Civilian Evacuation to Devon in the Second World War
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Park Farm Culmstock, Cullompton, Devon EX15 3JY
Park Farm Culmstock, Cullompton, Devon EX15 3JY This most attractive and well- proportioned double fronted Edwardian farmhouse sits on the edge of the Blackdown Hills between Culmstock and Hemyock, has 5 bedrooms and 3 reception rooms with gardens and grounds extending in all to about 2.5 acres. Features • Entrance hall • Living room with open fireplace • Dining room with open fireplace • Fitted kitchen with oil fired Rayburn set within chimney breast • Study • Family room • Store room • Utility room • Downstairs shower room • Cloakroom • Master bedroom • 4 further double bedrooms • Family bathroom • Separate WC • Gardens and grounds extending to about 2.5 acres • Stables • Private drainage • Oil fired central heating • Council tax band F Park Farm is situated in a rural yet accessible location close to the Devon/Somerset border. It lies between the thriving villages of Hemyock (2.2 miles) and Culmstock (2.5 miles) on the edge of the Blackdown Hills. The village of Culmstock has a good range of local amenities including church, village store, petrol station, public house and primary school which feeds into the well regarded secondary school at Uffculme. Wellington is 9 miles and the County town of Taunton is 15 miles. The M5 motorway junctions at 26 and 27 are each within 10 miles of the property and Tiverton Parkway station with mainline service to London (1hr 58) is about 8 miles. Viewing strictly through the selling agents: Robert Cooney Corporation Street, Taunton, Somerset TA1 4AW Telephone 01823 230 230 E-mail [email protected] Website www.robertcooney.co.uk For identification purposes only. -

Minutes Document for Devon and Exeter Rail Project Working Party, 15/07/2016 14:00
1 CABINET DEVON AND EXETER RAIL PROJECT WORKING PARTY- 15/07/16 DEVON AND EXETER RAIL PROJECT WORKING PARTY 15 July 2016 Present:- Devon County Council: Councillors Ball, Biederman, Bowden, Eastman, Julian, Mathews, Sellis, Way, Westlake and Younger-Ross Exeter City Council Councillors Sutton, Wardle and Leadbetter East Devon District Council Councillors Bailey and Longhurst Mid Devon District Council Councillor Snow Teignbridge District Councill Councillors Goodey and Prowse Torbay Councill Councillors Doggett and Manning Members attending in accordance with Standing Order 25: Councillor Greenslade Apologies: Councillors Hughes, Squires, Flynn, Deed and Luggar 9 Minutes RESOLVED that the minutes of the meeting held on 19 February 2016 be signed as a correct record. 10 Update from Great Western Railway (Councillor Greenslade attended in accordance with Standing Order 25(2) and spoke to this item). Mr L Ward, Regional Development Planning and Programme Manager, gave a presentation which covered: passenger growth performance fleet update speed to the West stations investment depot investment community rail Matters discussed by Members with Mr Ward included: the Tarka line - Barnstaple growth; the need for early train to Exeter St David’s; and increased passenger capacity to be resolved by expansion; 2 CABINET DEVON AND EXETER RAIL PROJECT WORKING PARTY- 15/07/16 the use of Class 143s on the Exeter – Okehampton Sunday Rover service when available; new developments leading to population growth at Exminster and Bideford; lack of -

DRAFT General Meeting Minutes Wednesday 11Th November 2013 at 7.30Pm the Blackdown Healthy Living Centre
DRAFT General Meeting Minutes Wednesday 11 th November 2013 at 7.30pm The Blackdown Healthy Living Centre Present: Apologies received from: Chairperson: Heather Stallard (Hemyock PC) David Edmondson ( Pitminster PC) John Brabrook (Clerk Combe Raleigh) Cllr John Hart (Leader DCC) Margaret Lee (Pitminster PC) Lisa Turner (Blackdown Hills AONB) Catherine Bass (BHPN Co-ordinator) John Cornish (Upottery PC) Ken Pearson (Clerk Churchstanton) Cathy Gardner (Clerk Stockland) Gary Gardner (Stockland) Cllr. Frank Rosamond (Mid-DevonDC) Geoffrey Sworder (Dunkeswell PC) Graham Long (Upottery PC) Bruce Payne( Wellington w/out PC) Geoffrey Bass (Culmstock PC) Cllr. Andrew Moulding (DCC) D. Corden (Blackdown Support Group) Cllr. Paul Diviani (EDDC/DCC/Yarcombe) C. Fowler (Payhembury) Cllr Ray Radford (DCC) Clive McIntyre ( Kentisbeare) Roy Hare ( Culmstock PC) Linda Bennett ( Blackdown Hills AONB) John Barrow ( Dunkeswell PC) Kirsty Campbell ( DCC) Gill Beardsworth (BHPN Volunteer) 11 parishes represented Two part meeting: Part One: Cllr John Hart (Leader Devon CC) and Cllr John Osman (Leader Somerset CC) had agreed in September to attend this meeting and were briefed to address the unique cross border characteristics of the Network parishes. Questions were invited in advance of the meeting and those received were sent to both invitees. Cllr Osman withdrew due to an urgent issue arising, while also expressing concern at the level of detail in the questions he had received, however was able to send written replies (Questions and Somerset Answers attached). Welcome and Introduction Heather Stallard welcomed everyone to the meeting, and apologised for the unavoidable absence of Cllr Osman. She expressed disappointment at this, as many rural issues for the BHPN relate to both Counties and occasionally policies appear to diverge. -

