Component of Osteosarcopenia on Fragility Fractures in Post-Menopausal Women
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Hmong Culture: Kinship, Marriage & Family Systems
THE HMONG CULTURE: KINSHIP, MARRIAGE & FAMILY SYSTEMS By Teng Moua A Research Paper Submitted in Partial Fulfillment of the Requirements for the Master of Science Degree With a Major in Marriage and Family Therapy Approved: 2 Semester Credits _________________________ Thesis Advisor The Graduate College University of Wisconsin-Stout May 2003 i The Graduate College University of Wisconsin-Stout Menomonie, Wisconsin 54751 ABSTRACT Moua__________________________Teng_____________________(NONE)________ (Writer) (Last Name) (First) (Initial) The Hmong Culture: Kinship, Marriage & Family Systems_____________________ (Title) Marriage & Family Therapy Dr. Charles Barnard May, 2003___51____ (Graduate Major) (Research Advisor) (Month/Year) (No. of Pages) American Psychological Association (APA) Publication Manual_________________ (Name of Style Manual Used In This Study) The purpose of this study is to describe the traditional Hmong kinship, marriage and family systems in the format of narrative from the writer’s experiences, a thorough review of the existing literature written about the Hmong culture in these three (3) categories, and two structural interviews of two Hmong families in the United States. This study only gives a general overview of the traditional Hmong kinship, marriage and family systems as they exist for the Hmong people in the United States currently. Therefore, it will not cover all the details and variations regarding the traditional Hmong kinship, marriage and family which still guide Hmong people around the world. Also, it will not cover the ii whole life course transitions such as childhood, adolescence, adulthood, late adulthood or the aging process or life core issues. This study is divided into two major parts: a review of literature and two interviews of the two selected Hmong families (one traditional & one contemporary) in the Minneapolis-St. -

A Re-Evaluation of Pelliot Tibétain 1257: an Early Tibet- An-Chinese Glossary from Dunhuang1
A Re-evaluation of Pelliot tibétain 1257: An Early Tibet- an-Chinese Glossary from Dunhuang1 James B. Apple and Shinobu A. Apple Introduction elliot tibétain 1257 (hereafter, PT1257) is an early manuscript preserved from the ancient city-state of Dunhuang kept P among the materials of the Paul Pelliot collection conserved at the Bibliothéque Nationale de France in Paris, France. Digital images of the manuscript are found at the web site of Gallica Digital Library (http://gallica.bnf.fr) and the International Dunhuang Project (http:// idp.bl.uk/; hereafter, IDP). French scholars Marcelle Lalou (1939) and R.A. Stein (1983 [English translation 2010]) have previously dis- cussed in an abbreviated manner the content and characteristics of this manuscript. A more extensive discussion of PT1257 is found among Japanese Buddhologists and specialists in Dunhuang studies. Akira Fujieda (1966), Zuihō Yamaguchi (1975), and Noriaki Haka- maya (1984) have provided initial insights into the structure and con- tent of PT1257 while the work of Ryūtoku Kimura (1985) and Kōsho Akamatsu (1988) have furnished more detailed points of analysis that have contributed to our current understanding of this manu- script. Other scholarship related to PT1257 has suggested that the manuscript was from a Chinese monastery and that it was utilized to help Chinese scholars translate Tibetan. This paper re-evaluates this presumption based upon a close analysis of the material components of the manuscript, the scribal writing, its list of Buddhist scriptures, and its vocabulary. Our assessment argues that PT1257 was a copy of a document initiated and circulated by Tibetans, presumably among Chinese monasteries in Dunhuang, to learn the Chinese equivalents to Tibetan translation terminology that was already in use among Tibet- ans. -
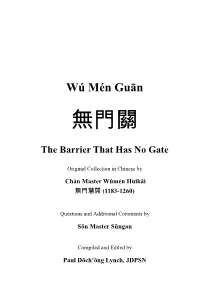
Gateless Gate Has Become Common in English, Some Have Criticized This Translation As Unfaithful to the Original
