglian MOL000762 Palmidin A 510.5 4.52 35.36 -0.38 -1.5 0.7 0.39 33.2 huanglian MOL000785 palmatine 352.4 3.65 64.6 1.33 0.37 0.7 0.13 2.25 huanglian MOL000098 quercetin 302.3 1.5 46.43 0.05 -0.8 0.3 0.38 14.4 huanglian MOL001458 coptisine 320.3 3.25 30.67 1.21 0.32 0.9 0.26 9.33 huanglian MOL002668 Worenine -

DIPPER, a Spatiotemporal Proteomics Atlas of Human Intervertebral Discs
TOOLS AND RESOURCES DIPPER, a spatiotemporal proteomics atlas of human intervertebral discs for exploring ageing and degeneration dynamics Vivian Tam1,2†, Peikai Chen1†‡, Anita Yee1, Nestor Solis3, Theo Klein3§, Mateusz Kudelko1, Rakesh Sharma4, Wilson CW Chan1,2,5, Christopher M Overall3, Lisbet Haglund6, Pak C Sham7, Kathryn Song Eng Cheah1, Danny Chan1,2* 1School of Biomedical Sciences, , The University of Hong Kong, Hong Kong; 2The University of Hong Kong Shenzhen of Research Institute and Innovation (HKU-SIRI), Shenzhen, China; 3Centre for Blood Research, Faculty of Dentistry, University of British Columbia, Vancouver, Canada; 4Proteomics and Metabolomics Core Facility, The University of Hong Kong, Hong Kong; 5Department of Orthopaedics Surgery and Traumatology, HKU-Shenzhen Hospital, Shenzhen, China; 6Department of Surgery, McGill University, Montreal, Canada; 7Centre for PanorOmic Sciences (CPOS), The University of Hong Kong, Hong Kong Abstract The spatiotemporal proteome of the intervertebral disc (IVD) underpins its integrity *For correspondence: and function. We present DIPPER, a deep and comprehensive IVD proteomic resource comprising [email protected] 94 genome-wide profiles from 17 individuals. To begin with, protein modules defining key †These authors contributed directional trends spanning the lateral and anteroposterior axes were derived from high-resolution equally to this work spatial proteomes of intact young cadaveric lumbar IVDs. They revealed novel region-specific Present address: ‡Department profiles of regulatory activities -

