1 Skin Infections Among Elderly Living in Long-Term Care Facilities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2U11/13U195 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date Χ n n 20 October 2011 (20.10.2011) 2U11/13U195 Al (51) International Patent Classification: ka Pharmaceutical Co., Ltd., 1-7-1, Dosho-machi, Chuo- C12P 19/34 (2006.01) C07H 21/04 (2006.01) ku, Osaka-shi, Osaka 541-0045 (JP). (21) International Application Number: (74) Agents: KELLOGG, Rosemary et al; Swanson & PCT/US201 1/032017 Bratschun, L.L.C., 8210 SouthPark Terrace, Littleton, Colorado 80120 (US). (22) International Filing Date: 12 April 201 1 (12.04.201 1) (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, English (25) Filing Language: AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (26) Publication Language: English CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (30) Priority Data: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 61/323,145 12 April 2010 (12.04.2010) US KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (71) Applicants (for all designated States except US): SOMA- ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, LOGIC, INC. [US/US]; 2945 Wilderness Place, Boulder, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, Colorado 80301 (US). OTSUKA PHARMACEUTI¬ SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, CAL CO., LTD. -

Module Test № 1 on Dermatology
THE MINISTRY OF HEALTHCARE OF THE RUSSIAN FEDERATION FEDERAL STATE BUDGETARY EDUCATIONAL INSTITUTION OF HIGHER PROFESSIONAL EDUCATION PIROGOV RUSSIAN NATIONAL RESEARCH MEDICAL UNIVERSITY DEPARTMENT OF DERMATOVENEROLOGY Gaydina T.A., Dvornikov A.S., Skripkina P.A., Nazhmutdinova D.K., Heydar S.A., Arutunyan G.B., Pashinyan A.G. MODULE TEST №1 ON DERMATOLOGY FOR STUDENTS OF INSTITUTES OF HIGHER MEDICAL EDUCATION ON SPECIALTY THERAPEUTIC FACULTY DEPARTMENT OF DERMATOVENEROLOGY Moscow 2016 ISBN УДК ББК A21 Module test №1 on Dermatology for students of institutes of high medical education on specialty «Therapeutic faculty» department of dermatovenerology: manual for students for self-training//FSBEI HPE “Pirogov RNRMU” of the ministry of healthcare of the russian federation, M.: (publisher) 2016, 144 p. The manual is a part of teaching-methods on Dermatovenerology. It contains tests on Dermatology on the topics of practical sessions requiring single or multiple choice anser. The manual can be used to develop skills of students during practical sessions. It also can be used in the electronic version at testing for knowledge. The manual is compiled according to FSES on specialty “therapeutic faculty”, working programs on dermatovenerology. The manual is intended for foreign students of 3-4 courses on specialty “therapeutic faculty” and physicians for professional retraining. Authors: Gaydina T.A. – candidate of medical science, assistant of dermatovenerology department of therapeutic faculty Pirogov RNRMU Dvornikov A.S. – M.D., professor of dermatovenerology department of therapeutic faculty Pirogov RNRMU Skripkina P.A. – candidate of medical science, assistant professor of dermatovenerology department of therapeutic faculty Pirogov RNRMU Nazhmutdinova D.K. – candidate of medical science, assistant professor of dermatovenerology department of therapeutic faculty Pirogov RNRMU Heydar S.A. -

