Prevalence and Characterization of Staphylococcus Species
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Review Article: Inhibition of Methanogenic Archaea by Statins As a Targeted Management Strategy for Constipation and Related Disorders
Alimentary Pharmacology and Therapeutics Review article: inhibition of methanogenic archaea by statins as a targeted management strategy for constipation and related disorders K. Gottlieb*, V. Wacher*, J. Sliman* & M. Pimentel† *Synthetic Biologics, Inc., Rockville, SUMMARY MD, USA. † Gastroenterology, Cedars-Sinai Background Medical Center, Los Angeles, CA, USA. Observational studies show a strong association between delayed intestinal transit and the production of methane. Experimental data suggest a direct inhibitory activity of methane on the colonic and ileal smooth muscle and Correspondence to: a possible role for methane as a gasotransmitter. Archaea are the only con- Dr K. Gottlieb, Synthetic Biologics, fi Inc., 9605 Medical Center Drive, rmed biological sources of methane in nature and Methanobrevibacter Rockville, MD 20850, USA. smithii is the predominant methanogen in the human intestine. E-mail: [email protected] Aim To review the biosynthesis and composition of archaeal cell membranes, Publication data archaeal methanogenesis and the mechanism of action of statins in this context. Submitted 8 September 2015 First decision 29 September 2015 Methods Resubmitted 7 October 2015 Narrative review of the literature. Resubmitted 20 October 2015 Accepted 20 October 2015 Results EV Pub Online 11 November 2015 Statins can inhibit archaeal cell membrane biosynthesis without affecting This uncommissioned review article was bacterial numbers as demonstrated in livestock and humans. This opens subject to full peer-review. the possibility of a therapeutic intervention that targets a specific aetiologi- cal factor of constipation while protecting the intestinal microbiome. While it is generally believed that statins inhibit methane production via their effect on cell membrane biosynthesis, mediated by inhibition of the HMG- CoA reductase, there is accumulating evidence for an alternative or addi- tional mechanism of action where statins inhibit methanogenesis directly. -

Food Microbiology Changes in the Microbial Communities in Vacuum
Food Microbiology 77 (2019) 26–37 Contents lists available at ScienceDirect Food Microbiology journal homepage: www.elsevier.com/locate/fm Changes in the microbial communities in vacuum-packaged smoked bacon during storage T ∗ Xinfu Lia,b,d, Cong Lia,b,d, Hua Yea,b, Zhouping Wanga,b, Xiang Wud, Yanqing Hand, Baocai Xub,c,d, a State Key Laboratory of Food Science and Technology, Jiangnan University, Wuxi, 214122, China b School of Food Science and Technology, Jiangnan University, Wuxi, 214122, China c School of Food Science and Engineering, Hefei University of Technology, Hefei, 230009, China d State Key Laboratory of Meat Processing and Quality Control, Yurun Group, Nanjing, 211806, China ARTICLE INFO ABSTRACT Keywords: This study aimed to gain deeper insights into the microbiota composition and population dynamics, monitor the Microbial communities dominant bacterial populations and identify the specific spoilage microorganisms (SSOs) of vacuum-packed Smoked bacon bacon during refrigerated storage using both culture-independent and dependent methods. High-throughout High-throughput sequencing (HTS) sequencing (HTS) showed that the microbial composition changed greatly with the prolongation of storage time. The diversity of microbiota was abundant at the initial stage then experienced a continuous decrease. Lactic acid bacteria (LAB) mainly Leuconostoc and Lactobacillus dominated the microbial population after seven days of storage. A total of 26 isolates were identified from different growth media using traditional cultivation isolation and identification method. Leuconostoc mesenteroides and Leuconostoc carnosum were the most prevalent species since day 15, while Lactobacillus sakei and Lactobacillus curvatus were only found on day 45, suggesting that they could be responsible for the spoilage of bacon. -
Cell Structure and Function in the Bacteria and Archaea
4 Chapter Preview and Key Concepts 4.1 1.1 DiversityThe Beginnings among theof Microbiology Bacteria and Archaea 1.1. •The BacteriaThe are discovery classified of microorganismsinto several Cell Structure wasmajor dependent phyla. on observations made with 2. theThe microscope Archaea are currently classified into two 2. •major phyla.The emergence of experimental 4.2 Cellscience Shapes provided and Arrangements a means to test long held and Function beliefs and resolve controversies 3. Many bacterial cells have a rod, spherical, or 3. MicroInquiryspiral shape and1: Experimentation are organized into and a specific Scientificellular c arrangement. Inquiry in the Bacteria 4.31.2 AnMicroorganisms Overview to Bacterialand Disease and Transmission Archaeal 4.Cell • StructureEarly epidemiology studies suggested how diseases could be spread and 4. Bacterial and archaeal cells are organized at be controlled the cellular and molecular levels. 5. • Resistance to a disease can come and Archaea 4.4 External Cell Structures from exposure to and recovery from a mild 5.form Pili allowof (or cells a very to attach similar) to surfacesdisease or other cells. 1.3 The Classical Golden Age of Microbiology 6. Flagella provide motility. Our planet has always been in the “Age of Bacteria,” ever since the first 6. (1854-1914) 7. A glycocalyx protects against desiccation, fossils—bacteria of course—were entombed in rocks more than 3 billion 7. • The germ theory was based on the attaches cells to surfaces, and helps observations that different microorganisms years ago. On any possible, reasonable criterion, bacteria are—and always pathogens evade the immune system. have been—the dominant forms of life on Earth. -

