Thiolated Polymers: Bioinspired Polymers Utilizing One of the Most Important Bridging Structures in Nature
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thioglycolic Acid (TGA) by Arkema
Thioglycolic Acid (tga) TGA – a leading corrosion inhibitor and iron controller for the oil and gas industry. Thioglycolic acid (TGA or mercaptoacetic acid, TGA IN CORROSION CAS 68-11-1) is a high-performance chemical INHIBITION FORMULATIONS containing mercaptan and carboxylic acid Water is present in most crude oil and gas functionalities. TGA is completely miscible in production and is the cause of problems in the water and is used in industries and applications recovery and transportation of oil and gas. as diverse as oil and gas, cosmetics, Water can come either from the formation cleaning, leather processing, metals, itself or from the water flooding used in the fine chemistry and polymerization. secondary recovery operations. Thioglycolic acid forms powerful complexes Corrosion is mainly due to the presence of with metals that give it specific characteristics water with CO and/or H2S. sought after for the assisted recovery of ore as well as for cleaning and corrosion inhibition. Corrosion inhibitors could be added to form a film which protects the metal from iron corrosion. Corrosion inhibitors are injected TGA FOR OIL AND GAS either continuously into the fluid stream or into PRODUCTION a producing well. They can be added in the Specialty chemicals are now taking on an water flooding operations of secondary oil important role in the enhancement of oil recovery, as well as pipelines, transmission recovery and production at different stages: lines and refinery units. Although the corrosion inhibition is a complex process, highly Well Drilling dependent of various parameters such as the Drilling fluids are used to lubricate the drill bit, nature of the inhibitor, fluid composition, pH, control the formation pressure, and remove temperature, etc., the mechanism generally formation cuttings. -

Rapid Modular Synthesis and Processing of Thiol−Ene Functionalized Styrene−Butadiene Block Copolymers Joshua S
Article pubs.acs.org/Macromolecules Rapid Modular Synthesis and Processing of Thiol−Ene Functionalized Styrene−Butadiene Block Copolymers Joshua S. Silverstein,†,‡ Brendan J. Casey,‡ Mary E. Natoli,† Benita J. Dair,‡ and Peter Kofinas*,† † Fischell Department of Bioengineering, University of Maryland, College Park, Maryland 20742, United States ‡ Center for Devices and Radiological Health, Office of Science and Engineering Laboratories, Division of Chemistry and Materials Science, Food and Drug Administration, Silver Spring, Maryland 20993, United States *S Supporting Information ABSTRACT: Diblock and triblock copolymers of poly- (styrene)-block-poly(1,2-butadiene) (PS/PB) and PS/PB/PS were modified by photochemical thiol−ene chemistry to pro- cess selected functional nanopatterned polymers, with reaction completion in 1 h. PB molecular weight (MW) and thiol−ene ratios were systematically varied based on a model monomer, boc-cysteamine, to determine the efficiency of the reaction. The results demonstrate the polydispersity index (PDI) of modified block copolymers significantly increased when low thiol−ene ratios were employed and sometimes induced gelation of the reacted polymers. Using a 10-fold excess of thiol, functionalizations between 60% and 90% were obtained for amines, carboxylic acids, amides, and a pharmaceutical with a pendant thiol. Differential scanning calorimetry showed a 30−60 °C increase in the glass transition temperature of the daughter polymers. Subsequently, these polymers were spin-coated from solvents found suitable to form self-assembled block copolymer films. The microstructure domain spacing for each polymer was consistent with those originating from the parent polymer. This technique described allows for the formation of nanopatterned block copolymer films with controlled chemistries from a single source material. -

