Organophosphate Insecticides
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ACEPHATE (Addendum)
3 ACEPHATE (addendum) First draft prepared by Professor P.K. Gupta 1 and Dr Angelo Moretto 2 1 Rajinder Nagar, Bareilly, UP, India; 2 Dipartimento Medicina Ambientale e Sanità Pubblica, Università di Padova, Padova, Italy Explanation..........................................................................................................3 Evaluation for acceptable daily intake.................................................................4 Biochemical aspects ......................................................................................4 Oral absorption, distribution, excretion and metabolism .......................4 Toxicological studies.....................................................................................5 Acute toxicity.........................................................................................5 Short-term studies of toxicity.................................................................6 Special studies........................................................................................7 Studies on inhibition of cholinesterase activity in vitro ..................7 Short-term study of neurotoxicity ...................................................7 Developmental neurotoxicity..........................................................9 Observations in humans ..............................................................................10 Comments..........................................................................................................12 Toxicological evaluation ...................................................................................13 -

What Is the Difference Between Pesticides, Insecticides and Herbicides? Pesticide Effects on Food Production
What is the Difference Between Pesticides, Insecticides and Herbicides? Pesticides are chemicals that may be used to kill fungus, bacteria, insects, plant diseases, snails, slugs, or weeds among others. These chemicals can work by ingestion or by touch and death may occur immediately or over a long period of time. Insecticides are a type of pesticide that is used to specifically target and kill insects. Some insecticides include snail bait, ant killer, and wasp killer. Herbicides are used to kill undesirable plants or “weeds”. Some herbicides will kill all the plants they touch, while others are designed to target one species. Pesticide Effects on Food Production As the human population continues to grow, more and more crops are needed to meet this growing demand. This has increased the use of pesticides to increase crop yield per acre. For example, many farmers will plant a field with Soybeans and apply two doses of Roundup throughout the growing year to remove all other plants and prepare the field for next year’s crop. The Roundup is applied twice through the growing season to kill everything except the soybeans, which are modified to be pesticide resistant. After the soybeans are harvested, there is little vegetative cover on the field creating potential erosion issues for the reason that another crop can easily be planted. With this method, hundreds of gallons of chemicals are introduced into the environment every year. All these chemicals affect wildlife, insects, water quality and air quality. One greatly affected “good” insect are bees. Bees play a significant role in the pollination of the foods that we eat. -

Novel Approach to Fast Determination of 64 Pesticides Using of Ultra-Performance Liquid Chromatography-Tandem Mass Spectrometry
Novel approach to fast determination of 64 pesticides using of ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) Tomas Kovalczuk, Ondrej Lacina, Martin Jech, Jan Poustka, Jana Hajslova To cite this version: Tomas Kovalczuk, Ondrej Lacina, Martin Jech, Jan Poustka, Jana Hajslova. Novel approach to fast determination of 64 pesticides using of ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS). Food Additives and Contaminants, 2008, 25 (04), pp.444-457. 10.1080/02652030701570156. hal-00577414 HAL Id: hal-00577414 https://hal.archives-ouvertes.fr/hal-00577414 Submitted on 17 Mar 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Food Additives and Contaminants For Peer Review Only Novel approach to fast determination of 64 pesticides using of ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) Journal: Food Additives and Contaminants Manuscript ID: TFAC-2007-065.R1 Manuscript Type: Original Research Paper Date Submitted by the 07-Jul-2007 Author: Complete List of Authors: -