EXETER LIVESTOCK CENTRE MARKET REPORT Friday 15Th May
EXETER LIVESTOCK CENTRE MARKET REPORT Friday 15th May Store Stock Market We are open for business! Our Markets are currently being run under very strict measures due to Covid-19. Following Government guidelines, ALL VENDORS must DROP & GO and only buyers are permitted into the market. HELP US TO HELP YOU and lets keep the Country fed with GREAT BRITISH FOOD! Today’s Market 241 Store Cattle 137 Stirks 78 Calves 22 Dairy 115 Pigs 54 Store Sheep EXETER LIVESTOCK CENTRE 01392 251261 [email protected] www.kivells.com Friday 15th May 241 Store Cattle Auctioneer: Simon Alford 07789 980203 Steers to £1170 Heifers to £1045 An excellent mid May entry of store cattle sold to a blistering trade with buyers from west Cornwall to north Yorkshire in attendance ensuring all types were strong money. Top price of the day was given for a pen of four outstanding pure bred yearling Simmental steers from Alan Brazier of Poltimore at a whopping £1170 apiece whilst another quality bunch of four Simmental bullocks (18m) eased to £1075 a head for Stephen Pearce of Liskeard. A couple of grand Charolais steers (25m) from the Shervington Family, Hittisleigh reached £1150 closely followed by a smart South Devon steer (20m) from Rob & Sue Greep, Cornwood at £1135, the latter also saw tremendous red Limousin steers (18m) make £1110. Groups of well farmed Aberdeen Angus steers (24m) ran to £1085 and £1080 for Russell & Alyson Retter of Cotleigh with later born Angus steers (16m) rising to £1075 for Peter Hendy of Plymouth. No really strong British Blue steers on offer although a group of four very decent Blues (25m) did reach £1040 for Garry Dunn of Okehampton whilst younger store steers saw a stunning Beef Shorthorn cross (11m) from Peter & Jake Chisholm of Hatherleigh make a creditable £980 and a pair of young (13m) Simmental steers from John & Jill Redman, Chagford saw £950 a life. -

Q CD Decision Report
Decision Register Ref Number Address Proposal Decision Decision Type Decision Date 15/00391/MOUT Land at NGR 295599 122818 (North Outline for the erection of REFUSE COMM 28/08/2015 of Bourchier Close) Bampton Devon between 15 and 20 dwellings and up to 2500 sq. m. of B1 floor space including landscaping, parking and provision of vehicular access from the B3190 Reasons In accordance with the requirements of Article 35 of the Town and Country Planning (Development Management Procedure) (England) Order 2015, in determining this application the Local Planning Authority has worked proactively and positively with the applicant to ensure that all relevant planning considerations have been properly resolved. This has included pre application discussion, negotiation and discussions. In accordance with paragraph 69 of the National Planning Policy Framework, the Local Planning Authority has also involved the community in the consideration of this application. Reasons 1 The emerging Local Plan Review 2013-2033 Proposed Submission proposes re-classification of Bampton's status a market town and key focus of development, to a village with a limited role and development to meet local needs only and to remove the allocation of which this site forms part. Although the site is currently still allocated under policy AL/BA/2 of the Mid Devon Allocations and Infrastructure DPD, the Local Planning Authority considers on balance that significant weight can be attributed to the emerging Local Plan Review 2013-2033 Proposed Submission to justify a refusal due -