I REGENERATIVE MEDICINE APPROACHES to SPINAL CORD
REGENERATIVE MEDICINE APPROACHES TO SPINAL CORD INJURY A Dissertation Presented to The Graduate Faculty of The University of Akron In Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy Ashley Elizabeth Mohrman March 2017 i ABSTRACT Hundreds of thousands of people suffer from spinal cord injuries in the U.S.A. alone, with very few patients ever experiencing complete recovery. Complexity of the tissue and inflammatory response contribute to this lack of recovery, as the proper function of the central nervous system relies on its highly specific structural and spatial organization. The overall goal of this dissertation project is to study the central nervous system in the healthy and injured state so as to devise appropriate strategies to recover tissue homeostasis, and ultimately function, from an injured state. A specific spinal cord injury model, syringomyelia, was studied; this condition presents as a fluid filled cyst within the spinal cord. Molecular evaluation at three and six weeks post-injury revealed a large inflammatory response including leukocyte invasion, losses in neuronal transmission and signaling, and upregulation in important osmoregulators. These included osmotic stress regulating metabolites betaine and taurine, as well as the betaine/GABA transporter (BGT-1), potassium chloride transporter (KCC4), and water transporter aquaporin 1 (AQP1). To study cellular behavior in native tissue, adult neural stem cells from the subventricular niche were differentiated in vitro. These cells were tested under various culture conditions for cell phenotype preferences. A mostly pure (>80%) population of neural stem cells could be specified using soft, hydrogel substrates with a laminin coating and interferon-γ supplementation. -

Thioglycolic Acid
Thioglycolic acid sc-251234 Material Safety Data Sheet Hazard Alert Code EXTREME HIGH MODERATE LOW Key: Section 1 - CHEMICAL PRODUCT AND COMPANY IDENTIFICATION PRODUCT NAME Thioglycolic acid STATEMENT OF HAZARDOUS NATURE CONSIDERED A HAZARDOUS SUBSTANCE ACCORDING TO OSHA 29 CFR 1910.1200. NFPA FLAMMABILITY1 HEALTH4 HAZARD INSTABILITY2 SUPPLIER Company: Santa Cruz Biotechnology, Inc. Address: 2145 Delaware Ave Santa Cruz, CA 95060 Telephone: 800.457.3801 or 831.457.3800 Emergency Tel: CHEMWATCH: From within the US and Canada: 877-715-9305 Emergency Tel: From outside the US and Canada: +800 2436 2255 (1-800-CHEMCALL) or call +613 9573 3112 PRODUCT USE Used as a sensitive reagent for iron, molybdenum, silver, tin. Used in the manufacture of thioglycolates. The ammonium and sodium salts are commonly used for cold waving and the calcium salt is a depilatory. Used in the manufacture of pharmaceuticals. SYNONYMS C2-H4-O2-S, HSCH2COOH, "2-thioglycolic acid", "2-thioglycolic acid", mercaptoacetate, "alpha-mercaptoacetic acid", "2- mercaptoacetic acid", "2-mercaptoacetic acid", "thioglycollic acid", "thiovanic acid", "glycolic acid, thio-", "glycolic acid, 2-thio-", "glycolic acid, 2-thio-" Section 2 - HAZARDS IDENTIFICATION CANADIAN WHMIS SYMBOLS EMERGENCY OVERVIEW RISK Contact with acids liberates very toxic gas. Causes burns. Risk of serious damage to eyes. Toxic by inhalation, in contact with skin and if swallowed. POTENTIAL HEALTH EFFECTS ACUTE HEALTH EFFECTS SWALLOWED ■ The material can produce chemical burns within the oral cavity and gastrointestinal tract following ingestion. ■ Toxic effects may result from the accidental ingestion of the material; animal experiments indicate that ingestion of less than 40 gram may be fatal or may produce serious damage to the health of the individual. -

