Florida State Emergency Response Commission
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Propoxur United States Environmental Protection Agency
United States Prevention, Pesticides EPA738-R-97-009 Environmental Protection And Toxic Substances August 1997 Agency (7508W) Reregistration Eligibility Decision (RED) PROPOXUR UNITED STATES ENVIRONMENTAL PROTECTION AGENCY WASHINGTON, D.C. 20460 OFFICE OF PREVENTION, PESTICIDES AND TOXIC SUBSTANCES CERTIFIED MAIL Dear Registrant: I am pleased to announce that the Environmental Protection Agency has completed its reregistration eligibility review and decisions on the pesticide chemical case propoxur. The enclosed Reregistration Eligibility Decision (RED) contains the Agency's evaluation of the data base of this chemical, its conclusions of the potential human health and environmental risks of the current product uses, and its decisions and conditions under which these uses and products will be eligible for reregistration. The RED includes the data and labeling requirements for products for reregistration. It may also include requirements for additional data (generic) on the active ingredient to confirm the risk assessments. To assist you with a proper response, read the enclosed document entitled "Summary of Instructions for Responding to the RED." This summary also refers to other enclosed documents which include further instructions. You must follow all instructions and submit complete and timely responses. The first set of required responses is due 90 days from the receipt of this letter. The second set of required responses is due 8 months from the date of receipt of this letter. Complete and timely responses will avoid the Agency taking the enforcement action of suspension against your products. If you have questions on the product specific data requirements or wish to meet with the Agency, please contact the Special Review and Reregistration Division representative Bonnie Adler (703) 308-8523. -

Carbamate Pesticides Aldicarb Aldicarb Sulfoxide Aldicarb Sulfone
Connecticut General Statutes Sec 19a-29a requires the Commissioner of Public Health to annually publish a list setting forth all analytes and matrices for which certification for testing is required. Connecticut ELCP Drinking Water Analytes Revised 05/31/2018 Microbiology Total Coliforms Fecal Coliforms/ E. Coli Carbamate Pesticides Legionella Aldicarb Cryptosporidium Aldicarb Sulfoxide Giardia Aldicarb Sulfone Carbaryl Physicals Carbofuran Turbidity 3-Hydroxycarbofuran pH Methomyl Conductivity Oxamyl (Vydate) Minerals Chlorinated Herbicides Alkalinity, as CaCO3 2,4-D Bromide Dalapon Chloride Dicamba Chlorine, free residual Dinoseb Chlorine, total residual Endothall Fluoride Picloram Hardness, Calcium as Pentachlorophenol CaCO3 Hardness, Total as CaCO3 Silica Chlorinated Pesticides/PCB's Sulfate Aldrin Chlordane (Technical) Nutrients Dieldrin Endrin Ammonia Heptachlor Nitrate Heptachlor Epoxide Nitrite Lindane (gamma-BHC) o-Phosphate Metolachlor Total Phosphorus Methoxychlor PCB's (individual aroclors) Note 1 PCB's (as decachlorobiphenyl) Note 1 Demands Toxaphene TOC Nitrogen-Phosphorus Compounds Alachlor Metals Atrazine Aluminum Butachlor Antimony Diquat Arsenic Glyphosate Barium Metribuzin Beryllium Paraquat Boron Propachlor Cadmium Simazine Calcium Chromium Copper SVOC's Iron Benzo(a)pyrene Lead bis-(2-ethylhexyl)phthalate Magnesium bis-(ethylhexyl)adipate Manganese Hexachlorobenzene Mercury Hexachlorocyclopentadiene Molybdenum Nickel Potassium Miscellaneous Organics Selenium Dibromochloropropane (DBCP) Silver Ethylene Dibromide (EDB) -
