A Case of a 15-Month-Old with Periorbital Edema and Severe Anemia Audrey D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Research Training in the Biomedical, Behavioral and Clinical Sciences
RESEARCH TRAINING IN THE BIOMEDICAL, BEHAVIORAL, AND CLINICAL RESEARCH SCIENCES Committee to Study the National Needs for Biomedical, Behavioral, and Clinical Research Personnel Board on Higher Education and Workforce Policy and Global Affairs THE NATIONAL ACADEMIES PRESS 500 Fifth Street, N.W. Washington, DC 20001 NOTICE: The project that is the subject of this report was approved by the Governing Board of the National Research Council, whose members are drawn from the councils of the National Academy of Sciences, the National Academy of Engineering, and the Institute of Medicine. The members of the committee responsible for the report were chosen for their special competences and with regard for appropriate balance. This project was supported by Contract/Grant No. DHHS-5294, Task Order #187 between the National Acad- emy of Science and the National Institutes of Health, Department of Health and Human Services. Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the Committee to Study the National Needs for Biomedical, Behavioral, and Clinical Research Personnel and do not necessarily reflect the views of the organizations or agencies that provided support for the project. International Standard Book Number-13: 978-0-309-15965-4 (Book) International Standard Book Number-10: 0-309-15965-2 (Book) International Standard Book Number-13: 978-0-309-15966-1 (PDF) International Standard Book Number-10: 0-309-15966-0 (PDF) Library of Congress Control Number: 2011921184 Additional copies of this report are available from The National Academies Press, 500 Fifth Street, N.W., Lockbox 285, Washington, DC 20055; (800) 624-6242 or (202) 334-3313 (in the Washington metropolitan area); Internet, http://www.nap.edu. -

Evaluation of Iron Profile in Type II Diabetes Mellitus Cases
International Journal of Biotechnology and Biochemistry ISSN 0973-2691 Volume 15, Number 1 (2019) pp. 27-37 © Research India Publications http://www.ripublication.com Evaluation of Iron Profile in Type II Diabetes Mellitus Cases Dr. Sayantaann Saha*, Dr. Roopa Murgod Department of Biochemistry Vydehi Institute of Medical Sciences and Research Centre, EPIP Area, Whitefield, Bangalore 560066, India. ABSTRACT Introduction: Type 2 diabetes mellitus is the most common metabolic disorder, characterized by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Iron, a transitional metal has been shown to play a major role in pathogenesis of T2DM with a bi-directional relationship where iron affects glucose metabolism, and glucose metabolism in turn impinges on several iron metabolic pathways. Aims or Objectives: To estimate and compare the parameters related to iron metabolism viz. Serum Iron (Fe), Serum Ferritin, Serum TIBC (Total Iron Binding Capacity), Serum Transferrin and Transferrin Saturation with Fasting Blood Sugar (FBS) between T2DM patients and healthy controls and correlation of FBS with the above iron parameters. Material and methods: A case control study was conducted between 41 cases of confirmed T2DM patients and 40 age & sex matched healthy controls. Iron profile parameters & FBS were estimated in both the groups and compared. Iron parameters were also correlated with FBS. * Corresponding author(Dr. Sayantaann Saha), Email id: [email protected] 28 Dr. Sayantaann Saha, Dr. Roopa Murgod Results: Serum ferritin, Serum iron & serum transferrin saturation were found to be significantly higher in patients with T2DM compared to control group (P<0.001). Serum transferrin & serum TIBC were found to be slightly lower in cases as compared to controls (P<0.001). -