Kosmetischer Stift Auf Basis Einer Öl-In-Wasser-Dispersion/Emulsion
*DE102008028822A120090219* (19) (10) Bundesrepublik Deutschland DE 10 2008 028 822 A1 2009.02.19 Deutsches Patent- und Markenamt (12) Offenlegungsschrift (21) Aktenzeichen: 10 2008 028 822.5 (51) Int Cl.8: A61K 8/92 (2006.01) (22) Anmeldetag: 19.06.2008 A61Q 19/00 (2006.01) (43) Offenlegungstag: 19.02.2009 A61Q 17/04 (2006.01) A61Q 15/00 (2006.01) (66) Innere Priorität: (72) Erfinder: 10 2007 028 819.2 20.06.2007 Banowski, Bernhard, 40597 Düsseldorf, DE; Claas, Marcus, 40723 Hilden, DE; Buse, Nadine, (71) Anmelder: 40721 Hilden, DE Henkel AG & Co. KGaA, 40589 Düsseldorf, DE Die folgenden Angaben sind den vom Anmelder eingereichten Unterlagen entnommen (54) Bezeichnung: Kosmetischer Stift auf Basis einer Öl-in-Wasser-Dispersion/Emulsion mit einem Hydrogelbildner (57) Zusammenfassung: Die Anmeldung betrifft kosmeti- sche Stifte auf Basis einer Öl-in-Wasser-Dispersion/Emul- sion zur Applikation auf die Haut. 1/79 DE 10 2008 028 822 A1 2009.02.19 Beschreibung [0001] Die Erfindung betrifft kosmetische Stifte auf Basis einer Öl-in-Wasser-Dispersion/Emulsion mit einem Hydrogelbildner zur Applikation kosmetischer Wirkstoffe auf die Haut. [0002] Handelsübliche kosmetische Zusammensetzungen werden meistens als Cremes oder Lotionen kon- fektioniert, die einem Tiegel, einer Tube, einer Flasche oder einem Pumpspender entnommen werden; dane- ben gibt es Roll-on-Präparate, Sprays und (Kompakt-)Puder im Markt. Bei den Verbrauchern erfreuen sich Stiftpräparate zur Anwendung sowohl dekorativer als auch pflegender Kosmetik hoher Beliebtheit. Sie sind handlich, transportstabil und bequem aufzutragen. Zunehmend besteht bei den Konsumenten das Bedürfnis nach Zusammensetzungen, die neben der Basisfunktion, also z. B. dem Abdecken von Hautunreinheiten oder dem Mattieren fettglänzender Haut, noch weitere Pflege- und Behandlungseffekte, z. -

Publications About Thiomers
Publications about Thiomers: Reviews: Akhtar, N., Ahad, A., Khar, R.K., Jaggi, M., Aqil, M., Iqbal, Z., Ahmad, F.J., Talegaonkar, S. (2011) The emerging role of P - glycoprotein inhibitors in d rug delivery: a patent review . Expert Opin. Ther. Pat . 21 , 561 - 576. Albrecht, K., Bernkop - Schnürch, A. (2007) Thiomers: forms, functions and applications to nanomedicine. Nanomedicine (Lond). 2 , 41 - 50. Bernkop - Schnürch, A., Hoffer, M.H., Kafedjiiski, K. (2004) Thiomers for oral delivery of hydrophilic macromolecular drugs. Expert Opin. Drug Deliv . 1 , 87 - 98. Bernkop - Schnürch A. (2005) Thiomers: a new generation of mucoadhesive polymers . Adv. Drug Deliv. Rev . , 57 , 1569 - 1582. Bernkop - Schnürch, A., Krauland, A.H., Leitner, V.M., Palmberger, T. (2004) Thiomers: potential excipients for non - invasive peptide delivery systems. Eur. J. Pharm. Biopharm ., 58 , 253 - 63. Bernkop - Schnürch, A., Hornof, M., Guggi, D. (2004) Thiolated chitosans. Eur. J. Pharm. Biopharm . 57 , 9 - 17. B ernkop - Schnürch, A., Kast, C.E., Guggi D. (2003) Permeation enhancing polymers in oral delivery of hydrophilic macromolecules: thiomer/GSH systems. J. Control Release , 93 , 95 - 103. Bonengel, S., Bernkop - Schnürch, A. (2014 ) Thiomers -- from bench to market. J. Control. Release , 195 , 120 - 129. Cano - Cebrián, M.J., Zornoza, T., Granero, L., Polache, A. (2005) Intestinal absorption enhancement via the paracellular route by fatty acids, chitosans and others: a target for drug delivery. Curr. Drug Deliv ., 2 , 9 - 22. Chaudhury, A., Das, S. (2011) Recent advancement of chitosan - based nanoparticles for oral controlled delivery of insulin and other therapeutic agents. AAPS PharmSciTech ., 12 , 10 - 20. Chen, M.C., Mi, F.L., Liao, Z.X., Hsiao, C.W., Sonaje, K., Chung, M.F., Hsu, L.W., Sun g, H.W. -