Update of the Guideline on Chronic Pruritus
Update of the Guideline on Chronic Pruritus Developed by the Guideline Subcommittee “Chronic Pruritus” of the European Dermatology Forum Subcommittee Members: Prof. Dr. Elke Weisshaar, Heidelberg (Germany) Prof. Dr. Sonja Ständer, Münster (Germany) Prof. Dr. Erwin Tschachler, Wien (Austria) Prof. Dr. Torello Lotti, Florence (Italy) Prof. Dr. Johannes Ring, Munich (Germany) Prof. Dr. Laurent Misery, Brest (France) Dr. Markus Streit, Aarau (Switzerland) Prof. Dr. Thomas Mettang, Wiesbaden (Germany) Prof. Dr. Jacek Szepietowski, Wroclaw (Poland) Prof. Dr. Joanna Wallengren, Lund (Sweden) Dr. Peter Maisel, Münster (Germany) Prof. Dr. Uwe Gieler, Gießen (Germany) Prof. Dr. Malcolm Greaves (Singapore) Prof. Dr. Ulf Darsow, Munich (Germany) Prof. Dr. Julien Lambert, Antwerp (Belgium) Members of EDF Guideline Committee: Prof. Dr. Werner Aberer, Graz (Austria) Prof. Dr. Dieter Metze, Münster (Germany) Prof. Dr. Martine Bagot, Paris (France) Dr. Kai Munte, Rotterdam (Netherlands) Prof. Dr. Nicole Basset-Seguin, Paris (France) Prof. Dr. Gilian Murphy, Dublin (Ireland) Prof. Dr. Ulrike Blume-Peytavi, Berlin (Germany) Prof. Dr. Martino Neumann, Rotterdam (Netherlands) Prof. Dr. Lasse Braathen, Bern (Switzerland) Prof. Dr. Tony Ormerod, Aberdeen (UK) Prof. Dr. Sergio Chimenti, Rome (Italy) Prof. Dr. Mauro Picardo, Rome (Italy) Prof. Dr. Alexander Enk, Heidelberg (Germany) Prof. Dr. Johannes Ring, Munich (Germany) Prof. Dr. Claudio Feliciani, Rome (Italy) Prof. Dr. Annamari Ranki, Helsinki (Finland) Prof. Dr. Claus Garbe, Tübingen (Germany) Prof. Dr. Berthold Rzany, Berlin (Germany) Prof. Dr. Harald Gollnick, Magdeburg (Germany) Prof. Dr. Rudolf Stadler, Minden (Germany) Prof. Dr. Gerd Gross, Rostock (Germany) Prof. Dr. Sonja Ständer, Münster (Germany) Prof. Dr. Vladimir Hegyi, Bratislava (Slovakia) Prof. Dr. Eggert Stockfleth, Berlin (Germany) Prof. Dr. -

Abstracts from the 9Th World Congress on Itch October 15–17, 2017
ISSN 0001-5555 ActaDV Volume 97 2017 SEPTEMBER, No. 8 ADVANCES IN DERMATOLOGY AND VENEREOLOGY A Non-profit International Journal for Interdisciplinary Skin Research, Clinical and Experimental Dermatology and Sexually Transmitted Diseases Abstracts from the 9th World Congress on Itch October 15–17, 2017 Official Journal of - European Society for Dermatology and Wroclaw, Poland Psychiatry Affiliated with - The International Forum for the Study of Itch Immediate Open Access Acta Dermato-Venereologica www.medicaljournals.se/adv Abstracts from the 9th World Congress on Itch DV cta A enereologica V Organizing Committee Scientific Committee ermato- Congress President: Jacek C Szepietowski (Wroclaw, Poland) Jeffrey D. Bernhard (Massachusetts, USA) D Congress Secretary General: Adam Reich (Rzeszów, Poland) Earl Carstens (Davis, USA) Congress Secretary: Edyta Lelonek (Wroclaw, Poland) Toshiya Ebata (Tokyo, Japan) cta Alan Fleischer (Lexington, USA) A IFSI President: Earl Carstens (Davis, USA) IFSI Vice President: Elke Weisshaar (Heidelberg, Germany) Ichiro Katayama (Osaka, Japan) Ethan Lerner (Boston, USA) Staff members of the Department of Dermatology, Venereology and Allergology, Wroclaw Medical University, Wroclaw, Poland Thomas Mettang (Wiesbaden, Germany) Martin Schmelz (Mannheim, Germany) Sonja Ständer (Münster, Germany) DV Jacek C. Szepietowski (Wroclaw, Poland) cta Kenji Takamori (Tokyo, Japan) A Elke Weisshaar (Heidelberg, Germany) Gil Yosipovitch (Miami, USA) Contents of this Abstract book Program 1000 Abstracts: Lecture Abstracts 1008 Poster Abstracts 1035 Author Index 1059 dvances in dermatology and venereology A www.medicaljournals.se/acta doi: 10.2340/00015555-2773 Journal Compilation © 2017 Acta Dermato-Venereologica. Acta Derm Venereol 2017; 97: 999–1060 1000 9th World Congress of Itch Sunday, October 15, 2017 Abstract # 1:30-3:30 PM IFSI Board meeting DV 5:00-5:20 PM OPENING CEREMONY 5:00-5:10 PM Opening remarks cta Jacek C. -