Genetically Determined Hypoalbuminemia As a Risk Factor for Hypertension: Instrumental Variable Analysis Jong Wook Choi1, Joon‑Sung Park2* & Chang Hwa Lee2*
www.nature.com/scientificreports OPEN Genetically determined hypoalbuminemia as a risk factor for hypertension: instrumental variable analysis Jong Wook Choi1, Joon‑Sung Park2* & Chang Hwa Lee2* Hypoalbuminemia is associated with vascular endothelial dysfunction and the development of chronic cardiovascular diseases. However, the relationship between serum albumin concentration and blood pressure changes remains controversial. Community‑based longitudinal cohort data collected from Korean Genome and Epidemiology Study were used in this study. Hypoalbuminemia was defned as a serum albumin concentration of ≤ 4.0 g/dL. A total of 4325 participants were categorized into control (n = 3157) and hypoalbuminemia (n = 1168) groups. Serum albumin had a non‑linear relationship with the risk of hypertension development. A genome‑wide association study revealed 71 susceptibility loci associated with hypoalbuminemia. Among susceptibility loci, genetic variations at rs2894536 in LOC107986598 and rs10972486 in ATP8B5P were related to elevated blood pressure. Serum albumin (HR = 0.654, 95% CI 0.521–0.820) and polymorphisms of rs2894536 (HR = 1.176, 95% CI 1.015–1.361) and rs10972486 (HR = 1.152, 95% CI 1.009–1.316) were signifcant predictors of hypertension development. Increased albumin concentration instrumented by 2 hypoalbuminemia‑associated SNPs (rs2894536 and rs10972486) was associated with decreased HRs for hypertension development (HR = 0.762, 95% CI 0.659–0.882 and HR = 0.759, 95% CI 0.656–0.878). Our study demonstrated that genetically determined hypoalbuminemia is a signifcant predictor of incipient hypertension. Albumin, one of the major serum proteins, has multiple important physiological functions involving stabilization of plasma colloid osmotic pressure, transportation of diverse substances, and signifcant antioxidant activity, and its concentration is fnely regulated by various systems in the physiologic state 1. -

Glycated Hemoglobin and Glycated Albumin in Patients with Diabetes
Kitajima et al. Renal Replacement Therapy (2020) 6:10 https://doi.org/10.1186/s41100-020-0260-5 RESEARCH Open Access Glycated hemoglobin and glycated albumin in patients with diabetes undergoing hemodiafiltration Yukie Kitajima1*, Shunichiro Urabe2, Takashi Hosono2, Satoshi Yoshikawa3, Yuzuru Sato3 and Toru Hyodo2 Abstract Background: Online hemodiafiltration (OHDF), which results in high albumin leakage, is now widely used in Japan for dialysis, since the national insurance system began reimbursing its costs in 2012. Glycated albumin (GA) levels are affected by albumin leakage into effluent dialysate fluid. Therefore, GA levels in patients requiring diabetes- related dialysis undergoing OHDF require monitoring. However, there have been no previous reports on glycemic control indicators of patients with diabetes undergoing OHDF. We aimed to develop a glycemic control index for patients requiring diabetes-related dialysis undergoing OHDF. Methods: This study comprised 133 diabetic patients undergoing OHDF. We examined the correlation between GA and glycated hemoglobin (HbA1c) levels. We analyzed effluent dialysate fluid samples from 41 patients classified into 3 groups, namely, group A, non-protein-leaking OHDF (n = 20); group B, protein-leaking OHDF (n = 14); and group C, highly efficient protein-leaking OHDF (n = 7). We examined the association between GA and HbA1c levels in each group and among patients. Results: A significant positive correlation was observed between GA and HbA1c levels (r = 0.562, p < 0.0001). There was no significant correlation between pre-dialysis blood glucose levels and HbA1c or GA levels as observed on regular blood tests performed under non-fasting conditions. Patients were classified into 2 groups based on their mean albumin levels (3.4 g/dL cutoff). -
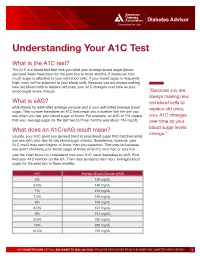
Understanding Your A1C Test
Diabetes Advisor Understanding Your A1C Test What is the A1C test? The A1C is a blood test that tells you what your average blood sugar (blood glucose) levels have been for the past two to three months. It measures how much sugar is attached to your red blood cells. If your blood sugar is frequently high, more will be attached to your blood cells. Because you are always making new red blood cells to replace old ones, your A1C changes over time as your blood sugar levels change. “Because you are always making new What is eAG? red blood cells to eAG stands for estimated average glucose and is your estimated average blood replace old ones, sugar. This number translates an A1C test result into a number like the one you see when you test your blood sugar at home. For example, an A1C of 7% means your A1C changes that your average sugar for the last two to three months was about 154 mg/dL. over time as your What does an A1C/eAG result mean? blood sugar levels change.” Usually, your A1C gives you general trend in your blood sugar that matches what you see with your day-to-day blood sugar checks. Sometimes, however, your A1C result may seem higher or lower than you expected. That may be because you aren’t checking your blood sugar at times when it’s very high or very low. Use the chart below to understand how your A1C result translates to eAG. First find your A1C number on the left. -