Determination of the Residual Efficacy of Carbamate and Organophosphate
Yewhalaw et al. Malar J (2017) 16:471 DOI 10.1186/s12936-017-2122-3 Malaria Journal RESEARCH Open Access Determination of the residual efcacy of carbamate and organophosphate insecticides used for indoor residual spraying for malaria control in Ethiopia Delenasaw Yewhalaw1,2†, Meshesha Balkew3†, Josephat Shililu4, Sultan Suleman5, Alemayehu Getachew4, Gedeon Ashenbo4, Sheleme Chibsa6, Gunawardena Dissanayake6, Kristen George7, Dereje Dengela8, Yemane Ye‑Ebiyo4 and Seth R. Irish9* Abstract Background: Indoor residual spraying is one of the key vector control interventions for malaria control in Ethiopia. As malaria transmission is seasonal in most parts of Ethiopia, a single round of spraying can usually provide efective protection against malaria, provided the insecticide remains efective over the entire malaria transmission season. This experiment was designed to evaluate the residual efcacy of bendiocarb, pirimiphos-methyl, and two doses of pro‑ poxur on four diferent wall surfaces (rough mud, smooth mud, dung, and paint). Filter papers afxed to wall surfaces prior to spraying were analyzed to determine the actual concentration applied. Cone bioassays using a susceptible Anopheles arabiensis strain were done monthly to determine the time for which insecticides were efective in killing mosquitoes. Results: The mean insecticide dosage of bendiocarb applied to walls was 486 mg/m2 (target 400/mg). This treat‑ ment lasted 1 month or less on rough mud, smooth mud, and dung, but 4 months on painted surfaces. Pirimiphos- methyl was applied at 1854 mg/m2 (target 1000 mg/m2), and lasted between 4 and 6 months on all wall surfaces. Propoxur with a target dose of 1000 mg/m2 was applied at 320 mg/m2, and lasted 2 months or less on all surfaces, except painted surfaces (4 months). -

Pepper Spray Evaluation Project
If you have issues viewing or accessing this file, please contact us at NCJRS.gov. L~ Pepper Spray Evaluation Project Results of the Introduction of Oleoresin Capsicum (OC) into the Baltimore County, MD, Police Department ~QCIATIONose ' I ~ S~NCF.~s93 I June 21, 1995 I Final Report Prepared for: i National Institute of Justice i ! U.S. Department Of Justice I F IACP PROJECT STAFF I r"" Daniel N. Rosenblatt Executive Director I pRINCIP/~L PROJECT STAFF Jerome A. Needle Director, Programs and Research I John Firman Report Coordinator Charles E. I-Iigginbotham Director, Information and Services John Granfield Project Manager I Steven M. Edwards Research Consultant Jami Long-Onnen On-Site Research Coordinator I! Lynne Hargest Project Specialist i PROJECT SUPPORT Dawn Phoubandith Report Editor I Katherine Spivey Assistant Editor Carolyn Cockroft Staff Specialist Edmund J. Kelly Support Specialist I: Tony Occhiuzzo Staff Specialist Lt. Roger Gross Visiting Fellow Lara Walker Editorial Assistant I David Bright Research Assistant I I I.... I r-- TABLE OF CONTENTS I' " Page Acknowledgments i Executive Summary i I Introduction 1 L Literature Review 2 i Chloroacetophenone (CN) 2 Ochlorobenzylidene-Malononitrile (CS) 4 I Oleoresin Capsicum 6 IL Research Setting 10 1 BCPD Interest in a Force Alternative 11 I IIL Project Methodology 12 Process Evaluation 12 I Outcome Methodology 12 Development of the Measurement Instruments 13 ! Data Limitations 16 ! IV. Findings: Outcome Evaluation 18 Overview Analysis 18 Reasons/Use of Spray 21 ! Application of OC on Animals 44 Summary of Outcome Data 44 Findings Regarding the Five Principle Questions 48 I v. Findings: Process Evaluation 51 I Training Issues 51 BCPD Training 53 Decontamination/First Aid 54 I Standard Operating Procedure 54 Use-of-Force Issues 55 Reporting the Use of OC as a Use of Force 56 I Police Use of Deadly Force in Defense of OC Spray Attack 57 I VI. -