Clinical Spectrum of Ageing Versus Non-Ageing Geriatric Dermatoses -A Case-Controlled Study in Tertiary Care Centre, Tamil Nadu, South India
IP Indian Journal of Clinical and Experimental Dermatology 2020;6(2):151–159 Content available at: iponlinejournal.com IP Indian Journal of Clinical and Experimental Dermatology Journal homepage: www.innovativepublication.com Original Research Article Clinical spectrum of ageing versus non-ageing geriatric dermatoses -A case-controlled study in tertiary care centre, Tamil Nadu, South India C Abhirami1, P K Kaviarasan1,*, B Poorana1, K Kannambal1, P V S Prasad1, N Chidambaram2 1Dept. of Dermatology Venereology & Leprosy, Rajah Muthiah Medical College and Hospital, Annamalai University, Chidambaram, Tamil Nadu, India 2Dept. of Medicine, Rajah Muthiah Medical College and Hospital, Annamalai University, Chidambaram, Tamil Nadu, India ARTICLEINFO ABSTRACT Article history: Introduction: Ageing process is a complex phenomenon which affects all organs in the body as well as Received 17-05-2020 skin. Geriatric dermatoses can be regarded as a cutaneous marker of underlying systemic disorders and Accepted 29-05-2020 internal malignancies. This was study aimed to analyse various clinical ageing patterns among elderly aged Available online 25-06-2020 above 60 years. Objectives: To determine the prevalence of clinical patterns of ageing and non-ageing dermatoses among elderly compare with non-dermatology patients. Keywords: Materials and Methods: An observational study, conducted on 300 patients aged 60 years and above were Ageing analysed for geriatric dermatoses. Of them 211 patients were subjects attended dermatology OPD (group Dermatoses A) and 89 patients were controls (Group B) from other were selected from specialties.. Detailed history, Geriatric through examination and appropriate investigations were done after obtaining informed consent. Pruritus Ageing Results: Out of 300 patients, males were (192, 64%) and females (108, 36%), the male female ratio of Pruritus 1.77:1. -

Pathophysiology and Treatment of Pruritus in Elderly
International Journal of Molecular Sciences Review Pathophysiology and Treatment of Pruritus in Elderly Bo Young Chung † , Ji Young Um †, Jin Cheol Kim , Seok Young Kang , Chun Wook Park and Hye One Kim * Department of Dermatology, Kangnam Sacred Heart Hospital, Hallym University, Seoul KS013, Korea; [email protected] (B.Y.C.); [email protected] (J.Y.U.); [email protected] (J.C.K.); [email protected] (S.Y.K.); [email protected] (C.W.P.) * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: Pruritus is a relatively common symptom that anyone can experience at any point in their life and is more common in the elderly. Pruritus in elderly can be defined as chronic pruritus in a person over 65 years old. The pathophysiology of pruritus in elderly is still unclear, and the quality of life is reduced. Generally, itch can be clinically classified into six types: Itch caused by systemic diseases, itch caused by skin diseases, neuropathic pruritus, psychogenic pruritus, pruritus with multiple factors, and from unknown causes. Senile pruritus can be defined as a chronic pruritus of unknown origin in elderly people. Various neuronal mediators, signaling mechanisms at neuronal terminals, central and peripheral neurotransmission pathways, and neuronal sensitizations are included in the processes causing itch. A variety of therapies are used and several novel drugs are being developed to relieve itch, including systemic and topical treatments. Keywords: elderly; ion channel; itch; neurotransmission pathophysiology of itch; pruritogen; senile pruritus; treatment of itch 1. Introduction Citation: Chung, B.Y.; Um, J.Y.; Kim, Pruritus is a relatively common symptom that anyone can experience at any point in J.C.; Kang, S.Y.; Park, C.W.; Kim, H.O. -