SITUATION of POLLING STATIONS Election of Members of The
SITUATION OF POLLING STATIONS Election of Members of the European Parliament for the South West Region South West Region Date of Election: Thursday 23 May 2019 Hours of Poll: 7:00 am to 10:00 pm Notice is hereby given that: The situation of Polling Stations and the description of persons entitled to vote thereat are as follows: Station Ranges of electoral register numbers Situation of Polling Station Number of persons entitled to vote thereat Village Hall, Kentisbury, Barnstaple 1 AA-1 to AA-70 Village Hall, Kentisbury, Barnstaple 1 CX -1 to CX -264 Church Hall, St Peter`s Church, Strand Lane, Ashford 2 AB-1 to AB-232 The Pavillion, Atherington, Devon 3 AC-1 to AC-357 Norah Bellot Court, Vicarage Street, Barnstaple 4 AD -1 to AD -1177 Holy Trinity Church Hall, Barbican Terrace, Barnstaple 5 AE -1 to AE -725 Holy Trinity Church Hall, Barbican Terrace, Barnstaple 5 AU -1 to AU -264 Forches Children's Centre, Forches Avenue, Barnstaple 6 AF -1 to AF -1163 Forches and Whiddon Valley, Community Centre, Barton 7 AG-1 to AG-897 Road, Whiddon Valley Orchard Vale Community, School,, Westacott Road, 8 AH -1 to AH -1076 Whiddon Valley Orchard Vale Community, School,, Westacott Road, 8 DC -1 to DC -27 Whiddon Valley Children's Summer Club, 2 Charles Dart Crescent, 9 AI -1 to AI -831 Barnstaple Our Lady`s Catholic School, Chanters Hill, Barnstaple 10 AJ -1 to AJ -657 Chichester Court, Communal Lounge, Valley Close, 11 AK-1 to AK-347 Gorwell Valley Estate Chichester Court, Communal Lounge, Valley Close, 11 AT -1 to AT -506 Gorwell Valley Estate The -

The Blackmore Country (1906)
I II i II I THE LIBRARY OF THE UNIVERSITY OF CALIFORNIA LOS ANGELES IN THE SAME SERIES PRICE 6/- EACH THE SCOTT COUNTRY THE BURNS COUNTRY BY W. S. CROCKETT BY C. S. DOOGALL Minister of Twccdsmuir THE THE THACKERAY COUNTRY CANTERBURY PILGRIMAGES BY LEWIS MELVILLE BY II. SNOWDEN WARD THE INQOLDSBY COUNTRY THE HARDY COUNTRY BY CHAS. G. HAKI'ER BY CHAS. G. HARPER PUBLISHED BY ADAM AND CHARLES BLACK, SOHO SQUARE, LONDON Zbc pWQVimnQC Series CO THE BLACKMORE COUNTRY s^- Digitized by the Internet Archive in 2007 with funding from IVIicrosoft Corporation http://www.archive.org/details/blackmorecountryOOsneliala ON THE LYN, BELOW BRENDON. THE BLACKMORE COUNTRY BY F. J. SNELL AUTHOR OF 'A BOOK OF exmoob"; " kably associations of archbishop temple," etc. EDITOR of " UEMORIALS OF OLD DEVONSHIRE " WITH FIFTY FULL -PAGE ILLUSTRATIONS FROM PHOTOGRAPHS BY C. W. BARNES WARD LONDON ADAM AND CHARLES BLACK 1906 " So holy and so perfect is my love, That I shall think it a most plenteous crop To glean the broken ears after the man That the main harvest reaps." —Sir Phiup SroNEY. CORRIGENDA Page 22, line 20, for " immorality " read " morality." „ 128, „ 2 1, /or "John" r^a^/" Jan." „ 131, „ 21, /<7r "check" r?a^ "cheque." ; PROLOGUE The " Blackmore Country " is an expression requiring some amount of definition, as it clearly will not do to make it embrace the whole of the territory which he annexed, from time to time, in his various works of fiction, nor even every part of Devon in which he has laid the scenes of a romance. -

