Pathology Confirmation of Particle Embolization of Middle Meningeal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anomalous Origin of the Middle Meningeal Artery
The Internet Journal of Radiology ISPUB.COM Volume 4 Number 2 Anomalous Origin of the Middle Meningeal Artery from the Petrous Segment of the Internal Carotid Artery Associated with Multiple Cerebrovascular Abnormalities I Omeis, M Crupain, M Tenner, R Murali Citation I Omeis, M Crupain, M Tenner, R Murali. Anomalous Origin of the Middle Meningeal Artery from the Petrous Segment of the Internal Carotid Artery Associated with Multiple Cerebrovascular Abnormalities. The Internet Journal of Radiology. 2005 Volume 4 Number 2. Abstract A 25-year-old male with a history of seizure disorder was found incidentally on cerebral angiography to have numerous congenital anomalies of the cerebral vascular system. Among these anomalies were the derivation of the left middle meningeal artery from the petrous portion of the internal carotid artery, the presence of a left cavernous angioma, cavernous origin of the left ophthalmic artery, and an accessory middle cerebral artery. Awareness of cerebral circulatory anatomical anomalies of this nature is of importance to all physicians who plan surgical and endovascular interventions. INTRODUCTION resonance imaging (MRI) with and without gadolinium The middle meningeal artery in most individuals arises from revealed a left temporal lobe cavernoma and associated the maxillary branch of the external carotid artery and enters developmental venous anomaly in the region of the collateral the skull through the foramen spinosum. It then divides into gyrus that were unchanged from of first diagnosis (Fig. 2). anterior and posterior branches to supply the dura and An electroencephalogram (EEG) showed some mild cerebral adjacent calvarium. A few instances have been reported of dysfunction over the left temporal region with no the aberrant origin of the middle meningeal artery from epileptiform abnormality. -

Clinical Importance of the Middle Meningeal Artery
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Jagiellonian Univeristy Repository FOLIA MEDICA CRACOVIENSIA 41 Vol. LIII, 1, 2013: 41–46 PL ISSN 0015-5616 Przemysław Chmielewski1, Janusz skrzat1, Jerzy waloCha1 CLINICAL IMPORTANCE OF THE MIDDLE MENINGEAL ARTERY Abstract: Middle meningeal artery (MMA)is an important branch which supplies among others cranial dura mater. It directly attaches to the cranial bones (is incorporated into periosteal layer of dura mater), favors common injuries in course of head trauma. This review describes available data on the MMA considering its varability, or treats specific diseases or injuries where the course of MMA may have clinical impact. Key words: Middle meningeal artery (MMA), aneurysm of the middle meningeal artery, epidural he- matoma, anatomical variation of MMA. TOPOGRAPHY OF THE MIDDLE MENINGEAL ARTERY AND ITS BRANCHES Middle meningeal artery (MMA) [1] is most commonly the strongest branch of maxillary artery (from external carotid artery) [2]. It supplies blood to cranial dura mater, and through the numerous perforating branches it nourishes also periosteum of the inner aspect of cranial bones. It enters the middle cranial fossa through the foramen spinosum, and courses between the dura mater and the inner aspect of the vault of the skull. Next it divides into two terminal branches — frontal (anterior) which supplies blood to bones forming anterior cranial fossa and the anterior part of the middle cranial fossa; parietal branch (posterior), which runs more horizontally toward the back and supplies posterior part of the middle cranial fossa and supratentorial part of the posterior cranial fossa. -

The Ophthalmic Artery Ii
Brit. J. Ophthal. (1962) 46, 165. THE OPHTHALMIC ARTERY II. INTRA-ORBITAL COURSE* BY SOHAN SINGH HAYREHt AND RAMJI DASS Government Medical College, Patiala, India Material THIS study was carried out in 61 human orbits obtained from 38 dissection- room cadavers. In 23 cadavers both the orbits were examined, and in the remaining fifteen only one side was studied. With the exception of three cadavers of children aged 4, 11, and 12 years, the specimens were from old persons. Method Neoprene latex was injected in situ, either through the internal carotid artery or through the most proximal part of the ophthalmic artery, after opening the skull and removing the brain. The artery was first irrigated with water. After injection the part was covered with cotton wool soaked in 10 per cent. formalin for from 24 to 48 hours to coagulate the latex. The roof of the orbit was then opened and the ophthalmic artery was carefully studied within the orbit. Observations COURSE For descriptive purposes the intra-orbital course of the ophthalmic artery has been divided into three parts (Singh and Dass, 1960). (1) The first part extends from the point of entrance of the ophthalmic artery into the orbit to the point where the artery bends to become the second part. This part usually runs along the infero-lateral aspect of the optic nerve. (2) The second part crosses over or under the optic nerve running in a medial direction from the infero-lateral to the supero-medial aspect of the nerve. (3) The thirdpart extends from the point at which the second part bends at the supero-medial aspect of the optic nerve to its termination. -