(51) International Patent Classification: C12R 1/44 (2006.01) A23L 5/41
( (51) International Patent Classification: Published: C12R 1/44 (2006.01) A23L 5/41 (2016.01) — with international search report (Art. 21(3)) A23L 29/00 (20 16.0 1) A23L 13/40 (20 16.01) — with (an) indication(s) in relation to deposited biological (21) International Application Number: material furnished under Rule 13bis separately from the PCT/EP20 19/06 1422 description (Rules 13bis.4(d)(i) and 48.2(a) (viii)) (22) International Filing Date: 03 May 2019 (03.05.2019) (25) Filing Language: English (26) Publication Language: English (30) Priority Data: 18170807.4 04 May 2018 (04.05.2018) EP 18184186.7 18 July 2018 (18.07.2018) EP (71) Applicant: CHR. HANSEN A/S [DK/DK]; Boege Alle 10-12, 2970 Hoersholm (DK). (72) Inventors: THORSEN, Tina Mailing; c/o Chr. Hansen A/S, Boege Alle 10-12, 2970 Hoersholm (DK). BAROI, George Nabin; c/o Chr. Hansen A/S, Boege Alle 10-12, 2970 Hoersholm (DK). TAPONEN, Robin; c/o Chr. Hansen A/S, Boege Alle 10-12, 2970 Hoersholm (DK). SOELTOFT-JENSEN, Jakob; c/o Chr. Hansen A/S, Boege Alle 10-12, 2970 Hoersholm (DK). YDE, Birgitte; c/o Chr. Hansen A/S, Boege Alle 10-12, 2970 Hoersholm (DK). (81) Designated States (unless otherwise indicated, for every kind of national protection available) : AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

Possible Detection of Pathogenic Bacterial Species Inhabiting Streams in Great Smoky Mountains National Park
POSSIBLE DETECTION OF PATHOGENIC BACTERIAL SPECIES INHABITING STREAMS IN GREAT SMOKY MOUNTAINS NATIONAL PARK A thesis presented to the faculty of the Graduate School of Western Carolina University in partial fulfillment of the requirement for the degree of Master of Science in Biology. By Kwame Agyapong Brown Director: Dr. Sean O’Connell Associate Professor of Biology and Biology Department Head Committee members: Dr. Sabine Rundle and Dr. Timothy Driscoll November 2016 ACKNOWLEDGEMENTS I would like to express my deepest gratitude to my adviser Dr. Sean O’Connell for his insightful mentoring and thoughtful contribution throughout this research. I would also like to acknowledge my laboratory teammates: Lisa Dye, Rob McKinnon, Kacie Fraser, and Tori Carlson for their diverse contributions to this project. This project would not have been possible without the generous support of the Western Carolina University Biology Department and stockroom; so I would like to thank the entire WCU biology faculty and Wesley W. Bintz for supporting me throughout my Masters program. Finally, I would like to thank my thesis committee members and reader: Dr. Sabine Rundle, Dr. Timothy Driscoll and Dr. Anjana Sharma for their contributions to this project. ii TABLE OF CONTENTS List of Tables ................................................................................................................................. iv List of Figures ..................................................................................................................................v -