Historical Perspectives on Apple Production: Fruit Tree Pest Management, Regulation and New Insecticidal Chemistries
Historical Perspectives on Apple Production: Fruit Tree Pest Management, Regulation and New Insecticidal Chemistries. Peter Jentsch Extension Associate Department of Entomology Cornell University's Hudson Valley Lab 3357 Rt. 9W; PO box 727 Highland, NY 12528 email: [email protected] Phone 845-691-7151 Mobile: 845-417-7465 http://www.nysaes.cornell.edu/ent/faculty/jentsch/ 2 Historical Perspectives on Fruit Production: Fruit Tree Pest Management, Regulation and New Chemistries. by Peter Jentsch I. Historical Use of Pesticides in Apple Production Overview of Apple Production and Pest Management Prior to 1940 Synthetic Pesticide Development and Use II. Influences Changing the Pest Management Profile in Apple Production Chemical Residues in Early Insect Management Historical Chemical Regulation Recent Regulation Developments Changing Pest Management Food Quality Protection Act of 1996 The Science Behind The Methodology Pesticide Revisions – Requirements For New Registrations III. Resistance of Insect Pests to Insecticides Resistance Pest Management Strategies IV. Reduced Risk Chemistries: New Modes of Action and the Insecticide Treadmill Fermentation Microbial Products Bt’s, Abamectins, Spinosads Juvenile Hormone Analogs Formamidines, Juvenile Hormone Analogs And Mimics Insect Growth Regulators Azadirachtin, Thiadiazine Neonicotinyls Major Reduced Risk Materials: Carboxamides, Carboxylic Acid Esters, Granulosis Viruses, Diphenyloxazolines, Insecticidal Soaps, Benzoyl Urea Growth Regulators, Tetronic Acids, Oxadiazenes , Particle Films, Phenoxypyrazoles, Pyridazinones, Spinosads, Tetrazines , Organotins, Quinolines. 3 I Historical Use of Pesticides in Apple Production Overview of Apple Production and Pest Management Prior to 1940 The apple has a rather ominous origin. Its inception is framed in the biblical text regarding the genesis of mankind. The backdrop appears to be the turbulent setting of what many scholars believe to be present day Iraq. -
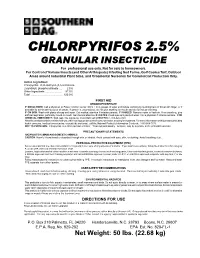
CHLORPYRIFOS 2.5% GRANULAR INSECTICIDE for Professional Use Only
CHLORPYRIFOS 2.5% GRANULAR INSECTICIDE For professional use only. Not for sale to homeowners. For Control of Various Insects (and Other Arthropods) Infesting Sod Farms, Golf Course Turf, Outdoor Areas around Industrial Plant Sites, and Ornamental Nurseries for Commercial Production Only. Active Ingredient: Chlorpyrifos: O,O-diethyl-0-(3,5,6-trichloro- 2-pyridinyl) phosphorothioate .... 2.5% Other Ingredients ....................... 97.5% Total ............................................ 100.0% FIRST AID ORGANOPHOSPHATE IF SWALLOWED: Call a physician or Poison Control Center. Drink 1 or 2 glasses of water and induce vomiting by touching back of throat with finger, or if available by administering syrup of ipecac. If person is unconscious, do not give anything by mouth and do not induce vomiting. IF ON SKIN: Wash with plenty of soap and water. Get medical attention if irritation persists. IF INHALED: Remove victim to fresh air. If not breathing, give artificial respiration, preferably mouth-to-mouth. Get medical attention. IF IN EYES: Flush eyes with plenty of water. Call a physician if irritation persists. FOR CHEMICAL EMERGENCY: Spill, leak, fire, exposure, or accident call CHEMTREC 1-800-424-9300. Have the product container or label with you when calling a poison control center or doctor, or going for treatment. For more information on this product (including health concerns, medical emergencies, or pesticide incidents), call the National Pesticide Information Center at: 1-800-858-7378. NOT TO PHYSICIAN: Chlorpyrifos is a cholinesterase inhibitor. Treat symptomatically. Atropine, only by injection, is the preferable antidote. PRECAUTIONARY STATEMENTS HAZARDS TO HUMANS AND DOMESTIC ANIMALS CAUTION: Harmful if swallowed or absorbed through skin or inhaled. -