Impaired Iloprost-Induced Platelet Inhibition and Phosphoproteome Changes in Patients with Confirmed Pseudohypoparathyroidism Ty
www.nature.com/scientificreports OPEN Impaired iloprost‑induced platelet inhibition and phosphoproteome changes in patients with confrmed pseudohypoparathyroidism type Ia, linked to genetic mutations in GNAS Frauke Swieringa1,2, Fiorella A. Solari1,9, Oliver Pagel1,9, Florian Beck1, Jingnan Huang1,2, Marion A. H. Feijge2, Kerstin Jurk4, Irene M. L. W. Körver‑Keularts5, Nadine J. A. Mattheij2, Jörg Faber3, Joachim Pohlenz3, Alexandra Russo3, Connie T. R. M. Stumpel5,6, Dirk E. Schrander7, Barbara Zieger8, Paola E. J. van der Meijden2, René P. Zahedi1, Albert Sickmann1 & Johan W. M. Heemskerk2* Patients diagnosed with pseudohypoparathyroidism type Ia (PHP Ia) sufer from hormonal resistance and abnormal postural features, in a condition classifed as Albright hereditary osteodystrophy (AHO) syndrome. This syndrome is linked to a maternally inherited mutation in the GNAS complex locus, encoding for the GTPase subunit Gsα. Here, we investigated how platelet phenotype and omics analysis can assist in the often difcult diagnosis. By coupling to the IP receptor, Gsα induces platelet inhibition via adenylyl cyclase and cAMP-dependent protein kinase A (PKA). In platelets from seven patients with suspected AHO, one of the largest cohorts examined, we studied the PKA-induced phenotypic changes. Five patients with a confrmed GNAS mutation, displayed impairments in Gsα- dependent VASP phosphorylation, aggregation, and microfuidic thrombus formation. Analysis of the platelet phosphoproteome revealed 2,516 phosphorylation sites, of which 453 were regulated by Gsα-PKA. Common changes in the patients were: (1) a joint panel of upregulated and downregulated phosphopeptides; (2) overall PKA dependency of the upregulated phosphopeptides; (3) links to key platelet function pathways. In one patient with GNAS mutation, diagnosed as non‑AHO, the changes in platelet phosphoproteome were reversed. -
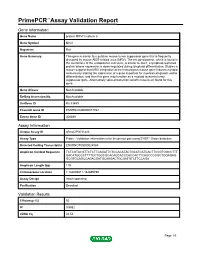
Primepcr™Assay Validation Report
PrimePCR™Assay Validation Report Gene Information Gene Name protein MRVI1 isoform b Gene Symbol Mrvi1 Organism Rat Gene Summary This gene is similar to a putative mouse tumor suppressor gene that is frequently disrupted by mouse AIDS-related virus (MRV). The encoded protein, which is found in the membrane of the endoplasmic reticulum, is similar to Jaw1, a lymphoid-restricted protein whose expression is down-regulated during lymphoid differentiation. Studies in mouse suggest that MRV integration at the homologous mouse gene induces myeloid leukemia by altering the expression of a gene important for myeloid cell growth and/or differentiation, and thus this gene may function as a myeloid leukemia tumor suppressor gene. Alternatively spliced transcript variants have been found for this gene. Gene Aliases Not Available RefSeq Accession No. Not Available UniGene ID Rn.33889 Ensembl Gene ID ENSRNOG00000017767 Entrez Gene ID 308899 Assay Information Unique Assay ID qRnoCIP0031443 Assay Type Probe - Validation information is for the primer pair using SYBR® Green detection Detected Coding Transcript(s) ENSRNOT00000024060 Amplicon Context Sequence TCTCGTACGTTCTCTTCAGATTCTCCACATACTGCATCATCACTTCCGTGGCCTTT GACATGCGCTTTTCCTGGCGCACAGCACCCACCACTTCAGCCCGGCTGGAGAG GCGTGCAGCCAGACGATGCAAGACTGCGATGTCTTCCAGA Amplicon Length (bp) 119 Chromosome Location 1:182696811-182699799 Assay Design Intron-spanning Purification Desalted Validation Results Efficiency (%) 95 R2 0.9982 cDNA Cq 24.54 Page 1/5 PrimePCR™Assay Validation Report cDNA Tm (Celsius) 88 gDNA Cq Specificity -

Mrvil, a Common MRV Integration Site in BXH2 Myeloid Leukemias, Encodes a Protein with Homology to a Lymphoid-Restricted Membrane Protein Jaw1
Oncogene (1999) 18, 2069 ± 2084 ã 1999 Stockton Press All rights reserved 0950 ± 9232/99 $12.00 http://www.stockton-press.co.uk/onc Mrvil, a common MRV integration site in BXH2 myeloid leukemias, encodes a protein with homology to a lymphoid-restricted membrane protein Jaw1 John D Shaughnessy Jr*,1, David A Largaespada2, Erming Tian1, Colin F Fletcher3, Brian C Cho4, Paresh Vyas5, Nancy A Jenkins3 and Neal G Copeland3 1Division of Hematology and Oncology, Department of Medicine, University of Arkansas for Medical Sciences, Little Rock, Arkansas, AR 72205, USA; 2Department of Laboratory Medicine and Pathology, University of Minnesota Cancer Center, Minneapolis, Minnesota, MN 55455, USA; 3Mammalian Genetics Laboratory, ABL-Basic Research Program, NCI-Frederick Cancer Research and Development Center, Frederick, Maryland, MD 21702, USA; 4Department of Microbiology and Immunology, Thomas Jeerson University Cancer Institute, Philadelphia, Pennsylvania, PA 19107, USA; 5Department of Hematology and Oncology, Children's Hospital, Boston, Massachusetts, USA Ecotropic MuLVs induce myeloid leukemia in BXH2 Introduction mice by insertional mutagenesis of cellular proto- oncogenes or tumor suppressor genes. Disease genes BXH2 mice represent an important model for the can thus be identi®ed by viral tagging as common sites of identi®cation of myeloid leukemia disease genes. Not viral integration in BXH2 leukemias. Previous studies only do these mice have the highest spontaneous showed that a frequent common integration site in BXH2 incidence of myeloid leukemia of any known inbred leukemias is the Nf1 tumor suppressor gene. Unexpect- mouse strain, but the leukemias in these mice are edly, about half of the viral integrations at Nf1 retrovirally-induced and the proviruses in the tumors represented a previously undiscovered defective none- can thus be used as insertional tags to identify the cotropic virus, termed MRV. -