In Diagnosis Must Be Based on Clinical Signs and Symptoms. in This Paper
242 POST-GRADUATE MEDICAL JOURNAL August, 1938 Postgrad Med J: first published as 10.1136/pgmj.14.154.242 on 1 August 1938. Downloaded from SOME REMARKS ON DIFFERENTIAL DIAGNOSIS OF BLOOD DISEASES. By A. PINEY, M.D., M.R.C.P. (Assistant Physician, St. Mary's Hospital for Women and Children.) Differential diagnosis of blood diseases has been discussed time and again, but, as a rule, blood-pictures, rather than clinical features, have been taken into account, so that the impression has become widespread that the whole problem is one for the laboratory, rather than for the bed-side. It is obvious, however, that the first steps in diagnosis must be based on clinical signs and symptoms. In this paper, there- fore, certain outstanding clinical features of blood diseases, and various rather puzzling syndromes will be described. The outstanding external sign that leads the practitioner to consider the possi- bility of a blood disease is pallor, which is not quite so simple a state as is often supposed. It is, of course, well known that cutaneous pallor is not an infallible sign of anaemia, but it is often presumed that well-coloured mucous membranes are fairly good evidence that anaemia is not present. This is not necessarily true. The conjunctive may be bright pink in spite of anaemia, because mild inflammationProtected by copyright. may be present, masking the pallor. This is quite frequently due to irritation by eyelash dyes. Similarly, the finger-nails, which used to serve as a reliable index of pallor, are now found disguised with coloured varnish. -

Serological (Antibody) Testing for Covid-19
SEROLOGICAL (ANTIBODY) TESTING FOR COVID-19 Serological tests detect antibodies in the blood People in the early stages of COVID-19 might generated as part of the immune response test antibody negative despite being highly to a specific infection, such as infection with infectious. Additionally, some tests might give a SARS-CoV-2, the virus that causes COVID-19. false positive result because of past or present Antibody tests are different from tests such as infection with other types of coronaviruses. polymerase chain reaction (PCR) and antigen False positive results are also more likely tests which detect the SARS-CoV-2 virus. when the percentage of the population with Many new serological tests for COVID-19 have the disease is low. The Idaho Division of Public been developed and have an emergency use Health discourages persons who have a positive authorization (EUA) from the U.S. Food and serology test from relaxing the precautions such Drug Administration (FDA). Only antibody tests as social distancing that are recommended for that have an FDA EUA should be used. The all Idahoans to prevent spread of coronavirus, Idaho Division of Public Health discourages and strongly discourages employers form the use of unauthorized serology-based assays relaxing the employee protections for an for diagnosis of COVID-19 or determining if employee solely based upon a positive serology someone is currently infected or had a prior test. infection. The immune response to SARS-CoV-2 (the Serological tests are not recommended for virus that causes COVID-19) infection is not COVID-19 diagnosis in most situations because well understood. -