Dural Arteriovenous Malformation of the Major Venous Sinuses: an Acquired Lesion
13 Dural Arteriovenous Malformation of the Major Venous Sinuses: An Acquired Lesion Mohammad Y. Chaudhary,1.2 Arteriovenous malformations of the dura are thought to be congenital. However, Ved P. Sachdev3 arteriographic investigations of four patients who, after a head injury, developed dural Soo H. Ch01 arteriovenous fistulae with features of congenital malformations suggest that these Imre Weitzner, Jr.1 abnormal communications may also be acquired. Thrombosis or thrombophlebitis in Smiljan Puljic2 the dural sinus or vein may be the primary event in their formation. The pathogenesis Yun Peng Huang 1 is probably " growth" of the dural arteries normally present in the walls of the sinuses during the organization of an intraluminal thrombus. This may result in a direct communication between artery and vein or sinus, establishing an abnormal shunt. Ultimate fibrosis of the sinus wall and intraluminal thrombus may be the factors responsible for the spontaneous disappearance of such malformations. Most dural arteriovenous malformations (AVMs) that involve th e major venous sinuses present either spontaneously or as incidental findings during arteriog raphy performed for other reasons. They occur predominantly in women over age 40 years [1]. The angiomatous network, multiple feeding arteries, numerous arteriovenous (A V) shunts, and occasional association with cerebral angiomas [2], as well as a few cases reported in children [3], suggest that these AVM s are congenital. Thrombosis of the draining sinus or vein is thought to be responsible for the occasional spontaneous disappearance of these lesions [4, 5]. Our experience with four patients who, after a head injury, developed dural AV fistulae with features of congenital malformations prompted a review of th e literature and this report. -

Clinical Importance of the Middle Meningeal Artery
FOLIA MEDICA CRACOVIENSIA 41 Vol. LIII, 1, 2013: 41–46 PL ISSN 0015-5616 Przemysław Chmielewski1, Janusz skrzat1, Jerzy waloCha1 CLINICAL IMPORTANCE OF THE MIDDLE MENINGEAL ARTERY Abstract: Middle meningeal artery (MMA)is an important branch which supplies among others cranial dura mater. It directly attaches to the cranial bones (is incorporated into periosteal layer of dura mater), favors common injuries in course of head trauma. This review describes available data on the MMA considering its varability, or treats specific diseases or injuries where the course of MMA may have clinical impact. Key words: Middle meningeal artery (MMA), aneurysm of the middle meningeal artery, epidural he- matoma, anatomical variation of MMA. TOPOGRAPHY OF THE MIDDLE MENINGEAL ARTERY AND ITS BRANCHES Middle meningeal artery (MMA) [1] is most commonly the strongest branch of maxillary artery (from external carotid artery) [2]. It supplies blood to cranial dura mater, and through the numerous perforating branches it nourishes also periosteum of the inner aspect of cranial bones. It enters the middle cranial fossa through the foramen spinosum, and courses between the dura mater and the inner aspect of the vault of the skull. Next it divides into two terminal branches — frontal (anterior) which supplies blood to bones forming anterior cranial fossa and the anterior part of the middle cranial fossa; parietal branch (posterior), which runs more horizontally toward the back and supplies posterior part of the middle cranial fossa and supratentorial part of the posterior cranial fossa. Branches of MMA traverse the arterial grooves giving rise to abundant lateral tracts which supply dura mater and periosteum. -