Nerve Agent - Lntellipedia Page 1 Of9 Doc ID : 6637155 (U) Nerve Agent
This document is made available through the declassification efforts and research of John Greenewald, Jr., creator of: The Black Vault The Black Vault is the largest online Freedom of Information Act (FOIA) document clearinghouse in the world. The research efforts here are responsible for the declassification of MILLIONS of pages released by the U.S. Government & Military. Discover the Truth at: http://www.theblackvault.com Nerve Agent - lntellipedia Page 1 of9 Doc ID : 6637155 (U) Nerve Agent UNCLASSIFIED From lntellipedia Nerve Agents (also known as nerve gases, though these chemicals are liquid at room temperature) are a class of phosphorus-containing organic chemicals (organophosphates) that disrupt the mechanism by which nerves transfer messages to organs. The disruption is caused by blocking acetylcholinesterase, an enzyme that normally relaxes the activity of acetylcholine, a neurotransmitter. ...--------- --- -·---- - --- -·-- --- --- Contents • 1 Overview • 2 Biological Effects • 2.1 Mechanism of Action • 2.2 Antidotes • 3 Classes • 3.1 G-Series • 3.2 V-Series • 3.3 Novichok Agents • 3.4 Insecticides • 4 History • 4.1 The Discovery ofNerve Agents • 4.2 The Nazi Mass Production ofTabun • 4.3 Nerve Agents in Nazi Germany • 4.4 The Secret Gets Out • 4.5 Since World War II • 4.6 Ocean Disposal of Chemical Weapons • 5 Popular Culture • 6 References and External Links --------------- ----·-- - Overview As chemical weapons, they are classified as weapons of mass destruction by the United Nations according to UN Resolution 687, and their production and stockpiling was outlawed by the Chemical Weapons Convention of 1993; the Chemical Weapons Convention officially took effect on April 291997. Poisoning by a nerve agent leads to contraction of pupils, profuse salivation, convulsions, involuntary urination and defecation, and eventual death by asphyxiation as control is lost over respiratory muscles. -

Pesticide Residue Monitoring in Sediment and Surface Water Within the South Florida Water Management District Volume 2
Technical Publication 91-01 Pesticide Residue Monitoring in Sediment and Surface Water Within the South Florida Water Management District Volume 2 by Richard J. Pfeuffer January 1991 This publication was produced at an annual cost of $243.75 or $.49 per copy to inform the public. 500 191 Produced on recycled paper. Water Quality Division Research and Evaluation Department South Florida Water Management District West Palm Beach, Florida A IBSTRAC'I' Pesticide monitoring data are collected under the requirements of several permits and agreements as an indicator of water quality. The monitoring provides data to determine shifts or adverse trends in the quality of water being delivered to Lake Okeechobee, Everglades National Park, and the Water Conservation Areas. In addition, pesticide residue data are collected throughout the South Florida Water Management District at locations selected to determine water quality conditions at the major water control points. Special investigations are performed on selected pesticides as required and follow-up sampling is conducted based on the pesticides detected. Data were collected from 13 stations in 1984. By 1988, the network was expanded to 29 stations. Currently, water and sediment samples are collected quarterly and analyzed for 67 pesticides, herbicides and degradation products. Out of a total of 197 surface water samples, 13 percent had detectable residues, while 25 percent of the 208 sediment samples had detectable residues. The compounds detected in the water samples included atrazine and zinc phosphide while a variety of compounds, including DDT, have been detected in the sediment. None of the residues detected are considered to have adverse health or environmental effects. -