Description: Uniprot:Q13976 Alternative Names: Specificity
TD2677 PRKG1 Antibody Order 021-34695924 [email protected] Support 400-6123-828 50ul [email protected] 100 uL √ √ Web www.ab-mart.com.cn Description: Serine/threonine protein kinase that acts as key mediator of the nitric oxide (NO)/cGMP signaling pathway. GMP binding activates PRKG1, which phosphorylates serines and threonines on many cellular proteins. Numerous protein targets for PRKG1 phosphorylation are implicated in modulating cellular calcium, but the contribution of each of these targets may vary substantially among cell types. Proteins that are phosphorylated by PRKG1 regulate platelet activation and adhesion, smooth muscle contraction, cardiac function, gene expression, feedback of the NO-signaling pathway, and other processes involved in several aspects of the CNS like axon guidance, hippocampal and cerebellar learning, circadian rhythm and nociception. Smooth muscle relaxation is mediated through lowering of intracellular free calcium, by desensitization of contractile proteins to calcium, and by decrease in the contractile state of smooth muscle or in platelet activation. Regulates intracellular calcium levels via several pathways: phosphorylates MRVI1/IRAG and inhibits IP3-induced Ca(2+) release from intracellular stores, phosphorylation of KCNMA1 (BKCa) channels decreases intracellular Ca(2+) levels, which leads to increased opening of this channel. PRKG1 phosphorylates the canonical transient receptor potential channel (TRPC) family which inactivates the associated inward calcium current. Another mode of action of NO/cGMP/PKGI signaling involves PKGI-mediated inactivation of the Ras homolog gene family member A (RhoA). Phosphorylation of RHOA by PRKG1 blocks the action of this protein in myriad processes: regulation of RHOA translocation; decreasing contraction; controlling vesicle trafficking, reduction of myosin light chain phosphorylation resulting in vasorelaxation. -

Comprehensive Analysis of Expression and Prognostic Value for JMJD5 and PKM2 in Stomach Adenocarcinoma
Comprehensive Analysis of Expression and Prognostic Value for JMJD5 and PKM2 in Stomach Adenocarcinoma Ling Qi Tumor Hospital of Harbin Medical University Li-Sha Li Tumor Hospital of Harbin Medical University Chao Zhan Tumor Hospital of Harbin Medical University Ming-Xia Jiang Tumor Hospital of Harbin Medical University Dong-Feng Song Tumor Hospital of Harbin Medical University Yi-Ming Wu Tumor Hospital of Harbin Medical University Jun-Qing Gan Tumor Hospital of Harbin Medical University Ke-Xin Jin Tumor Hospital of Harbin Medical University Mei Huang Tumor Hospital of Harbin Medical University yanjing Li ( [email protected] ) Tumor Hospital of Harbin Medical University https://orcid.org/0000-0003-0174-2017 Xiao-Xue Du Tumor Hospital of Harbin Medical University Cheng-Xin Song Tumor Hospital of Harbin Medical University Primary research Keywords: JMJD family, JMJD5, PKM2, stomach adenocarcinoma, bioinformatics analysis Posted Date: June 7th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-569965/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/18 Abstract Background: Jumonji C-domain-containing (JMJD) family, a group of genes that regulate epigenetics, is involved in tumor development in several types of cancer. JMJD5 is a member of the JMJD family, and its clinical impact on stomach adenocarcinoma (STAD) remains unclear. Pyruvate kinase M2 (PKM2) promotes metabolism, tumor proliferation, and metastasis in various cancer types. However, the relationship between JMJD5 and PKM2 in STAD is yet to be established. In this study, we investigated the expressions and relationship of JMJD5 and PKM2 in patients with STAD. -
Anti-MRVI1 (Aa 404-547) Polyclonal Antibody (DPABH-03411) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-MRVI1 (aa 404-547) polyclonal antibody (DPABH-03411) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description This gene is similar to a putative mouse tumor suppressor gene (Mrvi1) that is frequently disrupted by mouse AIDS-related virus (MRV). The encoded protein, which is found in the membrane of the endoplasmic reticulum, is similar to Jaw1, a lymphoid-restricted protein whose expression is downregulated during lymphoid differentiation. Studies in mouse suggest that MRV integration at Mrvi1 induces myeloid leukemia by altering the expression of a gene important for myeloid cell growth and/or differentiation, and thus this gene may function as a myeloid leukemia tumor suppressor gene. Several alternatively spliced transcript variants encoding different isoforms have been found for this gene, few of which initiate translation at a non-AUG (CUG) start site. Immunogen Recombinant fragment, corresponding to a region within amino acids 404-547 of Human MRVI1 Isotype IgG Source/Host Rabbit Species Reactivity Human Purification Immunogen affinity purified Conjugate Unconjugated Applications WB, IHC-P Format Liquid Size 100 μl Buffer pH: 7.00; Constituents: 78% PBS, 20% Glycerol, 1% BSA Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. GENE INFORMATION 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Gene Name MRVI1 -