( 12 ) United States Patent
US009956282B2 (12 ) United States Patent ( 10 ) Patent No. : US 9 ,956 , 282 B2 Cook et al. (45 ) Date of Patent: May 1 , 2018 ( 54 ) BACTERIAL COMPOSITIONS AND (58 ) Field of Classification Search METHODS OF USE THEREOF FOR None TREATMENT OF IMMUNE SYSTEM See application file for complete search history . DISORDERS ( 56 ) References Cited (71 ) Applicant : Seres Therapeutics , Inc. , Cambridge , U . S . PATENT DOCUMENTS MA (US ) 3 ,009 , 864 A 11 / 1961 Gordon - Aldterton et al . 3 , 228 , 838 A 1 / 1966 Rinfret (72 ) Inventors : David N . Cook , Brooklyn , NY (US ) ; 3 ,608 ,030 A 11/ 1971 Grant David Arthur Berry , Brookline, MA 4 ,077 , 227 A 3 / 1978 Larson 4 ,205 , 132 A 5 / 1980 Sandine (US ) ; Geoffrey von Maltzahn , Boston , 4 ,655 , 047 A 4 / 1987 Temple MA (US ) ; Matthew R . Henn , 4 ,689 ,226 A 8 / 1987 Nurmi Somerville , MA (US ) ; Han Zhang , 4 ,839 , 281 A 6 / 1989 Gorbach et al. Oakton , VA (US ); Brian Goodman , 5 , 196 , 205 A 3 / 1993 Borody 5 , 425 , 951 A 6 / 1995 Goodrich Boston , MA (US ) 5 ,436 , 002 A 7 / 1995 Payne 5 ,443 , 826 A 8 / 1995 Borody ( 73 ) Assignee : Seres Therapeutics , Inc. , Cambridge , 5 ,599 ,795 A 2 / 1997 McCann 5 . 648 , 206 A 7 / 1997 Goodrich MA (US ) 5 , 951 , 977 A 9 / 1999 Nisbet et al. 5 , 965 , 128 A 10 / 1999 Doyle et al. ( * ) Notice : Subject to any disclaimer , the term of this 6 ,589 , 771 B1 7 /2003 Marshall patent is extended or adjusted under 35 6 , 645 , 530 B1 . 11 /2003 Borody U . -

Structure of Bacterial and Archaeal Cells
© Jones & Bartlett Learning, LLC. NOT FOR SALE OR DISTRIBUTION 4 CHAPTER PREVIEW 4.1 There Is Tremendous Diversity Structure of Among the Bacteria and Archaea 4.2 Prokaryotes Can Be Distinguished by Their Cell Shape and Arrangements Bacterial and 4.3 An Overview to Bacterial and Archaeal Cell Structure 4.4 External Cell Structures Interact Archaeal Cells with the Environment Investigating the Microbial World 4: Our planet has always been in the “Age of Bacteria,” ever since the The Role of Pili first fossils—bacteria of course—were entombed in rocks more than TexTbook Case 4: An Outbreak of 3 billion years ago. On any possible, reasonable criterion, bacteria Enterobacter cloacae Associated with a Biofilm are—and always have been—the dominant forms of life on Earth. —Paleontologist Stephen J. Gould (1941–2002) 4.5 Most Bacterial and Archaeal Cells Have a Cell Envelope “Double, double toil and trouble; Fire burn, and cauldron bubble” is 4.6 The Cell Cytoplasm Is Packed the refrain repeated several times by the chanting witches in Shakespeare’s with Internal Structures Macbeth (Act IV, Scene 1). This image of a hot, boiling cauldron actu- MiCroinquiry 4: The Prokaryote/ ally describes the environment in which many bacterial, and especially Eukaryote Model archaeal, species happily grow! For example, some species can be iso- lated from hot springs or the hot, acidic mud pits of volcanic vents ( Figure 4.1 ). When the eminent evolutionary biologist and geologist Stephen J. Gould wrote the opening quote of this chapter, he, as well as most micro- biologists at the time, had no idea that embedded in these “bacteria” was another whole domain of organisms. -