Ringing Devon
Ringing THE GUILD OF DEVONSHIRE RINGERS Devon Newsletter 108, December 2017 MERRY CHRISTMAS David took the trouble to go into detail about the principles Guild Events behind the judging, how judges like he and his wife Felicity approached the subject, what they looked for. He also gave Striking Competitions – Saturday October 21st detailed advice on how to proceed at the event, how to make the The Guild striking competitions 2017- a novice’s view most of the time and tips and hints for leading and tenor ringing. Held at three separate towers and organised by the North East With his kind permission, we have put together a transcript of his Branch, this year’s Guild competitions were a wholehearted remarks which is published as a separate article in this issue. success. Seen from the writer’s perspective - that of an entirely But the ringing is only part of a successful competition day. The novice ringer - the day showed all those qualities which ringers venues of Bampton and Stoodleigh in the morning and Silverton tend to take entirely for granted - qualities of true comradeship. in the afternoon provided what we all are tempted to take for Ringers are the most friendly group of people you’ll find and they granted in this Guild, that someone always provides tea, coffee came together on the 21st October with one purpose in mind - and biscuits for a mere pittance of a contribution. But at Silverton that of bringing the traditional music of the church tower to new the whole distaff side seemed to have been galvanized - no bread heights. -

Environment Agency South West Region
ENVIRONMENT AGENCY SOUTH WEST REGION 1997 ANNUAL HYDROMETRIC REPORT Environment Agency Manley House, Kestrel Way Sowton Industrial Estate Exeter EX2 7LQ Tel 01392 444000 Fax 01392 444238 GTN 7-24-X 1000 Foreword The 1997 Hydrometric Report is the third document of its kind to be produced since the formation of the Environment Agency (South West Region) from the National Rivers Authority, Her Majesty Inspectorate of Pollution and Waste Regulation Authorities. The document is the fourth in a series of reports produced on an annua! basis when all available data for the year has been archived. The principal purpose of the report is to increase the awareness of the hydrometry within the South West Region through listing the current and historic hydrometric networks, key hydrometric staff contacts, what data is available and the reporting options available to users. If you have any comments regarding the content or format of this report then please direct these to the Regional Hydrometric Section at Exeter. A questionnaire is attached to collate your views on the annual hydrometric report. Your time in filling in the questionnaire is appreciated. ENVIRONMENT AGENCY Contents Page number 1.1 Introduction.............................. .................................................... ........-................1 1.2 Hydrometric staff contacts.................................................................................. 2 1.3 South West Region hydrometric network overview......................................3 2.1 Hydrological summary: overview -
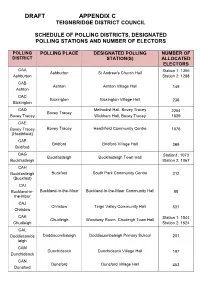
DRAFT Schedule of Polling Places and Designated Polling Stations
DRAFT APPENDIX C TEIGNBRIDGE DISTRICT COUNCIL SCHEDULE OF POLLING DISTRICTS, DESIGNATED POLLING STATIONS AND NUMBER OF ELECTORS POLLING POLLING PLACE DESIGNATED POLLING NUMBER OF DISTRICT STATION(S) ALLOCATED ELECTORS CAA Station 1: 1366 Ashburton St Andrew’s Church Hall Ashburton Station 2: 1288 CAB Ashton Ashton Village Hall 149 Ashton CAC Bickington Bickington Village Hall 236 Bickington CAD Methodist Hall, Bovey Tracey 2254 Bovey Tracey Bovey Tracey Wickham Hall, Bovey Tracey 1839 CAE Bovey Tracey Bovey Tracey Heathfield Community Centre 1076 (Heathfield) CAF Bridford Bridford Village Hall 369 Bridford CAG Station1: 1073 Buckfastleigh Buckfastleigh Town Hall Buckfastleigh Station 2: 1067 CAH Buckfastleigh Buckfast South Park Community Centre 312 (Buckfast) CAI Buckland-in- Buckland-in-the-Moor Buckland-in-the-Moor Community Hall 88 the-Moor CAJ Christow Teign Valley Community Hall 631 Christow CAK Station 1: 1544 Chudleigh Woodway Room, Chudeigh Town Hall Chudleigh Station 2: 1524 CAL Doddiscombs Doddiscombsleigh Doddiscombsleigh Primary School 201 leigh CAM Dunchideock Dunchideock Village Hall 197 Dunchideock CAN Dunsford Dunsford Village Hall 453 Dunsford DRAFT APPENDIX C CAO Station 1: 1397 Exminster Victory Hall, Exminster Exminster Station 2: 1439 CAP Hennock Hennock Hennock Village Hall 334 (Village) CAQ Hennock Chudleigh Knighton Chudleigh Knighton Village Hall 884 (Chudleigh Knighton) CAR Holcombe Holcombe Burnell Longdown Village Hall 405 Burnell CAS Ide Ide Memorial Hall 388 Ide CAT Ilsington Ilsington Village Hall 475 Ilsington -