Comments of Teresa Homan with Attachments
Teresa Homan Watertown, SD 57201 I am a landowner in Deuel County, South Dakota. Our land boarders the Deuel Harvest Wind Project in Deuel county, Docket # EL 18-053. There are 112 towers cited in the project, with 9 towers within a mile of our property. We have spent over three decades developing this property to enhance wildlife and for the enjoyment of our family. Can you imagine how we felt when we found we have a population of eastern bluebirds? We have yellow warblers, which by the way feed on the web worms that form in our trees. We have orioles, cedar waxwings, brown thrashers, rose breasted grosbeaks, gold finches, purple finches, robins, blue jays, nuthatches, eastern kingbirds, bitterns, dark eyed juncos, red winged blackbirds, morning doves, owls, cow birds, northern mocking birds, grey cat birds, wood thrushes, tufted titmouse, king fishers, indigo buntings, scarlet tanagers, bobolinks, meadowlarks, many woodpeckers, turkeys, turkey vultures, even humming birds and bald eagles. There are more, just to numerous to list. Many of these birds we have seen for the first time in our lives on this property in the past 1 O years. Not only are these birds beautiful and fun to watch, they have their purpose in the ecosystem. We also see northern long eared bats, that are on the endangered list in South Dakota. These birds are making a come back after the use of insecticides that nearly wiped out many. In the 1940's the insecticide DDT was introduced for public use, it is now banned from sale. In 1976 the herbicide Roundup was introduced to the public. -

Environmental Properties of Chemicals Volume 2
1 t ENVIRONMENTAL 1 PROTECTION Esa Nikunen . Riitta Leinonen Birgit Kemiläinen • Arto Kultamaa Environmental properties of chemicals Volume 2 1 O O O O O O O O OO O OOOOOO Ol OIOOO FINNISH ENVIRONMENT INSTITUTE • EDITA Esa Nikunen e Riitta Leinonen Birgit Kemiläinen • Arto Kultamaa Environmental properties of chemicals Volume 2 HELSINKI 1000 OlO 00000001 00000000000000000 Th/s is a second revfsed version of Environmental Properties of Chemica/s, published by VAPK-Pub/ishing and Ministry of Environment, Environmental Protection Department as Research Report 91, 1990. The pubiication is also available as a CD ROM version: EnviChem 2.0, a PC database runniny under Windows operating systems. ISBN 951-7-2967-2 (publisher) ISBN 952-7 1-0670-0 (co-publisher) ISSN 1238-8602 Layout: Pikseri Julkaisupalvelut Cover illustration: Jussi Hirvi Edita Ltd. Helsinki 2000 Environmental properties of chemicals Volume 2 _____ _____________________________________________________ Contents . VOLUME ONE 1 Contents of the report 2 Environmental properties of chemicals 3 Abbreviations and explanations 7 3.1 Ways of exposure 7 3.2 Exposed species 7 3.3 Fffects________________________________ 7 3.4 Length of exposure 7 3.5 Odour thresholds 8 3.6 Toxicity endpoints 9 3.7 Other abbreviations 9 4 Listofexposedspecies 10 4.1 Mammais 10 4.2 Plants 13 4.3 Birds 14 4.4 Insects 17 4.5 Fishes 1$ 4.6 Mollusca 22 4.7 Crustaceans 23 4.8 Algae 24 4.9 Others 25 5 References 27 Index 1 List of chemicals in alphabetical order - 169 Index II List of chemicals in CAS-number order -