Rapid Automated Identification of Gram-Positive and Gram-Negative Bacteria in the Phoenixtm System J
As presented at the 99th General Meeting of the American Society for Microbiology, May 1999. Rapid Automated Identification of Gram-Positive and Gram-Negative Bacteria in the PhoenixTM System J. SALOMON, T. DUNK, C. YU, J. POLLITT, AND J. REUBEN BD Biosciences • 7 Loveton Circle • Sparks, MD, USA 21152 ABSTRACT I Feasibility of rapid and reliable identification of over 225 taxa that included gram-negative and gram-positive species was evaluated in the PhoenixTM Automated Microbiology System (BD Biosciences, Sparks, MD). The PHOENIX Phoenix system is intended for the rapid identification of clinically relevant aerobic bacteria without supplemental INTRODUCTION tests. Seventy-five glucose-fermenting and 50 glucose- Accurate and rapid identification of clinically relevant gram- positive and gram-negative bacteria is becoming increasingly more nonfermenting gram-negative species and isolates from important in infectious disease therapy. Bacterial identification with Staphylococcus, Streptococcus, Enterococcus, commercially available, miniaturized, automated and manual systems has been on the rise for decades. More recently, miniaturized Corynebacterium and Bacillus species were included in identification systems have successfully employed a combination of this evaluation. Additionally, a total of 74 isolates from biochemical and enzymatic substrates to identify bacteria to the species level. This study was conducted to determine the feasibility of Campylobacteraceae that included Campylobacter, rapid identification of aerobic, gram-positive and gram-negative bacteria in the Phoenix Automated Microbiology System (BD Helicobacter and Arcobacter species were also tested in Biosciences, Sparks, MD). Identification in the Phoenix system is this new system. All test strains were previously identified based on phenotypic profiles of bacterial reactivity in the presence of substrates that are kinetically monitored. -

The Pennsylvania State University
SCHREYER HONORS COLLEGE DEPARTMENT OF VETERINARY AND BIOMEDICAL SCIENCES CHARACTERIZATION OF THE NASAL BACTERIAL MICROFLORA OF HOUSEHOLD DOGS MARGARET ZEMANEK SPRING 2019 A thesis submitted in partial fulfillment of the requirements for a baccalaureate degree in Veterinary and Biomedical Sciences with honors in Veterinary and Biomedical Sciences Reviewed and approved* by the following: Bhushan Jayarao Professor of Veterinary and Biomedical Sciences Resident Director, Penn State Animal Diagnostic Laboratory Thesis Supervisor Lester Griel Jr. Professor Emeritus of Veterinary Sciences Honors Adviser * Signatures are on file in the Schreyer Honors College. i ABSTRACT In this study, the bacterial microflora in the nasal cavity of healthy dogs and their resistance to antimicrobials was determined. Identification of bacterial isolates was done using MALDI-TOF MS (matrix-assisted laser desorption/ionization time-of-flight mass spectrometer) and the results compared to 16S rRNA sequence analysis. A total of 203 isolates were recovered from the nasal passages of 63 dogs. The 203 isolates belonged to 58 bacterial species. The predominant genera were Streptococcus and Staphylococcus, followed by Corynebacterium, Rothia, and Carnobacterium. The species most commonly isolated were Streptococcus pluranimalium and Staphylococcus pseudointermedius, followed by Rothia nasimurium, Carnobacterium inhibens, and Staphylococcus epidermidis. Many of the other bacterial species were infrequently isolated from nasal passages, accounting for one or two dogs in the study. MALDI-TOF identified certain groups of bacteria, specifically non-spore-forming, catalase- positive, gram-positive cocci, but was less reliable in identifying non-spore-forming, catalase- negative, gram-positive rods. This study showed that MALDI-TOF can be used for identifying “clinically relevant” bacteria, but many times failed to identify less important species. -