Wú Mén Guān The Barrier That Has No Gate Original Collection in Chinese by Chán Master Wúmén Huìkāi (1183-1260) Questions and Additional Comments by Sŏn Master Sǔngan Compiled and Edited by Paul Dōch’ŏng Lynch, JDPSN Page ii Frontspiece “Wú Mén Guān” Facsimile of the Original Cover Page iii Page iv Wú Mén Guān The Barrier That Has No Gate Chán Master Wúmén Huìkāi (1183-1260) Questions and Additional Comments by Sŏn Master Sǔngan Compiled and Edited by Paul Dōch’ŏng Lynch, JDPSN Sixth Edition Before Thought Publications Huntington Beach, CA 2010 Page v BEFORE THOUGHT PUBLICATIONS HUNTINGTON BEACH, CA 92648 ALL RIGHTS RESERVED. COPYRIGHT © 2010 ENGLISH VERSION BY PAUL LYNCH, JDPSN NO PART OF THIS BOOK MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM OR BY ANY MEANS, GRAPHIC, ELECTRONIC, OR MECHANICAL, INCLUDING PHOTOCOPYING, RECORDING, TAPING OR BY ANY INFORMATION STORAGE OR RETRIEVAL SYSTEM, WITHOUT THE PERMISSION IN WRITING FROM THE PUBLISHER. PRINTED IN THE UNITED STATES OF AMERICA BY LULU INCORPORATION, MORRISVILLE, NC, USA COVER PRINTED ON LAMINATED 100# ULTRA GLOSS COVER STOCK, DIGITAL COLOR SILK - C2S, 90 BRIGHT BOOK CONTENT PRINTED ON 24/60# CREAM TEXT, 90 GSM PAPER, USING 12 PT. GARAMOND FONT Page vi Dedication What are we in this cosmos? This ineffable question has haunted us since Buddha sat under the Bodhi Tree. I would like to gracefully thank the author, Chán Master Wúmén, for his grace and kindness by leaving us these wonderful teachings. I would also like to thank Chán Master Dàhuì for his ineptness in destroying all copies of this book; thankfully, Master Dàhuì missed a few so that now we can explore the teachings of his teacher. -

An Efficient Framework for Implementing Persistent Data Structures on Asymmetric NVM Architecture
AsymNVM: An Efficient Framework for Implementing Persistent Data Structures on Asymmetric NVM Architecture Teng Ma Mingxing Zhang Kang Chen∗ [email protected] [email protected] [email protected] Tsinghua University Tsinghua University & Sangfor Tsinghua University Beijing, China Shenzhen, China Beijing, China Zhuo Song Yongwei Wu Xuehai Qian [email protected] [email protected] [email protected] Alibaba Tsinghua University University of Southern California Beijing, China Beijing, China Los Angles, CA Abstract We build AsymNVM framework based on AsymNVM ar- The byte-addressable non-volatile memory (NVM) is a promis- chitecture that implements: 1) high performance persistent ing technology since it simultaneously provides DRAM-like data structure update; 2) NVM data management; 3) con- performance, disk-like capacity, and persistency. The cur- currency control; and 4) crash-consistency and replication. rent NVM deployment with byte-addressability is symmetric, The key idea to remove persistency bottleneck is the use of where NVM devices are directly attached to servers. Due to operation log that reduces stall time due to RDMA writes and the higher density, NVM provides much larger capacity and enables efficient batching and caching in front-end nodes. should be shared among servers. Unfortunately, in the sym- To evaluate performance, we construct eight widely used metric setting, the availability of NVM devices is affected by data structures and two transaction applications based on the specific machine it is attached to. High availability canbe AsymNVM framework. In a 10-node cluster equipped with achieved by replicating data to NVM on a remote machine. real NVM devices, results show that AsymNVM achieves However, it requires full replication of data structure in local similar or better performance compared to the best possible memory — limiting the size of the working set. -
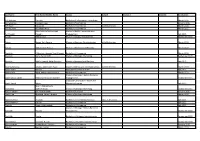
Last Name First Name/Middle Name Course Award Course 2 Award 2 Graduation
Last Name First Name/Middle Name Course Award Course 2 Award 2 Graduation A/L Krishnan Thiinash Bachelor of Information Technology March 2015 A/L Selvaraju Theeban Raju Bachelor of Commerce January 2015 A/P Balan Durgarani Bachelor of Commerce with Distinction March 2015 A/P Rajaram Koushalya Priya Bachelor of Commerce March 2015 Hiba Mohsin Mohammed Master of Health Leadership and Aal-Yaseen Hussein Management July 2015 Aamer Muhammad Master of Quality Management September 2015 Abbas Hanaa Safy Seyam Master of Business Administration with Distinction March 2015 Abbasi Muhammad Hamza Master of International Business March 2015 Abdallah AlMustafa Hussein Saad Elsayed Bachelor of Commerce March 2015 Abdallah Asma Samir Lutfi Master of Strategic Marketing September 2015 Abdallah Moh'd Jawdat Abdel Rahman Master of International Business July 2015 AbdelAaty Mosa Amany Abdelkader Saad Master of Media and Communications with Distinction March 2015 Abdel-Karim Mervat Graduate Diploma in TESOL July 2015 Abdelmalik Mark Maher Abdelmesseh Bachelor of Commerce March 2015 Master of Strategic Human Resource Abdelrahman Abdo Mohammed Talat Abdelziz Management September 2015 Graduate Certificate in Health and Abdel-Sayed Mario Physical Education July 2015 Sherif Ahmed Fathy AbdRabou Abdelmohsen Master of Strategic Marketing September 2015 Abdul Hakeem Siti Fatimah Binte Bachelor of Science January 2015 Abdul Haq Shaddad Yousef Ibrahim Master of Strategic Marketing March 2015 Abdul Rahman Al Jabier Bachelor of Engineering Honours Class II, Division 1 -