Decision-Making in Chemical Warfare Agent (CWA) Response There Is a Lot of Fear Associated with Chemical Will Act Accordingly
Application Note: 102 Decision-Making in Chemical Warfare Agent (CWA) Response There is a lot of fear associated with Chemical will act accordingly. If the first responders Warfare Agents (CWAs). The misnomer over-react and immediately jump into full “Nerve Gas” quickly brings horrible images to encapsulation protection it could panic the the minds of many civilians. But if we lay aside public and cause unnecessary worry and the politics and fear, CWA detection should even injury. treated like other gas/vapor detection challenges. It should be a collaborative Over Protection Can Be Dangerous process encompassing physical clues, threat to the Responder scenario, biological clues, and a variety of Heat stress is the number one injury in sensing technologies. No one clue or HazMat response and immediately jumping technology is always correct. Experience and into full Level A encapsulation is a good way the use of multiple clues and technologies are of overheating oneself. Level A the keys to successful CWA response. encapsulation also makes one much more Understanding what the clues are and how to susceptible to slip, trip and fall injuries. layer them to make a decision is critical to Finally, over protection makes it harder to get successful CWA response. things done. When properly used, detection allows responders to respond at lower levels Why is Gas Detection Important? of Personal Protective Equipment (PPE) to Responders cannot rely on their senses for provide the highest levels of safety to decision-making. Without effectively knowing themselves and to the community that they how to use detection techniques responders protect. -

Review of Azinphos-Methyl Was Undertaken by the Office of Chemical Safety (OCS), Which Considered All the Toxicological Data and Information Submitted for the Review
The reconsideration of the active constituent azinphos-methyl, registrations of products containing azinphos-methyl and approvals of their associated labels PRELIMINARY REVIEW FINDINGS Volume 1: Review Summary OCTOBER 2006 Canberra Australia Azinphos-methyl review – Preliminary Review Findings © Australian Pesticides & Veterinary Medicines Authority 2006 This work is copyright. Apart from any use permitted under the Copyright Act 1968, no part may be reproduced without permission from the Australian Pesticides & Veterinary Medicines Authority. The Australian Pesticides & Veterinary Medicines Authority publishes this preliminary review findings report for the active constituent azinphos-methyl and products containing azinphos- methyl. For further information about this review or the Pesticides Review Program, contact: Manager Chemical Review Australian Pesticides & Veterinary Medicines Authority PO Box E 240 KINGSTON ACT 2604 Australia Telephone: 61 2 6272 3213 Facsimile: 61 2 6272 3218 Email: [email protected] APVMA web site: http://www.apvma.gov.au i Azinphos-methyl review – Preliminary Review Findings FOREWORD The Australian Pesticides & Veterinary Medicines Authority (APVMA) is an independent statutory authority with responsibility for the regulation of agricultural and veterinary chemicals in Australia. Its statutory powers are provided in the Agvet Codes scheduled to the Agricultural and Veterinary Chemicals Code Act 1994. The APVMA can reconsider the approval of an active constituent, the registration of a chemical product or -