United States Patent (19) 11, 3,927,085 Zengel Et Al
United States Patent (19) 11, 3,927,085 Zengel et al. (45) Dec. 16, 1975 54 PROCESS FOR THE PRODUCTION OF A 3,029,279 4/1962 Kondo............................. 26O1526 S MERCAPTOCARBOXYLIC ACID 3,502,708 3/1970 Thoma et al.................... 260/526 S 3,517,058 6/1970 Thoma et al.................... 26O1526 S 75 Inventors: Hans-Georg Zengel, Kleinwallstadt; 3,551,499 l2/1970 Krockow ......................... 260/526 S Anton Toth, Obernburg; Helmut Magerlein, Obernburg; Gerhard Primary Examiner-Vivian Garner Meyer, Obernburg, all of Germany Attorney, Agent, or Firm-Johnston, Keil, Thompson 73 Assignee: Akzo N. V., Arnhem, Netherlands & Shurtleff 22 Filed: Oct. 15, 1974 57 ABSTRACT 21 Appl. No.: 514,463 A process for the production of mercaptoacetic acid and g-mercaptopropionic acid by reacting hydrogen 30 Foreign Application Priority Data sulfide at a partial pressure above 2 atm., preferably 8 Oct. 29, 1973 Germany............................ 2354O98 to 22 atm. and at a temperature of about 60°C. to 140°C., preferably 80°C. to 105°C., in admixture with 52 U.S. Cl........ 260/526 S; 260/.535 R; 260/537 P a chlorocarboxylic acid compound of the formula 51 Int. Cl’........................................ C07C 148/00 C-(CH2) -COOM, wherein n is the integer 1 or 2 58 Field of Search.................................. 260/526 S and M is hydrogen, ammonium or sodium or mixtures thereof in the presence of aqueous sodium or ammo 56 References Cited nium hydroxide and the initial reaction mixture has a concentration of the chlorocarboxylic acid compound UNITED STATES PATENTS in water of about 4.0 to 12 mol percent, preferably 6.0 2,449,989 9/1948 Gresham......................... -
Bbm:978-3-642-64958-5/1.Pdf
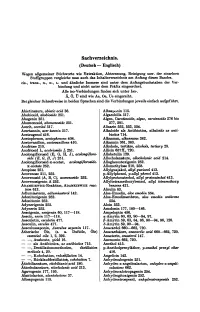
Sachverzeichnis. (Deutsch - Englisch) Wegen allgemeiner Stichworte wie Extraktion, Abtrennung, Reinigung usw. der einzelnen Stoffgruppen vergleiche man auch das Inhaltsverzeichnis am Anfang dieses Bandes. cis-, t.rans-, no, D-, L- und ahnliche lsomere sind unter dem Anfangsbuchst&ben der Ver bindung ~nd nicht unter dem Prafix eingeordnet. AIle iso-Verbindungen finden sich unter lso-. A, 0, tJ sind wie Ae, Oe, Ue eingereiht. Bei gleicher Schreibweise in beiden Sprachen sind die Verbindungen jeweils einfach aufgefiihrt. Abietinsaure, abietic acid 36. Albsa}Nnin 115. Abobiosid, abobioside 251. Algarobilla 517. Abogenin 251. Algen, Carotinoide, algae, carotenoid8 276 bis Abomonosid, abmnono8ide 251. 277,281. Acerit, aceritol 517. Alizarin 552, 553, 554. Acertannin, acer·tannin 517. Alkaloide als Antibiotica, alkaloid8 as anti- Aceteugenol416. biotics 714. Acetophenon, acetopheTUYlle 408. Alkannan, alkannane 382. Acetovanillon, acetovanillone 410. Alkannin 361,383. Acofriose 210. Alkohole, tertiare, alcohols, tertiary 29. Acofriosid L, acolrioside L 251. Allicin 657ft'., 720. Acolongiflorosid (E, G, H, J), acolongilloro- Allobetulin 129. Bide (E, a, H, J) 251. Allocholansaure, aUockolanic acid 214. Acolongiflorosid-K-acetat, acolongilloroside- Alloglaucotoxigenin 252. K-acetate 252. Allomethylose 210, 258. Acopiose 251. AIlylguajakol, allyl guaiacol 413. Acovenose 211, 252. p-Allylphenol, p-allyl phenol 413. Acovenosid (A, B, C); acoven08ide 252. Allylprotocatechol, aUyl protocatechol 413. Acovenosigenin A 252. Allyltetramethoxybenzol, aUyl tetramethoxy ADAMKIEwIcz-Reaktion, ADAMKIEWICZ reac- bemene 421. tion 613. Alnulin 83. Adlumiasterin, adlumiasterol 142. Aloe-Emodin, aloe emodin 554. Adonitoxigenin 252. Aloe-Emodinanthron, aloe emodin anthrone Adonitoxin 252. 554. Adynerigenin 252. Aloin 553.· Adynerin 252. Amolonin 177, 185-186. Aescigenin, Il8cigenin 60, 117-118. Ampeloptin 456. Aescin, Il8cin 117-118. I1-Amyrin 60, 63, 90-94, 97. -