A Dictionary of Kristang (Malacca Creole Portuguese) with an English-Kristang Finderlist
A dictionary of Kristang (Malacca Creole Portuguese) with an English-Kristang finderlist PacificLinguistics REFERENCE COpy Not to be removed Baxter, A.N. and De Silva, P. A dictionary of Kristang (Malacca Creole Portuguese) English. PL-564, xxii + 151 pages. Pacific Linguistics, The Australian National University, 2005. DOI:10.15144/PL-564.cover ©2005 Pacific Linguistics and/or the author(s). Online edition licensed 2015 CC BY-SA 4.0, with permission of PL. A sealang.net/CRCL initiative. Pacific Linguistics 564 Pacific Linguistics is a publisher specialising in grammars and linguistic descriptions, dictionaries and other materials on languages of the Pacific, Taiwan, the Philippines, Indonesia, East Timor, southeast and south Asia, and Australia. Pacific Linguistics, established in 1963 through an initial grant from the Hunter Douglas Fund, is associated with the Research School of Pacific and Asian Studies at The Australian National University. The authors and editors of Pacific Linguistics publications are drawn from a wide range of institutions around the world. Publications are refereed by scholars with relevant expertise, who are usually not members of the editorial board. FOUNDING EDITOR: Stephen A. Wurm EDITORIAL BOARD: John Bowden, Malcolm Ross and Darrell Tryon (Managing Editors), I Wayan Arka, Bethwyn Evans, David Nash, Andrew Pawley, Paul Sidwell, Jane Simpson EDITORIAL ADVISORY BOARD: Karen Adams, Arizona State University Lillian Huang, National Taiwan Normal Peter Austin, School of Oriental and African University Studies -

The Incidental Learning of L2 Chinese Vocabulary Through Reading
Reading in a Foreign Language October 2020, Volume 32, No. 2 ISSN 1539-0578 pp. 169–193 The Incidental Learning of L2 Chinese Vocabulary through Reading Jing Zhou Pomona College United States Richard R. Day University of Hawai’i at Mānoa United States Abstract The study investigated the effect of marginal glossing and frequency of occurrence on the incidental learning of six aspects of vocabulary knowledge through reading in the second language (L2) Chinese. Participants were 30 intermediate L2 Chinese learners in an American public university. The MACOVA tests indicated that the treatment group who read with marginal glossing significantly outperformed (F = 6.686, p < 0.01) the control group who did not read with marginal glossing on six aspects of vocabulary knowledge after reading two stories. Significant differences were found on receptive word form, productive word form, receptive word meaning, and productive word grammatical function. The two-way ANOVA test suggested that the treatment group performed consistently better on learning words repeated three times and one time, and there was no interaction between the groups and the frequency of occurrence the words. The findings indicated that reading interesting and comprehensible Chinese stories can be beneficial for the learning of Chinese words. Keywords: L2 reading, marginal glossing, frequency of occurrence, incidental learning, receptive knowledge, productive knowledge, word form, word meaning, word grammatical function Vocabulary is one of the most important aspects of second or foreign language (L2) learning. However, the number of words needed to be learned to become proficient in the L2 is too large to learn through direct learning alone. -

A04 FES Background Docs