VICTORIAN RURAL POLICEMAN Mini Project 2017
VICTORIAN RURAL POLICEMAN Mini Project 2017 Rural Constabularies were established following the Royal Commission which met between 1836 and 1839, the County Police Act of 1839 and the amending Act of 1840. In 1856 the County and Borough Police Act made the establishing of a police force mandatory for all counties and boroughs. All the police men in the mini project are listed as Police Constables in the 1881 census. The purpose of the project is to find out more about these rural policemen – who they were, how they lived and do they fit the quotations. FACHRS Ref: WATC01 Researcher Name: Timothy M Clark Policeman’s Name: STEPHEN CLARK Age in 1881 Census: 41 Source: - RG Number: 11 Piece: 2240 Folio: Page: 14 Reg. District: South Molton Parish: Warkleigh County Devon Migration, Employment and Social Status Information from each census about Stephen Clark and the household he lived in: Born 22 November 1839 at Malborough, South Devon, birth registered at Kingsbridge. Second son of William Steer Clark, mariner, and Sarah nee Jarvis, both Devon born, as were the 3 previous generations. YEAR 1841 1851 1861 1871 1881 1891 1901 1911 CENSUS H107 RG 9 RG 10 RG 11 RG 12 RG 13 PIECE 248 1412 2090 2240 1772 2144 FOLIO 92 23 104 PAGE 1 14 7 1 17 REG DIS 6 Upton South Molton South Molton Newport, St PARISH Malborough Tormoham Paignton Warkleigh Chittlehambolt John ADDRESS Buckley 12 Queen Warkleigh Village 20 Victoria 3 Hobbs Cottages Street Villa Street TOWN Salcombe Newton South Molton South Molton Barnstaple Barnstaple Abbot COUNTY Devon Devon Devon -

West Buckland School Bus Timetable – from 29Th August 2018 Croyde
West Buckland School Bus Timetable – From 29th August 2018 ROUTE 1 CROYDE INWARDS MON-THURS OUTWARDS FRI OUTWARDS Croyde – Bridge Holiday 7.40 1815 1735 Park-unison 7.42 1813 1733 Green Lanes Shopping centre 8.02 1735 1658 Sowden Lane 8.05 1735 1655 Walton Way (Toll House) 8.08 1732 1652 Goodleigh (Top of village) 8.11 1729 1649 Stone Cross Gunn 8.20 1720 1640 School 8.40 1710 1630 ROUTE 1A BRAUNTON INWARDS MON-THURS OUTWARDS FRI OUTWARDS Braunton – George Hotel 7.45 1755 1715 Wrafton Bus Stop 7.47 1753 1713 Chivenor, Bus stop by Army Camp 7.49 1751 1711 Ashford Bus Stop 7.52 1748 1708 Landkey Castle Inn 8.10 1735 1655 School 8.40 1710 1630 ROUTE 2 BARNSTAPLE INWARDS MON-THURS OUTWARDS FRI OUTWARDS Co-Op Store Pottington Estate 7.50 1755 1715 Barnstaple Square 7.55 1750 1710 Clinton Road 8.00 1745 1705 Litchdon Medical Centre 8.03 1742 1702 Mount Pleasant 8.05 1740 1700 Landkey (Top of Landkey Bus Stop) PM 1735 1655 ONLY Landkey Newlands 8.10 1734 1654 Swimbridge 8.15 1730 1650 Filleigh Garage 8.18 1727 1647 School 8.40 1710 1630 ROUTE 3 TORRINGTON INWARDS MON-THURS FRI OUTWARDS OUTWARDS Newton Tracey- Hunters Inn 7.40 1820 1740 Alverdiscott Cross Roads 7.42 1818 1738 Yarnscombe Paintball (MORNING ONLY) 7.43 Torrington Community College 7.50 1810 1730 High Bullen Garage 7.55 1805 1735 Canford Cross 7.59 1801 1731 Chittlehampton Square 8.15 1735 1655 Honey Beetle Cross 8.18 1732 1652 West Heddon Farm Lane end 8.20 1730 1650 Underhighdown 8.22 1728 1648 West Buckland Village 8.25 1725 1645 School 8.40 1710 1630 ROUTE 3A BIDEFORD INWARDS