Development of a CEN Standardised Method for Liquid Chromatography Coupled to Accurate Mass Spectrometry
Development of a CEN standardised method for liquid chromatography coupled to accurate mass spectrometry CONTENTS 1. Aim and scope ................................................................................................................. 2 2. Short description ................................................................................................................ 2 3. Apparatus and consumables ......................................................................................... 2 4. Chemicals ........................................................................................................................... 2 5. Procedure ........................................................................................................................... 3 5.1. Sample preparation ................................................................................................... 3 5.2. Recovery experiments for method validation ...................................................... 3 5.3. Extraction method ...................................................................................................... 3 5.4. Measurement .............................................................................................................. 3 5.5. Instrumentation and analytical conditions ............................................................ 4 5.5.1. Dionex Ultimate 3000 .......................................................................................... 4 5.5.2. QExactive Focus HESI source parameters ..................................................... -

Florida State Emergency Response Commission
Florida State Emergency Response Commission Sub-Committee on Training (SOT) HAZARDOUS MATERIALS MEDICAL TREATMENT PROTOCOLS Version 3.3 TOXIDROMES Toxidromes are clinical syndromes that the patient presents with. These patterns of signs and symptoms are essential for the successful recognition of chemical exposure. The toxidromes identified in this protocol are chemical exposure based while others such as the opioids are found within general medical protocol. These chemical toxidromes are identified clinically into five syndromes: Irritant Gas Toxidrome Asphyxiant Toxidrome Corrosive Toxidrome Hydrocarbon and Halogenated Hydrocarbons Toxidrome Cholinergic Toxidrome Each can present as a clinical manifestation of the chemical/poisoning involved with some cross-over between toxidromes. This list combines the toxic syndromes found within NFPA 473 (A.5.4.1(2) and traditional syndromes. Toxidrome Correlation to NFPA Standard 473 and Traditional Syndromes Toxidrome NFPA 473 A.5.4.1(2) Hazardous Materials Protocol Correlation Irritant Gas (j) Irritants Bronchospasm OC Pepper spray & lacrimants Asphyxiant (c) Chemical asphyxiants Carbon Monoxide (d) Simple asphyxiants Aniline dyes, Nitriles, Nitrares (h) Blood Agents Cyanide & Hydrogen Sulfide (n) Nitrogen Compounds Closed Space Fires Simple Asphyxants Corrosive (a) Corrosives Hydrofluroic Acid (g) Vesicants Chemical burns to the eye Choramine and Chlorine Hydrocarbon (e) Organic solvents Phenol and (q) Phenolic Compounds Halogenated Hydrocarbons Halogenated Hydrocarbons Cholinergic (b) Pesticides -

The Spruce Budworm, Choristoneura Fumiferana
02-01370 Spruce Budworm Bro 10/10/02 11:09 AM Page 1 MORE INFORMATION The he spruce budworm, Choristoneura fumiferana For more information on Spruce Budworms call: The Tree Line Spruce (Clemens), is the most destructive and widely (204) 945-7866. Or write: Budworm distributed forest defoliator in North America. Manitoba Conservation Forestry Branch In Manitoba T Forest Health and Ecology The destructive phase of this pest is the larval or caterpillar 200 Saulteaux Crescent Winnipeg, Manitoba R3J 3W3 stage. Massive budworm outbreaks occur periodically, Web site: www.gov.mb.ca/natres/forestry/ destroying hundreds of thousands of hectares of valuable fir and spruce. Aerial view of budworm damage In eastern Canada the budworm’s preferred food is balsam fir, Photos courtesy of Canadian Forest Service, Great Lakes Forest Research Centre, white spruce and red spruce. In Manitoba, the budworm Sault Ste. Marie, Ontario and Northern Forest Research Centre, Edmonton, Alberta. feeds primarily on white spruce and balsam fir, and, less frequently, on black spruce. 02-01370 Spruce Budworm Bro 10/10/02 11:09 AM Page 2 DESCRIPTION OF LIFE STAGES LIFE CYCLE DAMAGE CONTROL The adult moth has a wingspread of The female moth lays In light and moderate infestations Various insecticides are used 21 to 30 mm. It is grey-brown in its eggs in July on the damage is restricted to a partial against the spruce budworm to colour with silvery white patches on underside of needles. loss of new foliage, particularly in protect valuable spruce and fir the forewings. Normally, the eggs the upper crown trees. -