Attachment 4: SSC MRIP Workshop Aug 2019 Documentation and Information FES Calibration and Review The collection of documents contained in this pdf are only a part of the resources available on the FES calibration and review workshop website. That website also includes recorded webinar presentations given during the review workshop for the calibration models. That information can be found at the address below. https://www.fisheries.noaa.gov/event/fishing-effort-survey-calibration-model-peer-review 1 Attachment 4: SSC MRIP Workshop Aug 2019 A Small Area Estimation Approach for Reconciling Mode Differences in Two Surveys of Recreational Fishing Effort draft: please do not cite or distribute F. Jay Breidt Teng Liu Jean D. Opsomer Colorado State University June 10, 2017 Abstract For decades, the National Marine Fisheries Service has conducted a telephone survey of United States coastal households to estimate recreational effort (the number of fishing trips) in saltwater. The ef- fort estimates are computed for each of 17 US states along the coast of the Gulf of Mexico and the Atlantic Ocean, during six two-month waves (January-February through November-December). Recently, concerns about coverage errors in the telephone survey have led to implementation of a mail survey of the same population. Results from the mail survey are quite different from those of the telephone survey, due to coverage differences and mode effects, and a means of \cali- brating" or reconciling the two sets of estimates is needed by fisheries managers and stock assessment scientists. We develop a log-normal model for the estimates from the two surveys, accounting for tempo- ral dynamics through regression on population size and state-by-wave seasonal factors, and accounting in part for changing coverage prop- erties through regression on wireless telephone penetration. -
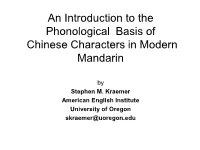
An Introduction to the Phonological Basis of Chinese Characters in Modern Mandarin
An Introduction to the Phonological Basis of Chinese Characters in Modern Mandarin by Stephen M. Kraemer American English Institute University of Oregon [email protected] 现代汉字语音简介 雷思遠 American English Institute University of Oregon [email protected] © Copyright 2009 Stephen M. Kraemer Phonetic Compound (形声字xingshengzi) • A “signific” part, which indicates meaning • plus • A “phonetic” part which indicates sound • 妈 [ma1] = 女 (female) + 马 [ma3] The Mandarin Syllable • A syllable in Modern Standard Mandarin • Consists of: • An initial • A final • A tone The Final • The final can also be broken down into a medial (vowel), a nucleus (vowel) and an ending (vowel or consonant) • Final = (M)N(E) Mandarin Consonants Source: Labial Labio- Dental Alveolar Alveo- Palatal Velar Kratochvil dental palatal (1968:25) stop p, p’ t, t’ k, k’ nasal m n (ŋ) fricative f s ʂ, ʐ(r) ɕ x lateral l affricate ts, ts’ tʂ, tʂ’ tɕ, tɕ’ Mandarin Vowels i ʅ i y(ü) u e ə ɤ o ɛ a ɑ Source: Cheng(1973:12) Background Literature • Xu Shen–說 文 解 字Shuo Wen Jie Zi (2nd cent. A.D.) • Soothill-1911 • Karlgren-1916, 1923a, 1923b, 1926, 1940, 1949, 1958 • Wieger-1927/1965 • Astor-1970 • Zhou Youguang-周有光 1978,1980, 2003 • Kraemer-1980, 1991a, 1991b • DeFrancis-1984 • Alber-1986, 1989 周有光 Zhou Youguang (1980) 汉字声旁读音便查 Hanzi shengpang duyin biancha ( A handy look up for the pronunciation of phonetics in Chinese characters) • Zhou analyzes characters in the Xin Hua Zidian (1971) based on Phonetic elements and sets up three categories of phonetic compound characters based on the similarity of the phonetic compound to the pronunciation of the phonetic itself. -

The Chinese Education Movement in Malaysia
INSTITUTIONS AND SOCIAL MOBILIZATION: THE CHINESE EDUCATION MOVEMENT IN MALAYSIA ANG MING CHEE NATIONAL UNIVERSITY OF SINGAPORE 2011 i 2011 ANG MING CHEE CHEE ANG MING SOCIAL MOBILIZATION:SOCIAL INSTITUTIONS AND THE CHINESE EDUCATION CHINESE MOVEMENT INTHE MALAYSIA ii INSTITUTIONS AND SOCIAL MOBILIZATION: THE CHINESE EDUCATION MOVEMENT IN MALAYSIA ANG MING CHEE (MASTER OF INTERNATIONAL STUDIES, UPPSALA UNIVERSITET, SWEDEN) (BACHELOR OF COMMUNICATION (HONOURS), UNIVERSITI SAINS MALAYSIA) A THESIS SUBMITTED FOR THE DEGREE OF DOCTOR OF PHILOSOPHY DEPARTMENT OF POLITICAL SCIENCE NATIONAL UNIVERSITY OF SINGAPORE 2011 iii ACKNOWLEDGEMENTS My utmost gratitude goes first and foremost to my supervisor, Associate Professor Jamie Seth Davidson, for his enduring support that has helped me overcome many challenges during my candidacy. His critical supervision and brilliant suggestions have helped me to mature in my academic thinking and writing skills. Most importantly, his understanding of my medical condition and readiness to lend a hand warmed my heart beyond words. I also thank my thesis committee members, Associate Professor Hussin Mutalib and Associate Professor Goh Beng Lan for their valuable feedback on my thesis drafts. I would like to thank the National University of Singapore for providing the research scholarship that enabled me to concentrate on my thesis as a full-time doctorate student in the past four years. In particular, I would also like to thank the Faculty of Arts and Social Sciences for partially supporting my fieldwork expenses and the Faculty Research Cluster for allocating the precious working space. My appreciation also goes to members of my department, especially the administrative staff, for their patience and attentive assistance in facilitating various secretarial works. -