Dermatology in Geriatrics a Gandhi, M Gandhi, S Kalra
The Internet Journal of Geriatrics and Gerontology ISPUB.COM Volume 5 Number 2 Dermatology in Geriatrics A Gandhi, M Gandhi, S Kalra Citation A Gandhi, M Gandhi, S Kalra. Dermatology in Geriatrics. The Internet Journal of Geriatrics and Gerontology. 2009 Volume 5 Number 2. Abstract Over the past few years the world's population has continued on its remarkable transition from a state of high birth and death rates to one characterized by low birth and death rates. Consequently, primary care physicians and dermatologists will see more elderly patients presenting age related dermatological conditions.As people age, their chances of developing skin-related disorders increase due to multiple underlying medical conditions i.e. diabetes mellitus, atherosclerosis and decreased immunity. Common skin disorders found in the elderly individual are xerosis, pruritus, eczematous dermatitis, purpura, chronic venous insufficiency, psychocutaneous disorders etc. Caregivers and medical personnel can help decrease or prevent the development of many skin disorders in the elderly by addressing several factors i.e patient’s nutritional status, medical history, current medications, allergies, physical limitations, mental state, and personal hygiene and for specific underlying etiologies; several pharmacological treatment choices are suggested. INTRODUCTION and assisted living facilities3 .Caregivers and medical The famous old saying OLD IS GOLD doesn’t apply to personnel can help decrease or prevent the development of human skin as elderly people are recognized by their many skin disorders in the elderly by addressing several wrinkled and dull skin. The population is getting older, with factors i.e patient’s nutritional state, medical history, current a greater percentage of the population in the over-65 age medications, allergies, physical limitations, mental state, and group. -
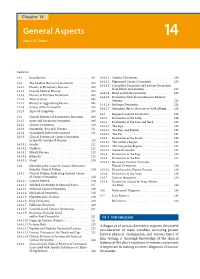
General Aspects 14 Niels K
14_199_254* 05.11.2005 10:15 Uhr Seite 201 Chapter 14 General Aspects 14 Niels K. Veien Contents 14.1 Introduction . 201 14.4.2.1 Cement Ulcerations . 224 14.4.2.2 Pigmented Contact Dermatitis . 225 14.2 The Medical History of the Patient . 202 14.4.2.3 Caterpillar Dermatitis and Irritant Dermatitis 14.2.1 History of Hereditary Diseases . 202 from Plants and Animals . 225 14.2.2 General Medical History . 202 14.4.2.4 Head and Neck Dermatitis . 225 14.2.3 History of Previous Dermatitis . 203 14.4.2.5 Dermatitis from Transcutaneous Delivery 14.2.4 Time of Onset . 203 Systems . 225 14.2.5 History of Aggravating Factors . 204 14.4.2.6 Berloque Dermatitis . 226 14.2.6 Course of the Dermatitis . 205 14.4.2.7 Stomatitis due to Mercury or Gold Allergy . 226 14.2.7 Types of Symptoms . 205 14.5 Regional Contact Dermatitis . 226 14.3 Clinical Features of Eczematous Reactions . 206 14.5.1 Dermatitis of the Scalp . 226 14.3.1 Acute and Recurrent Dermatitis . 206 14.5.2 Dermatitis of the Face and Neck . 228 14.3.2 Chronic Dermatitis . 210 14.5.2.1 The Lips . 230 14.3.3 Nummular (Discoid) Eczema . 211 14.5.2.2 The Eyes and Eyelids . 230 14.3.4 Secondarily Infected Dermatitis . 211 14.5.2.3 The Ear . 231 14.3.5 Clinical Features of Contact Dermatitis 14.5.3 Dermatitis of the Trunk . 232 in Specific Groups of Persons . 212 14.5.3.1 The Axillary Region . -

Id Reaction Associated with Red Tattoo Ink
CASE LETTER Id Reaction Associated With Red Tattoo Ink Alexandra Price, MD; Masoud Tavazoie, MD, PhD; Shane A. Meehan, MD; Marie Leger, MD, PhD 1 month later, she developed pruritic papulonodular PRACTICE POINTS lesions localized to the red-pigmented areas of the tattoo. • Hypersensitivity reactions to tattoo pigment are on Concomitantly, the patient developed a similar eruption the rise due to the increasing popularity and preva- confined to areas of red pigment in a polychromatic tattoo lence of tattoos. Systemic allergic reactions to tattoo on the right upper arm that she had obtained 10 years ink are rare but can cause considerable morbidity. prior. She was treated with intralesional triamcinolone to • Id reaction, also known as autoeczematization or several of the lesionscopy on the right dorsal foot with some autosensitization, is a reaction that develops distant benefit; however, a few days later she developed a gener- to an initial site of infection or sensitization. alized, erythematous, pruritic eruption on the back, abdo- • Further investigation of color additives in tattoo pig- men, arms, and legs. Her medical history was remarkable ments is warranted to better elucidate the compo- only for mild iron-deficiency anemia. She had no known nents responsible for cutaneous allergic reactions drugnot allergies or history of atopy and was not taking any associated with tattoo ink. medications prior to the onset of the eruption. Skin examination revealed multiple, well-demarcated, eczematous papulonodules with surrounding erythema To the Editor: Doconfined to the red-pigmented areas of the tattoo on Although relatively uncommon, hypersensitivity reactions the right dorsal foot, with several similar lesions on to tattoo pigment are on the rise due to the increasing the surrounding nontattooed skin (Figure 1). -