Advancements in the Understanding of Staphylococcal
ADVANCEMENTS IN THE UNDERSTANDING OF STAPHYLOCOCCAL MASTITIS THROUGH THE USE OF MOLECULAR TOOLS __________________________________________ A Dissertation presented to the Faculty of the Graduate School at the University of Missouri-Columbia __________________________________________ In partial fulfillment of the requirements for the degree Doctor of Philosophy __________________________________________ By PAMELA RAE FRY ADKINS Dr. John Middleton, Dissertation Supervisor May 2017 The undersigned, appointed by the dean of the Graduate School, have examined the dissertation entitled ADVANCEMENTS IN THE UNDERSTANDING OF STAPHYLOCOCCAL MASTITIS THROUGH THE USE OF MOLECULAR TOOLS presented by Pamela R. F. Adkins, a candidate for the degree of Doctor of Philosophy, and hereby certify that, in their opinion, it is worthy of acceptance. Professor John R. Middleton Professor James N. Spain Professor Michael J. Calcutt Professor George C. Stewart Professor Thomas J. Reilly DEDICATION I dedicate this to my husband, Eric Adkins, and my mother, Denice Condon. I am forever grateful for their eternal love and support. ACKNOWLEDGEMENTS I thank John R. Middleton, committee chair, for this support and guidance. I sincerely appreciate his mentorship in the areas of research, scientific writing, and life in academia. I also thank all the other members of my committee, including Michael Calcutt, George Stewart, James Spain, and Thomas Reilly. I am grateful for their guidance and expertise, which has helped me through many aspects of this research. I thank Simon Dufour (University of Montreal), Larry Fox (Washington State University) and Suvi Taponen (University of Helsinki) for their contribution to this research. I acknowledge Julie Holle for her technical assistance, for always being willing to help, and for being so supportive. -
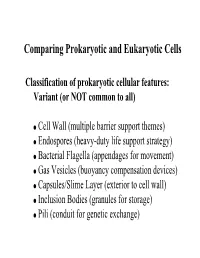
Comparing Prokaryotic and Eukaryotic Cells
Comparing Prokaryotic and Eukaryotic Cells Classification of prokaryotic cellular features: Variant (or NOT common to all) Cell Wall (multiple barrier support themes) Endospores (heavy-duty life support strategy) Bacterial Flagella (appendages for movement) Gas Vesicles (buoyancy compensation devices) Capsules/Slime Layer (exterior to cell wall) Inclusion Bodies (granules for storage) Pili (conduit for genetic exchange) Cell walls of Bacteria Cell envelope structure E. coli structure of peptidoglycan aka murein Peptidoglycan of a gram-positive bacterium Bond broken by penicillin DAP or Diaminopimelic acid Lysine Overall structure of peptidoglycan Cell walls of gram-positive and gram-negative bacteria Teichoic acids and the overall structure of the gram-positive cell wall Summary diagram of the gram-positive cell wall Cell envelopes of Bacteria Cell envelopes of Bacteria Structure of the lipopolysaccharide of gram-negative Bacteria The gram-negative cell wall N-Acetyltalosaminuronic acid Pseudopeptidoglycan of Archaea Paracrystalline S-layer: A protein jacket for Bacteria & Archaea Formation of the endospore Morphology of the bacterial endospore (a) Terminal (b) Subterminal (c) Central (a) Structure of Dipicolinic Acid & (b) crosslinked with Ca++ Bacterial flagella (a) Polar (aka monotrichous) & (b) Peritrichous Structure of the bacterial flagellum Flagellar Motility: Relationship of flagellar rotation to bacterial movement. Gas Vesicles (a) Anabaena flos-aquae (b) Microcystis sp. Hammer & Stopper Experiment (Before) (After) Model of how the two proteins that make up the gas vesicle, GvpA and GvpC, interact to form a watertight but gas-permeable structure. β-sheet α-helix Bacterial Capsules (a) Acinetobacter sp. (b) Rhizobium trifolii negative stain Storage of PHB Sulfur globules inside the purple sulfur bacterium Isochromatium buderi Magnetotactic bacteria with Fe3O4 (magnetite) particles called magnetosomes EM of Salmonella typhi “Sex” Pili used in bacterial conjugation of E. -

Détection Et Culture Des Archaea Associées Aux Muqueuses
AIX-MARSEILLE UNIVERSITE FACULTE DE MEDECINE DE MARSEILLE ECOLE DOCTORALE DES SCIENCES DE LA VIE ET DE LA SANTE THESE DE DOCTORAT Présentée par Saber KHELAIFIA En vue de l'obtention du grade de Docteur de l'Université Aix-Marseille Spécialité: Maladies Transmissibles et Pathologies Tropicales Détection et culture des archaea associées aux muqueuses intestinale et orale humaines Soutenue le 07 Juin 2013 COMPOSITION DU JURY Mr le Professeur Jean-Louis Mège Président du jury Mr le Docteur Bruno Franzetti Rapporteur Mr le Professeur Max Maurin Rapporteur Mr le Professeur Michel Drancourt Directeur de thèse Unité de Recherche sur les Maladies Infectieuses et Tropicales Emergentes, UMR CNRS6236 Prof – Didier Raoult 2013 Avant propos Le format de présentation de cette thèse correspond à une recommandation de la spécialité Maladies Infectieuses et Microbiologie du Master des Sciences de la Vie et de la Santé qui dépend de l’Ecole Doctorale des Sciences de la Vie de Marseille. Le candidat est amené à respecter des règles qui lui sont imposées et qui comportent un format de thèse utilisé dans le Nord de l’Europe et qui permet un meilleur rangement que les thèses traditionnelles. Par ailleurs, la partie introduction et bibliographie est remplacée par une revue publiée dans un journal scientifique afin de permettre une évaluation extérieure de la qualité de la revue et de permettre à l’étudiant de commencer le plus tôt possible une bibliographie exhaustive sur le domaine de cette thèse. Par ailleurs, la thèse est présentée sur article publié, accepté ou soumis associé d’un bref commentaire donnant le sens général du travail.