Interracial Experience Across Colonial Hong Kong and Foreign Enclaves in China from the Late 1800S to the 1980S
Volume 14, Number 2 • Spring 2017 Erasure, Solidarity, Duplicity: Interracial Experience across Colonial Hong Kong and Foreign Enclaves in China from the late 1800s to the 1980s By Vicky Lee, Ph.D., Hong Kong Baptist University Abstract: How were Eurasians perceived and classified in Hong Kong and China during this hundred-year period? Blood admixture was only one of many ways: others included patrilineal descent, choice of family name, and socio-economic background. Family-imposed silence on one’s Eurasian background remained strong, and individual attempts to erase one’s Eurasian identity were common for survival reasons. It is no wonder that government authorities often had difficulty quantifying their Eurasian population. What experiences of erasure of Eurasianness were shared both collectively and individually? A strong sense of Eurasian solidarity was manifested in different forms, such as intermarriage and community cemeteries. Duplicity was another common element in their experience: Name-changing practices and submission to the new Japanese government during the Occupation sometimes rendered Eurasians suspect during and after wartime. Memoirs reflect the constant psychological harassment of Eurasians in patriotic Chinese schools during 1940s Peking and in Tsingdao, and Eurasians became frequent targets for criticism during the Maoist Era. Many Eurasians experienced psychological and physical torment as their very faces were evidence enough to subject them to criticism and punishments. Permalink: Citation: Lee, Vicky. “Erasure, Solidarity, Duplicity: usfca.edu/center-asia-pacific/perspectives/v14n2/Lee Interracial Experience across Colonial Hong Kong and Keywords: Foreign Enclaves in China from the late 1800s to the Chinese Eurasian, Mixed Identities, Colonial 1980s,” Asia Pacific Perspectives, Vol. -

A Survey of Taoist Literature : Tenth to Seventeenth Centuries
32 INSTITUTE OF EAST ASIAN STUDIES UNIVERSITY OF CALIFORNIA • BERKELEY CENTER FOR CHINESE STUDIES A Survey of Taoist Literature Tenth to Seventeenth Centuries Judith M. Boltz • \r<ye ^855#* INTERNATIONAL AND AREA STUDIES Richard Buxbaum, Dean International and Area Studies at the University of California, Berkeley, comprises four groups: international and comparative studies, area studies, teaching pro grams, and services to international programs. INSTITUTE OF EAST ASIAN STUDIES UNIVERSITY OF CALIFORNIA, BERKELEY The Institute of East Asian Studies, now a part of Berkeley International and Area Studies, was established at the University of California at Berkeley in the fall of 1978 to promote research and teaching on the cultures and societies of China, Japan, and Korea. It amalgamates the following research and instructional centers and programs: the Center for Chinese Studies, the Center for Japanese Studies, the Center for Korean Studies, the Group in Asian Studies, the Indochina Studies Pro ject, and the East Asia National Resource Center. INSTITUTE OF EAST ASIAN STUDIES Director: Frederic E. Wakeman, Jr. Associate Director: Joyce K. Kallgren Assistant Director: Joan P. Kask Executive Committee: Mary Elizabeth Berry Lowell Dittmer Thomas Gold Thomas Havens Joyce K. Kallgren Joan P. Kask Hong Yung Lee Jeffrey Riegel Ting Pang-hsin Wen-hsin Yeh CENTER FOR CHINESE STUDIES Chair: Wen-hsin Yeh CENTER FOR JAPANESE STUDIES Chair: Mary Elizabeth Berry CENTER FOR KOREAN STUDIES Chair: Hong Yung Lee GROUP IN ASIAN STUDIES Chair: Lowell Dittmer INDOCHINA STUDIES PROJECT Chair: Douglas Pike EAST ASIA NATIONAL RESOURCE CENTER Director: Frederic E. Wakeman, Jr. A Survey of Taoist Literature, Tenth to Seventeenth Centuries A publication of the Institute of East Asian Studies University of California Berkeley, California 94720 The China Research Monograph series is one of several publications series sponsored by the Institute of East Asian Studies in conjunction with its constituent units.