Section 8: Hematology CHAPTER 47: ANEMIA
Section 8: Hematology CHAPTER 47: ANEMIA Q.1. A 56-year-old man presents with symptoms of severe dyspnea on exertion and fatigue. His laboratory values are as follows: Hemoglobin 6.0 g/dL (normal: 12–15 g/dL) Hematocrit 18% (normal: 36%–46%) RBC count 2 million/L (normal: 4–5.2 million/L) Reticulocyte count 3% (normal: 0.5%–1.5%) Which of the following caused this man’s anemia? A. Decreased red cell production B. Increased red cell destruction C. Acute blood loss (hemorrhage) D. There is insufficient information to make a determination Answer: A. This man presents with anemia and an elevated reticulocyte count which seems to suggest a hemolytic process. His reticulocyte count, however, has not been corrected for the degree of anemia he displays. This can be done by calculating his corrected reticulocyte count ([3% × (18%/45%)] = 1.2%), which is less than 2 and thus suggestive of a hypoproliferative process (decreased red cell production). Q.2. A 25-year-old man with pancytopenia undergoes bone marrow aspiration and biopsy, which reveals profound hypocellularity and virtual absence of hematopoietic cells. Cytogenetic analysis of the bone marrow does not reveal any abnormalities. Despite red blood cell and platelet transfusions, his pancytopenia worsens. Histocompatibility testing of his only sister fails to reveal a match. What would be the most appropriate course of therapy? A. Antithymocyte globulin, cyclosporine, and prednisone B. Prednisone alone C. Supportive therapy with chronic blood and platelet transfusions only D. Methotrexate and prednisone E. Bone marrow transplant Answer: A. Although supportive care with transfusions is necessary for treating this patient with aplastic anemia, most cases are not self-limited. -

BPS White Paper
BOARD OF PHARMACY SPECIALTIES WHITE PAPER Five‐Year Vision for Pharmacy Specialties Approved by the BPS Board of Directors on January 12, 2013 © Copyright 2013, Board of Pharmacy Specialties Introduction The Joint Commission of Pharmacy Practitioners’ (JCPP) Future Vision of Pharmacy Practice 2015 states, “Pharmacists will be the healthcare professionals responsible for providing patient care that ensures optimal medication therapy outcomes.” i As the scope of pharmacy practice evolves to meet the complex medication‐related needs of patients, board certification is critical to assure stakeholders of the level of knowledge and skills of pharmacists who provide direct patient care. The Board of Pharmacy Specialties (BPS) acknowledges the support and collaboration of many national pharmacy organizations in this pursuit and assumes the responsibility for recognition of pharmacy specialization through board certification.ii,iii, iv In assuming this responsibility, BPS also acknowledges the pharmacist’s role in direct patient care as it continues to evolve against a backdrop of many unknowns such as changing health care delivery systems and payment models in which the role of government and the private sector are in a state of flux. Whatever changes come to fruition in the delivery of health care, BPS must move forward in a flexible manner that meets its mission to improve patient care by promoting the recognition and value of specialized training, knowledge, and skills in pharmacy and specialty board certification of pharmacists. v This white paper adds focus and clarity to how BPS will approach the board certification of pharmacist specialists over the next five years. This timeline is critical as the goal will be to create a scalable foundation on which to build future board certification activities for pharmacists. -
![PHYSICIAN-SCIENTIST [MD/PHD] Who Better to Study Disease Than Those Who Know It Intimately? WHAT IS a PHYSICIAN SCIENTIST?](https://docslib.b-cdn.net/cover/7441/physician-scientist-md-phd-who-better-to-study-disease-than-those-who-know-it-intimately-what-is-a-physician-scientist-217441.webp)
PHYSICIAN-SCIENTIST [MD/PHD] Who Better to Study Disease Than Those Who Know It Intimately? WHAT IS a PHYSICIAN SCIENTIST?
PHYSICIAN-SCIENTIST [MD/PHD] Who better to study disease than those who know it intimately? WHAT IS A PHYSICIAN SCIENTIST? A physician scientist is a unique clinician who is part of a small cadre of physicians who usually work in academic health science centers and have a high impact on health care through discovery, translational and clinical research, and clinical practice. A physician scientist in Pathology and Laboratory Medicine is a laboratory physician who is trained in both scientific biomedical investigation and in pathology and/or laboratory medicine, often with clinical subspecialty training. On one hand, the physician scientist brings the rigors of scientific investigation into the patient care arena and on the other, the physician scientist’s contact with disease brings clinically relevant questions into the research arena to drive investigations into pathogenesis, prevention, diagnosis, prognosis, and treatment of disease. asip.org/CareerPath/ MEET ADEL MAHMOUD, MD, PHD P HYSICIAN . SCIENTIST. PROFESSOR . MENTOR . Princeton University Lecturer with rank of Professor in Molecular Biology and Public Policy, Woodrow Wilson School MD from the University of Cairo in 1963 PhD from the University of London, School of Hygiene and Tropical Medicine in 1971 Elected to membership of the American Society for Clinical Investigation in 1978, the Association of American Physicians in 1980 and the Institute of Medicine of the National Academy of Sciences in 1987. Received the Bailey K. Ashford Award of the A merican Society of Tropical Medicine and Hygiene in 1983, and the Squibb Award of the Infectious Diseases Society of America in 1984 . F e l l o w of the American College of Physicians and a member of the Expert Advisory Panel on Parasitic Diseases of the World Health Organization. -

Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: a Retrospective Case Series (1999–2018) †
animals Article Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: A Retrospective Case Series (1999–2018) † Maria Alfonsa Cavalera 1, Floriana Gernone 1, Annamaria Uva 1, Paola D’Ippolito 2, Xavier Roura 3 and Andrea Zatelli 1,* 1 Department of Veterinary Medicine, University of Bari, 70010 Valenzano, Italy; [email protected] (M.A.C.); fl[email protected] (F.G.); [email protected] (A.U.) 2 Veterinary diagnostic Lab ACV Triggiano, 70019 Triggiano, Italy; [email protected] 3 Hospital Clínic Veterinari, Universitat Autònoma de Barcelona, 08193 Bellaterra, Spain; [email protected] * Correspondence: [email protected]; Tel.: +39-080-4679804 † This study was partially presented as oral communication at the 11th ECVIM-CA/ESVIM Congress, Dublin (Ireland) as “Congenital nephrotic syndrome with renal glomerular immaturity in 7 Boxer dogs”. Zatelli, A., Domenech, O., Bussadori, C., Lubas, G., Del Piero, F. Simple Summary: This study describes clinical findings in Boxer dogs with renal maldevelopment and proposes a possible mode of inheritance. Medical records of 9 female Boxer dogs, older than 5 months and with a clinical diagnosis of proteinuric chronic kidney disease prior to one year of age, showed the presence of polyuria and polydipsia, decreased appetite, weight loss, lethargy and weakness in all affected dogs. Common laboratory findings were proteinuria and diluted urine, non- regenerative anemia, azotemia, hyperphosphatemia, hypoalbuminemia and hypercholesterolemia. Citation: Cavalera, M.A.; Gernone, Histopathology of the kidneys identified the presence of immature glomeruli in all dogs. In 7 out F.; Uva, A.; D’Ippolito, P.; Roura, X.; of 9 related dogs, the pedigree analysis showed that a simple autosomal recessive trait may be a Zatelli, A. -

Emerging and Dynamic Biomedical Uses of Ferritin
pharmaceuticals Review Emerging and Dynamic Biomedical Uses of Ferritin Brian Chiou and James R. Connor * Department of Neurosurgery, Penn State College of Medicine, Hershey, PA 17033, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-717-531-4541 Received: 24 October 2018; Accepted: 12 November 2018; Published: 13 November 2018 Abstract: Ferritin, a ubiquitously expressed protein, has classically been considered the main iron cellular storage molecule in the body. Owing to the ferroxidase activity of the H-subunit and the nucleation ability of the L-subunit, ferritin can store a large amount of iron within its mineral core. However, recent evidence has demonstrated a range of abilities of ferritin that extends well beyond the scope of iron storage. This review aims to discuss novel functions and biomedical uses of ferritin in the processes of iron delivery, delivery of biologics such as chemotherapies and contrast agents, and the utility of ferritin as a biomarker in a number of neurological diseases. Keywords: ferritin; iron; iron delivery; nanotechnology; nanocage; drug delivery; inflammation; serum biomarker 1. Ferritin Introduction Ferritin, a protein originally identified in 1937 by Vilém Laufberger [1], is a ubiquitously expressed iron storage protein most commonly characterized by its ability to accumulate and store up to 4500 atoms of iron [2]. Ferritin consists of 24 subunits, typically comprised of different ratios of the H and L chain subunit. The ratios vary by organ and even by cell type. Importantly, the different subunits have divergent functions—H-ferritin utilizes ferroxidase activity that is necessary for the oxidation of ferrous (Fe2+) to ferric (Fe3+) iron while L-ferritin contains acidic residues on the surface cavity of the protein that facilitate ferroxidase turnover and are crucial for the nucleation of ferric iron within the core of the fully formed protein.