Organic Seminar Abstracts
UNIVERSITY OF IILINOIS LIBRARY AT U ^.NA-CHAMPAIGN Digitized by the Internet Archive in 2012 with funding from University of Illinois Urbana-Champaign http://archive.org/details/organicsemi1979821univ 1 SEMINAR TOPICS X- I Semester 1979-80 — ^ Generation and Synthetic Utility of Carbanions Stabilized by Divalent Sulfur Peter Becker The Design, Synthesis, and Biology of Intercalating Agents David W. Robertson r HERTZBERG - NEW METHOD, INC. EAST VANDALIA ROAD, JACKSONVILLE, ILL. 62650 J - Q_ , TITUE NO. ACCOUNT NO. LOT AND TICKET NO. ...13 B ]• 22 : NRTK« 31 5>79~82*PT Q* 547*IG»L< 33 CLOTH COLOR CHARGING INFORMATION .... 36 STUBBING FRONT COVER HAND SEW NO TR IM THRU SEW PAGES LAMINATED THRU SEW ON TAPE EXTRA THICKNESS ... .46 HAND ADHESIVE MAP POCKET PAPER LENGTHWISE MAP POCKET CLOTH SPECIAL WORK AND PREP. FOREIGN TITLE SPECIAL WORK LINES OF LETTERING 56 Phosphorus uompouiiub Stephen D. Harper Vanadium- and Molybdenum-Catalyzed of Olefins with Epoxidations 59 Alkyl Hydroperoxides - John R. Hurst Characterization of Certain Detection and 68 Carbon Diradicals Via ESR and CIDNP... G. H. Slocum 76 Enzymic Catalysis in Organic Synthesis Venkatesalu Bakthavachalam in the Reactions of Regioselectivity 86 Hetero-Substituted Allylic Carbanions, Dale Kempf SEMINAR TOPICS I Semester 1979-80 - T* Generation and Synthetic Utility of Carbanions Stabilized by Divalent Sulfur 1 Peter Becker The Design, Synthesis, and Biology of Intercalating Agents 3 David W. Robertson Modification of Olefins with Organo- Selenium Reagents 13 Larry D. Boardman Synthetic Methods for the Preparation of Sterically Hindered Olefins 22 Ronald S. Michalak Mechanistic Considerations in 1,3-Dipolar Cycloadditions 31 Clark Cummins Applications of Lasers in Organic Chemistry 33 Rick Gdanski Magnetic Field Effects on Chemical Reactions in Solution 36 Paul Gelburd Synthetic Approaches to Biotin 46 Jack Muskopf Stable Hexacoordinate Organo- Phosphorus Compounds 56 Stephen D. -

ABSTRACT WILLIAMS, TOVA N. Approaches
ABSTRACT WILLIAMS, TOVA N. Approaches to the Design of Sustainable Permanent Hair Dyes (Under the direction of Harold S. Freeman). Interest in designing sustainable permanent hair dyes derives from the toxicological concerns associated with certain commercial dyes, in particular the moderate to strong/extreme skin sensitization potential of certain precursors used to develop the dyes. While work has been undertaken to help address toxicological concerns of hair dyes, alternatives having commercial success are based on the conventional permanent hair dye coloration process and still may pose health problems. The conventional process involves the oxidation of small and essentially colorless precursors (e.g., p-phenylenediamine and resorcinol) within the hair fiber that couple to build oligomeric indo dyes that are difficult to desorb. The resultant depth of shade achieved is superior that of other hair dyes and provides a high degree of gray coverage. In fact, these dyes dominate the commercial realm and stimulate the multibillion-dollar global hair dye market for the millions of consumers (men and women) who use them. Approaches to the design of sustainable (less toxic) permanent hair dyes lie at the heart of the present study. In Part 1 of this study, two types of keratin films (opaque and translucent) were characterized for their potential as screening tools for predicting the efficacy of potential hair dyes using the hair dye, C.I. Acid Orange 7. Translucent keratin films, which were found to be less porous than opaque films and more like hair in this regard, were deemed better tools for predicting the efficacy of potential hair dyes on hair. -