Anatomy of the Middle Meningeal Artery
Published online: 2021-08-03 THIEME Review Article | Artigo de Revisão Anatomy of the Middle Meningeal Artery Anatomia da artéria meníngea média Marco Aurélio Ferrari Sant’Anna1 Leonardo Luca Luciano2 Pedro Henrique Silveira Chaves3 Leticia Adrielle dos Santos4 Rafaela Gonçalves Moreira5 Rian Peixoto6 Ronald Barcellos7,8 Geraldo Avila Reis7,8 Carlos Umberto Pereira8 Nícollas Nunes Rabelo9 1 Hospital Celso Pierro, Pontifícia Universidade Católica de Address for correspondence Nicollas Nunes Rabelo, MD, Department Campinas, Campinas, SP, Brazil of Neurosurgery, Faculdade Atenas, Passos, Minas Gerais, Rua Oscar 2 School of Medicine, Universidade Federal de Alfenas, Alfenas, MG, Cândido Monteiro, 1000, jardim Colégio de Passos, Passos, MG, Brazil 37900, Brazil (e-mail: [email protected]). 3 Centro Universitário Atenas, Paracatu, MG, Brazil 4 Universidade Federal do Sergipe, Aracaju, SE, Brazil 8 Neurosurgery Department of the Fundação de Beneficência 5 Faculdade Atenas, Passos, MG, Brazil Hospital de Cirurgia Aracaju, SE, Brazil 6 School of Medicine, Faculdade Santa Marcelina, São Paulo, SP, Brazil 9 Neurosurgery Department, Neurosurgery Service of HGUSE and 7 Neurosurgery Department of the Hospital de Urgência de Sergipe the Benefit Foundation Hospital of Surgery, Aracaju, SE, Brazil Governador João Alves Filho, Aracaju, SE, Brazil 10Department of Neurosurgery, Faculdade Atenas, Passos, MG, Brazil Arq Bras Neurocir Abstract Introduction The middle meningeal artery (MMA) is an important artery in neuro- surgery. As the largest branch of the maxillary artery, it provides nutrition to the meninges and to the frontal and parietal regions. Diseases, including dural arteriove- nous fistula (DAVF), pseudoaneurysm, true aneurysm, traumatic arteriovenous fistula (TAVF), Moya-Moya disease (MMD), recurrent chronic subdural hematoma (CSDH), migraine, and meningioma, may be related to the MMA. -

Anatomic and Angiographic Analyses of Ophthalmic Artery Collaterals in Moyamoya Disease
Published April 12, 2018 as 10.3174/ajnr.A5622 ORIGINAL RESEARCH EXTRACRANIAL VASCULAR Anatomic and Angiographic Analyses of Ophthalmic Artery Collaterals in Moyamoya Disease X T. Robert, X G. Ciccio`, X P. Sylvestre, X A. Chiappini, X A.G. Weil, X S. Smajda, X C. Chaalala, X R. Blanc, X M. Reinert, X M. Piotin, and X M.W. Bojanowski ABSTRACT BACKGROUND AND PURPOSE: Moyamoya disease is a progressive neurovascular pathology defined by steno-occlusive disease of the distal internal carotid artery and associated with the development of compensatory vascular collaterals. The etiology and exact anatomy of vascular collaterals have not been extensively studied. The aim of this study was to describe the anatomy of collaterals developed between the ophthalmic artery and the anterior cerebral artery in a Moyamoya population. MATERIALS AND METHODS: All patients treated for Moyamoya disease from 2004 to 2016 in 4 neurosurgical centers with available cerebral digital subtraction angiography were included. Sixty-three cases were evaluated, and only 38 met the inclusion criteria. Two patients had a unilateral cervical internal carotid occlusion that limited analysis of ophthalmic artery collaterals to one hemisphere. This study is consequently based on the analysis of 74 cerebral hemispheres. RESULTS: Thirty-eight patients fulfilled the inclusion criteria. The most frequently encountered anastomosis between the ophthalmic artery and cerebral artery was a branch of the anterior ethmoidal artery (31.1%, 23 hemispheres). In case of proximal stenosis of the anterior cerebral artery, a collateral from the posterior ethmoidal artery could be visualized (16 hemispheres, 21.6%). One case (1.4%) of anastomosis between the lacrimal artery and the middle meningeal artery that permitted the vascularization of a middle cerebral artery territory was also noted. -