Menlo Therapeutics Inc. June 2019
Menlo Therapeutics Inc. June 2019 Developing Serlopitant, a Once-Daily Oral NK1 Receptor Antagonist for Pruritus Safe Harbor Statements Special Note Regarding Forward-Looking Statements This presentation contains forward-looking statements, including statements about our plans to develop and commercialize our product candidates, our planned clinical trials for serlopitant, the timing of the availability of data from our clinical trials, the timing of our planned regulatory filings, the timing of and our ability to obtain and maintain regulatory approvals for serlopitant and the clinical utility of serlopitant, alone and as compared to other treatment options, the duration of patent protection, and other statements regarding strategy, future operations and plans, as well as assumptions underlying such statements. These statements involve substantial known and unknown risks, uncertainties and other factors, some of which are outside of our control, that may cause our actual results, levels of activity, performance or achievements to be materially different from the information expressed or implied by these forward- looking statements, including risks related to the clinical drug development process, the regulatory approval process, our reliance on third parties, and our ability to defend our intellectual property. We may not actually achieve the plans, intentions or expectations disclosed in our forward-looking statements, and you should not place undue reliance on our forward-looking statements. Actual results or events could differ materially from the plans, intentions and expectations disclosed in the forward-looking statements we make. Additional information that could lead to material changes in our performance is contained in our filings with the U.S. Securities and Exchange Commission. -

Delete Afterwards
G N O TIO F IA DE C R O M S S A T A O N L SCIENTIFIC CONFERENCE A O I G R I E S T I S N ABSTRACTS . N.A D. A Peculiar Case Of Darier's Disease In A Patient With HIV Infection Otrofanowei E1, Ayanlowo OO2, Akinkugbe AO2, Gold-Olufadi SA1 1Department of Medicine, Lagos University Teaching Hospital, Lagos, Nigeria 2Department of Medicine, College of Medicine, University of Lagos, Nigeria. INTRODUCTION: Darier's disease (Keratosis METHODS: Clinical examination of a young man follicularis) is a rare autosomal dominant who presented with a two month history of genodermatosis with mutations in the ATP2A2 gene worsening vegetative, warty-like malodourous which is necessary for the SERCA2 protein- a calcium lesions in the axillae, gluteal cleft, groin and nape. pump. This causes abnormal intracellular Ca2+ Routine investigations were carried out and a skin signaling, notably involving the endoplasmic biopsy was sent for histopathology. reticulum. The result is a loss of suprabasilar cell RESULT: Investigations revealed essentially normal adhesion(acantholysis) and an induction of apoptosis haemogram with an elevated ESR and a positive (dyskeratosis). With a worldwide prevalence of about 1 retroviral status, whilst histology confirmed Darier's to 4 per 100,000, it has no race or sex predilection and it is disease with characteristic suprabasal acantholysis in a characterized by greasy hyperkeratotic papules in dilapidated brick wall appearance. He was seborrheic areas. There are associated nail and mucosal commenced on anti-retroviral medication as well as changes and the disease usually runs a chronic course. -

Mallory Prelims 27/1/05 1:16 Pm Page I
Mallory Prelims 27/1/05 1:16 pm Page i Illustrated Manual of Pediatric Dermatology Mallory Prelims 27/1/05 1:16 pm Page ii Mallory Prelims 27/1/05 1:16 pm Page iii Illustrated Manual of Pediatric Dermatology Diagnosis and Management Susan Bayliss Mallory MD Professor of Internal Medicine/Division of Dermatology and Department of Pediatrics Washington University School of Medicine Director, Pediatric Dermatology St. Louis Children’s Hospital St. Louis, Missouri, USA Alanna Bree MD St. Louis University Director, Pediatric Dermatology Cardinal Glennon Children’s Hospital St. Louis, Missouri, USA Peggy Chern MD Department of Internal Medicine/Division of Dermatology and Department of Pediatrics Washington University School of Medicine St. Louis, Missouri, USA Mallory Prelims 27/1/05 1:16 pm Page iv © 2005 Taylor & Francis, an imprint of the Taylor & Francis Group First published in the United Kingdom in 2005 by Taylor & Francis, an imprint of the Taylor & Francis Group, 2 Park Square, Milton Park Abingdon, Oxon OX14 4RN, UK Tel: +44 (0) 20 7017 6000 Fax: +44 (0) 20 7017 6699 Website: www.tandf.co.uk All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior permission of the publisher or in accordance with the provisions of the Copyright, Designs and Patents Act 1988 or under the terms of any licence permitting limited copying issued by the Copyright Licensing Agency, 90 Tottenham Court Road, London W1P 0LP. Although every effort has been made to ensure that all owners of copyright material have been acknowledged in this publication, we would be glad to acknowledge in subsequent reprints or editions any omissions brought to our attention.