Dissertation Assessment of Water Quality, Toxicity and Treatment Strategies Downstream of Npdes Oil and Gas Produced Water Disch
DISSERTATION ASSESSMENT OF WATER QUALITY, TOXICITY AND TREATMENT STRATEGIES DOWNSTREAM OF NPDES OIL AND GAS PRODUCED WATER DISCHARGES INTENDED FOR BENEFICIAL REUSE Submitted by Molly Cook McLaughlin Department of Civil and Environmental Engineering In partial fulfillment of the requirements For the Degree of Doctor of Philosophy Colorado State University Fort Collins, Colorado Fall 2019 Doctoral Committee: Advisor: Thomas Borch Co-Advisor: Jens Blotevogel Juan Lucas Argueso Paula Mouser Tom Sale Copyright by Molly Cook McLaughlin 2019 All Rights Reserved ABSTRACT ASSESSMENT OF WATER QUALITY, TOXICITY AND TREATMENT STRATEGIES DOWNSTREAM OF NPDES OIL AND GAS PRODUCED WATER DISCHARGES INTENDED FOR BENEFICIAL REUSE Produced water is the largest waste stream associated with oil and gas operations. This complex fluid contains petroleum hydrocarbons, heavy metals, salts, naturally occurring radioactive materials (NORMs) and any remaining chemical additives. In the United States, west of the 98th meridian, the federal National Pollutant Discharge Elimination System (NPDES) exemption allows release of produced water for agricultural beneficial reuse if it is of “good enough quality.” Due to the complex and variable composition of produced water as well as the variations in permit effluent limits and treatment approaches, the downstream impacts of NPDES produced water releases are not fully understood. The goal of this dissertation was to determine if the current NPDES produced water permit effluent limits are adequate and if not, to identify additional steps that can be taken to improve water quality. As a first step towards this goal, a detailed chemical and toxicological analysis was conducted on a stream composed of produced water released for agricultural beneficial reuse. -

Nomination Background: Sodium Thioglycolate (CASRN: 367-51-1)
SUMMARY OF DATA FOR CHEMICAL SELECTION THIOGLYCOLIC ACID, SALTS AND ESTERS 68-11-1, 367-51-1, 814-71-1, 5421-46-5, 30618-84-9 BASIS OF NOMINATION TO THE CSWG The nomination of thioglycolic acid to the CSWG is based on very high production volume, extensive exposure potential, and lack of information on potential carcinogenicity. Dr. Elizabeth Weisburger, a member of the American Conference of Governmental Industrial Hygienists (ACGIH) TLV Committee as well as the Chemical Selection Working Group (CSWG), provided a list of 281 chemical substances with ACGIH recommended TLVs for which there were no long-term studies cited in the supporting data and no designations with respect to carcinogenicity. She presented the list to the Chemical Selection Planning Group (CSPG) for evaluation as chemicals which may warrant chronic testing; it was affirmed at the CSPG meeting held on August 9, 1994, that the 281 "TLV Chemicals" be reviewed as a Class Study. As a result of the class study review, thioglycolic acid is presented as a candidate for testing by the National Toxicology Program because of: • potential for broad consumer exposures based on cosmetic use • potential for occupational exposures based on high production volume • evidence of occupational exposures based on TLV and other literature documentation • lack of chronic toxicity data. Sources of human exposure to thioglycolic acid are both occupational and general (consumer); and the exposure potential is considered high based on cosmetic use and an estimated U.S. annual production volume range of 2.6 to 11.5 million pounds for thioglycolic acid, an estimate of 30,055 worker exposures (15,142 female) reported in the NOES database for thioglycolic acid, 41,132 worker exposures (30,869 female) for ammonium thioglycolate, and 7,553 worker exposures (6,204 female) for sodium thioglycolate.