Microsurgical Anatomy of the Dural Arteries
ANATOMIC REPORT MICROSURGICAL ANATOMY OF THE DURAL ARTERIES Carolina Martins, M.D. OBJECTIVE: The objective was to examine the microsurgical anatomy basic to the Department of Neurological microsurgical and endovascular management of lesions involving the dural arteries. Surgery, University of Florida, Gainesville, Florida METHODS: Adult cadaveric heads and skulls were examined using the magnification provided by the surgical microscope to define the origin, course, and distribution of Alexandre Yasuda, M.D. the individual dural arteries. Department of Neurological RESULTS: The pattern of arterial supply of the dura covering the cranial base is more Surgery, University of Florida, complex than over the cerebral convexity. The internal carotid system supplies the Gainesville, Florida midline dura of the anterior and middle fossae and the anterior limit of the posterior Alvaro Campero, M.D. fossa; the external carotid system supplies the lateral segment of the three cranial Department of Neurological fossae; and the vertebrobasilar system supplies the midline structures of the posterior Surgery, University of Florida, fossa and the area of the foramen magnum. Dural territories often have overlapping Gainesville, Florida supply from several sources. Areas supplied from several overlapping sources are the parasellar dura, tentorium, and falx. The tentorium and falx also receive a contribution Arthur J. Ulm, M.D. from the cerebral arteries, making these structures an anastomotic pathway between Department of Neurological Surgery, University of Florida, the dural and parenchymal arteries. A reciprocal relationship, in which the territories Gainesville, Florida of one artery expand if the adjacent arteries are small, is common. CONCLUSION: The carotid and vertebrobasilar arterial systems give rise to multiple Necmettin Tanriover, M.D. -

Unusual Origin and Relations of the Accessory Meningeal Artery – a Case Report
Int. J. Morphol., 35(4):1348-1350, 2017. Unusual Origin and Relations of the Accessory Meningeal Artery – A Case Report Origen Inusual y Relaciones de la Arteria Meníngea Accesoria - Reporte de un Caso Prakashchandra Shetty; Melanie Rose D’Souza & Satheesha Nayak B. SHETTY, P.; D’SOUZA, M. R. & NAYAK, S. B. Unusual origin and relations of the accessory meningeal artery – A case report. Int. J. Morphol., 35(4):1348-1350, 2017. SUMMARY: Accessory meningeal artery is a branch of the first part of the maxillary artery. It supplies the structures in the infratemporal fossa and the dura mater in the middle cranial fossa. Accessory meningeal artery arose from the middle meningeal artery, 25 mm below the base of the skull and entered the middle cranial fossa through the foramen ovale. The two roots of the auriculotemporal nerve looped around it. The knowledge of the variant origin and relations may be useful during the surgeries of the infratemporal fossa. It might also be useful to the radiologists. KEY WORDS: Accessory meningeal artery; Maxillary artery; Middle meningeal artery; Infratemporal fossa. INTRODUCTION Accessory meningeal artery is a branch of first part root. The main trunk of the auriculotemporal nerve passed of the maxillary artery. However, it might also arise from backwards, deep to the middle meningeal artery. Since the the middle meningeal artery in a few cases. Though the artery originated just below the skull, it did not supply the name is accessory meningeal artery, it predominantly structures in the infratemporal fossa. It predominantly supplies the muscles, and nerves of the infratemporal fossa. -