422 Part 180—Tolerances and Ex- Emptions for Pesticide
Pt. 180 40 CFR Ch. I (7–1–16 Edition) at any time before the filing of the ini- 180.124 Methyl bromide; tolerances for resi- tial decision. dues. 180.127 Piperonyl butoxide; tolerances for [55 FR 50293, Dec. 5, 1990, as amended at 70 residues. FR 33360, June 8, 2005] 180.128 Pyrethrins; tolerances for residues. 180.129 o-Phenylphenol and its sodium salt; PART 180—TOLERANCES AND EX- tolerances for residues. 180.130 Hydrogen Cyanide; tolerances for EMPTIONS FOR PESTICIDE CHEM- residues. ICAL RESIDUES IN FOOD 180.132 Thiram; tolerances for residues. 180.142 2,4-D; tolerances for residues. Subpart A—Definitions and Interpretative 180.145 Fluorine compounds; tolerances for Regulations residues. 180.151 Ethylene oxide; tolerances for resi- Sec. dues. 180.1 Definitions and interpretations. 180.153 Diazinon; tolerances for residues. 180.3 Tolerances for related pesticide chemi- 180.154 Azinphos-methyl; tolerances for resi- cals. dues. 180.4 Exceptions. 180.155 1-Naphthaleneacetic acid; tolerances 180.5 Zero tolerances. for residues. 180.6 Pesticide tolerances regarding milk, 180.163 Dicofol; tolerances for residues. eggs, meat, and/or poultry; statement of 180.169 Carbaryl; tolerances for residues. policy. 180.172 Dodine; tolerances for residues. 180.175 Maleic hydrazide; tolerances for resi- Subpart B—Procedural Regulations dues. 180.176 Mancozeb; tolerances for residues. 180.7 Petitions proposing tolerances or ex- 180.178 Ethoxyquin; tolerances for residues. emptions for pesticide residues in or on 180.181 Chlorpropham; tolerances for resi- raw agricultural commodities or proc- dues. essed foods. 180.182 Endosulfan; tolerances for residues. 180.8 Withdrawal of petitions without preju- 180.183 Disulfoton; tolerances for residues. -

Approach to Site-Selective Protein Modification JUSTIN M
A “Tag-and-Modify” Approach to Site-Selective Protein Modification JUSTIN M. CHALKER, GONC-ALO J. L. BERNARDES, AND BENJAMIN G. DAVIS* Department of Chemistry, University of Oxford, Chemistry Research Laboratory, 12 Mansfield Road, Oxford OX1 3TA, United Kingdom RECEIVED ON FEBRUARY 27, 2011 CONSPECTUS ovalent modification can expand a protein's functional capacity. Fluorescent or radioactive labeling, for instance, allows C imaging of a protein in real time. Labeling with an affinity probe enables isolation of target proteins and other interacting molecules. At the other end of this functional spectrum, protein structures can be naturally altered by enzymatic action. ProteinÀprotein interactions, genetic regulation, and a range of cellular processes are under the purview of these post- translational modifications. The ability of protein chemists to install these covalent additions selectively has been critical for elucidating their roles in biology. Frequently the transformations must be applied in a site-specific manner, which demands the most selective chemistry. In this Account, we discuss the development and application of such chemistry in our laboratory. A centerpiece of our strategy is a “tag-and-modify” approach, which entails sequential installation of a uniquely reactive chemical group into the protein (the “tag”) and the selective or specific modification of this group. The chemical tag can be a natural or unnatural amino acid residue. Of the natural residues, cysteine is the most widely used as a tag. Early work in our program focused on selective disulfide formation in the synthesis of glycoproteins. For certain applications, the susceptibility of disulfides to reduction was a limitation and prompted the development of several methods for the synthesis of more stable thioether modifications.