Chemical Name Federal P Code CAS Registry Number Acutely
Acutely / Extremely Hazardous Waste List Federal P CAS Registry Acutely / Extremely Chemical Name Code Number Hazardous 4,7-Methano-1H-indene, 1,4,5,6,7,8,8-heptachloro-3a,4,7,7a-tetrahydro- P059 76-44-8 Acutely Hazardous 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide P050 115-29-7 Acutely Hazardous Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- P197 17702-57-7 Acutely Hazardous 1-(o-Chlorophenyl)thiourea P026 5344-82-1 Acutely Hazardous 1-(o-Chlorophenyl)thiourea 5344-82-1 Extremely Hazardous 1,1,1-Trichloro-2, -bis(p-methoxyphenyl)ethane Extremely Hazardous 1,1a,2,2,3,3a,4,5,5,5a,5b,6-Dodecachlorooctahydro-1,3,4-metheno-1H-cyclobuta (cd) pentalene, Dechlorane Extremely Hazardous 1,1a,3,3a,4,5,5,5a,5b,6-Decachloro--octahydro-1,2,4-metheno-2H-cyclobuta (cd) pentalen-2- one, chlorecone Extremely Hazardous 1,1-Dimethylhydrazine 57-14-7 Extremely Hazardous 1,2,3,4,10,10-Hexachloro-6,7-epoxy-1,4,4,4a,5,6,7,8,8a-octahydro-1,4-endo-endo-5,8- dimethanonaph-thalene Extremely Hazardous 1,2,3-Propanetriol, trinitrate P081 55-63-0 Acutely Hazardous 1,2,3-Propanetriol, trinitrate 55-63-0 Extremely Hazardous 1,2,4,5,6,7,8,8-Octachloro-4,7-methano-3a,4,7,7a-tetra- hydro- indane Extremely Hazardous 1,2-Benzenediol, 4-[1-hydroxy-2-(methylamino)ethyl]- 51-43-4 Extremely Hazardous 1,2-Benzenediol, 4-[1-hydroxy-2-(methylamino)ethyl]-, P042 51-43-4 Acutely Hazardous 1,2-Dibromo-3-chloropropane 96-12-8 Extremely Hazardous 1,2-Propylenimine P067 75-55-8 Acutely Hazardous 1,2-Propylenimine 75-55-8 Extremely Hazardous 1,3,4,5,6,7,8,8-Octachloro-1,3,3a,4,7,7a-hexahydro-4,7-methanoisobenzofuran Extremely Hazardous 1,3-Dithiolane-2-carboxaldehyde, 2,4-dimethyl-, O- [(methylamino)-carbonyl]oxime 26419-73-8 Extremely Hazardous 1,3-Dithiolane-2-carboxaldehyde, 2,4-dimethyl-, O- [(methylamino)-carbonyl]oxime. -

Chlorpyrifos, Part 1: Toxicology
JOURNAL OF PESTICIDE REFORM/ WINTER 1994 • VOL.14, NO. 4 ■ INSECTICIDE FACTSHEET CHLORPYRIFOS, PART 1: TOXICOLOGY The broad spectrum organophosphate insecticide chlorpyrifos is the most widely used insecticide in the U.S. Total use is estimated at almost 30 million pounds per year. Like all organophosphate insecticides, chlorpyrifos affects the nervous system by inhibiting an enzyme that is important in the transmission of nerve impulses. Symptoms of acute poisoning include headache, nausea, muscle twitching, and convulsions. Chlorpyrifos poisonings are reported to state and federal agencies more often than poisonings of almost every other insecticide. In both laboratory animals and humans, chlorpyrifos can also cause delayed effects on the nervous system. Some effects have been measured years after exposure. Human birth defects have been associated with exposure to chlorpyrifos products. In pregnant laboratory animals, chlorpyrifos exposure caused fetal death. Pups that did survive were smaller pups and did not survive as well as pups from unexposed mothers. Chlorpyrifos also affects the male reproductive system; exposure to a chlorpyrifos product has caused death of cells in male rat testes and a decrease in sperm production in cattle. Chlorpyrifos has caused genetic damage in human blood and lymph cells, mice spleen cells, and hamster bone marrow cells. Immune system abnormalities have been reported from patients exposed to chlorpyrifos. Many individuals report developing sensitivities to a broad array of substances following chlorpyrifos exposure. The second part of this factsheet will discuss human exposure to chlorpyrifos and the ecological effects of chlorpyrifos. BY CAROLINE COX mary agricultural uses are for oranges, al- plications are made annually. -