Epigenetic Regulation of Acute Myeloid Leukaemic Stem Cells
Epigenetic Regulation of Acute Myeloid Leukaemic Stem Cells Halina Hoi Laam Leung Bachelor of Medicinal Chemistry Advanced (Honours Class 1) A thesis submitted in fulfilment of the requirements for the degree of Doctor of Philosophy Children‘s Cancer Institute Australia for Medical Research School of Women‘s and Children‘s Health Faculty of Medicine University of New South Wales November 2015 PLEASE TYPE THE UNIVERSITY OF NEW SOUTH WALES Thesis/Dissertation Sheet Surname or Family name: Leung First name: Halina Other name/s: Hoi Laam Abbreviation for degree as given in the University calendar: PhD School: Women’s and Children’s Health Faculty: Medicine Title: Epigenetic Regulation of Acute Myeloid Leukaemic Stem Cells Abstract 350 words maximum: (PLEASE TYPE) Acute myeloid leukaemia (AML) is a heterogeneous blood disease with high relapse rates. A small population of highly drug resistant leukaemic stem cells (LSC) persists after chemotherapy, causing disease relapse. This emphasises the need to develop novel LSC-targeted therapies. While increasing evidence has emerged in recent years highlighting the role of epigenetic regulators in cancer development and maintenance, knowledge in epigenetic regulation of LSC is limited. This study investigated the role of two novel histone demethylases, Jmjd1c and Jmjd5, in regulating LSC, as well as the effectiveness of currently available epigenetic agents on leukaemogenesis. This study has shown that Jmjd1c is required for AML development and maintenance. Experiments involving enforced expression of Jmjd1c in haematopoietic stem cells (HSC) suggested that Jmjd1c has the capacity to enhance stem cell proliferation. Jmjd1c overexpression also promoted proliferation of HSC transduced with oncogenes, Hoxa9/Meis1a, and accelerated leukaemia development in mice. -

Multipronged Approach to Study Glaucoma-Associated Phenotypes
University of Tennessee Health Science Center UTHSC Digital Commons Theses and Dissertations (ETD) College of Graduate Health Sciences 8-2016 Multipronged Approach to Study Glaucoma- Associated Phenotypes Sumana Rameshbabu Chintalapudi University of Tennessee Health Science Center Follow this and additional works at: https://dc.uthsc.edu/dissertations Part of the Neurosciences Commons Recommended Citation Chintalapudi, Sumana Rameshbabu (http://orcid.org/0000-0003-1079-0950), "Multipronged Approach to Study Glaucoma- Associated Phenotypes" (2016). Theses and Dissertations (ETD). Paper 404. http://dx.doi.org/10.21007/etd.cghs.2016.0410. This Dissertation is brought to you for free and open access by the College of Graduate Health Sciences at UTHSC Digital Commons. It has been accepted for inclusion in Theses and Dissertations (ETD) by an authorized administrator of UTHSC Digital Commons. For more information, please contact [email protected]. Multipronged Approach to Study Glaucoma-Associated Phenotypes Document Type Dissertation Degree Name Doctor of Philosophy (PhD) Program Integrated Program in Biomedical Sciences Track Neuroscience Research Advisor Monica M. Jablonski, Ph.D. Committee Edward Chaum, M.D., Ph.D. Dianna A. Johnson, Ph.D. Rajendra Raghow, Ph.D. Vanessa Morales-Tirado, Ph.D. Robert W. Williams, Ph.D. ORCID http://orcid.org/0000-0003-1079-0950 DOI 10.21007/etd.cghs.2016.0410 Comments One year embargo expires August 2017. This dissertation is available at UTHSC Digital Commons: https://dc.uthsc.edu/dissertations/404 Multipronged Approach to Study Glaucoma-Associated Phenotypes A Dissertation Presented for The Graduate Studies Council The University of Tennessee Health Science Center In Partial Fulfillment Of the Requirements for the Degree Doctor of Philosophy From The University of Tennessee By Sumana Rameshbabu Chintalapudi August 2016 .