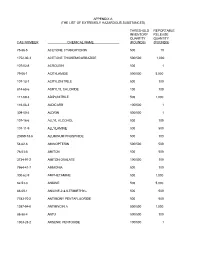
The List of Extremely Hazardous Substances)
APPENDIX A (THE LIST OF EXTREMELY HAZARDOUS SUBSTANCES) THRESHOLD REPORTABLE INVENTORY RELEASE QUANTITY QUANTITY CAS NUMBER CHEMICAL NAME (POUNDS) (POUNDS) 75-86-5 ACETONE CYANOHYDRIN 500 10 1752-30-3 ACETONE THIOSEMICARBAZIDE 500/500 1,000 107-02-8 ACROLEIN 500 1 79-06-1 ACRYLAMIDE 500/500 5,000 107-13-1 ACRYLONITRILE 500 100 814-68-6 ACRYLYL CHLORIDE 100 100 111-69-3 ADIPONITRILE 500 1,000 116-06-3 ALDICARB 100/500 1 309-00-2 ALDRIN 500/500 1 107-18-6 ALLYL ALCOHOL 500 100 107-11-9 ALLYLAMINE 500 500 20859-73-8 ALUMINUM PHOSPHIDE 500 100 54-62-6 AMINOPTERIN 500/500 500 78-53-5 AMITON 500 500 3734-97-2 AMITON OXALATE 100/500 100 7664-41-7 AMMONIA 500 100 300-62-9 AMPHETAMINE 500 1,000 62-53-3 ANILINE 500 5,000 88-05-1 ANILINE,2,4,6-TRIMETHYL- 500 500 7783-70-2 ANTIMONY PENTAFLUORIDE 500 500 1397-94-0 ANTIMYCIN A 500/500 1,000 86-88-4 ANTU 500/500 100 1303-28-2 ARSENIC PENTOXIDE 100/500 1 THRESHOLD REPORTABLE INVENTORY RELEASE QUANTITY QUANTITY CAS NUMBER CHEMICAL NAME (POUNDS) (POUNDS) 1327-53-3 ARSENOUS OXIDE 100/500 1 7784-34-1 ARSENOUS TRICHLORIDE 500 1 7784-42-1 ARSINE 100 100 2642-71-9 AZINPHOS-ETHYL 100/500 100 86-50-0 AZINPHOS-METHYL 10/500 1 98-87-3 BENZAL CHLORIDE 500 5,000 98-16-8 BENZENAMINE, 3-(TRIFLUOROMETHYL)- 500 500 100-14-1 BENZENE, 1-(CHLOROMETHYL)-4-NITRO- 500/500 500 98-05-5 BENZENEARSONIC ACID 10/500 10 3615-21-2 BENZIMIDAZOLE, 4,5-DICHLORO-2-(TRI- 500/500 500 FLUOROMETHYL)- 98-07-7 BENZOTRICHLORIDE 100 10 100-44-7 BENZYL CHLORIDE 500 100 140-29-4 BENZYL CYANIDE 500 500 15271-41-7 BICYCLO[2.2.1]HEPTANE-2-CARBONITRILE,5- -

Malathion Human Health and Ecological Risk Assessment Final Report
SERA TR-052-02-02c Malathion Human Health and Ecological Risk Assessment Final Report Submitted to: Paul Mistretta, COR USDA/Forest Service, Southern Region 1720 Peachtree RD, NW Atlanta, Georgia 30309 USDA Forest Service Contract: AG-3187-C-06-0010 USDA Forest Order Number: AG-43ZP-D-06-0012 SERA Internal Task No. 52-02 Submitted by: Patrick R. Durkin Syracuse Environmental Research Associates, Inc. 5100 Highbridge St., 42C Fayetteville, New York 13066-0950 Fax: (315) 637-0445 E-Mail: [email protected] Home Page: www.sera-inc.com May 12, 2008 Table of Contents Table of Contents............................................................................................................................ ii List of Figures................................................................................................................................. v List of Tables ................................................................................................................................. vi List of Appendices ......................................................................................................................... vi List of Attachments........................................................................................................................ vi ACRONYMS, ABBREVIATIONS, AND SYMBOLS ............................................................... vii COMMON UNIT CONVERSIONS AND ABBREVIATIONS.................................................... x CONVERSION OF SCIENTIFIC NOTATION ..........................................................................