Rhesus Monkey with Emphasis on the External Carotid System '
The Arterial System of the Head and Neck of the Rhesus Monkey with Emphasis on the External Carotid System ' WALTER A. CASTELLI AND DONALD F. HUELKE Department of Anatomy, The University of Michigan, Ann Arbor, Michigan ABSTRACT The arterial plan of the head and neck of 64 immature rhesus mon- keys (Macacn mulatta) was studied using four techniques - dissection, corrosion preparations, cleared specimens, and angiographs. In general, the arterial plan of this area in the monkey is similar to that of man. However, certain outstanding differ- ences were noted. The origin, course, and distribution of all arteries is described as well as the vascular relations to pertinent structures. As has been mentioned previously 10% formalin except 17 which were un- (Dyrud, '44; Schwartz and Huelke, '63) embalmed. Four different techniques were the rhesus monkey is useful for many used for the study of the arterial distribu- types of medical and dental investigations, tion : ( 1 ) dissections - 27 specimens; (2) yet its detailed gross morphology is virtu- corrosion preparations - 6; (3) cleared ally unknown. Although certain areas of specimens - 15; (4) angiographs - 16 the monkey have been studied in detail - heads ( 11 unembalmed and 5 embalmed). brachial plexus, facial and masticatory The arterial system of the specimens used musculature, subclavian, axillary and cor- for dissection was injected with vinyl ace- onary arteries, orbital vasculature, and tate, red latex, or with a red-colored gela- other structures (Schwartz and Huelke, tion mass. For the dissection of smaller ar- '63; Chase and DeGaris, '40; DeGaris and teries, the smallest of 150 ~1 in diameter, Glidden, '38; Chase, '38; Huber, '25; Wein- the binocular dissection microscope was stein and Hedges, '62; Samuel and War- used. -

Classification of the Ophthalmic Artery That Arises from the Middle Meningeal Artery in Japanese Adults
Okajimas Folia Anat. Jpn., 72(2-3): 163-176, August, 1995 Classification of the Ophthalmic Artery that Arises from the Middle Meningeal Artery in Japanese Adults By Kazuyuki SHIMADA, Yasumi KANEKO, Iwao SATO, Hiromitsu EZURE and Gen MURAKAMI Department of Anatomy, Showa University, School of Medicine, Tokyo, Japan Department of Anatomy, Nippon Dental University, School of Dentistry at Tokyo, Tokyo, Japan Department of Anatomy, Sapporo Medical University, School of Medicine, Sapporo, Japan -Received for Publication, July 4, 1995- Key Words: Gross anatomy, Middle meningeal artery, Orbital branch, Meningo-orbital foramen Summary: In a study of Japanese adults, we found that the orbital branch (OB) passing through the superior orbital fissure frequently anastomosed with the lacrimal artery or the ophthalmic artery (12/20). However, the OB passing through the meningo-orbital foramen (mof) only associationaly anastomosed with branches of the ophthalmic artery (4/79). Further- more, the OB in the orbit, excluding the lacrimal gland as previously reported. We examined 116 cases in which the OB passed through the mof in 129 adult Japanese cadavers (45.0% in 258 sides). The OB passing through the mof was always distributed to the periorbital region and the area that it supplied was limited to the periorbita in about half of those cases. In another half of the cases (58/116), the area supplied included the lacrimal gland. The ophthalmic artery in the orbital branch arising cadavers (74 males and 55 females) to determine the from the middle meningeal artery has been described course of the orbital branch and the nerve of the previously (Zuckerkandl, 1876; Meyer, 1887; Lang supply to the orbital area from the middle meningeal and Wachsmuth, 1979; Hollinshead, 1982). -
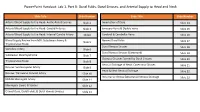
Powerpoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck
PowerPoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck Slide Title Slide Number Slide Title Slide Number Arterial Blood Supply to the Head: Aortic Arch Branches Slide 2 Innervation of Dura Slide 14 Arterial Blood Supply to the Head: Carotid Arteries Slide 3 Emissary Veins & Diploic Veins Slide 15 Arterial Blood Supply to the Head: Internal Carotid Artery Slide4 Cerebral & Cerebellar Veins Slide 16 Blood Supply Review from MSI: Subclavian Artery & Named Dural Folds Slide 5 Slide 17 Thyrocervical Trunk Dural Venous Sinuses Slide 18 Vertebral Artery Slide 6 Dural Venous Sinuses (Continued) Slide 19 Subclavian Steal Syndrome Slide 7 Osseous Grooves formed by Dural Sinuses Slide 20 Thyrocervical Trunk Slide 8 Venous Drainage of Head: Cavernous Sinuses Slide 21 Review: Suprascapular Artery Slide 9 Head & Neck Venous Drainage Slide 22 Review: Transverse Cervical Artery Slide 10 Intracranial Versus EXtracranial Venous Drainage Slide 23 Middle Meningeal Artery Slide 11 Meningeal Layers & Spaces Slide 12 Cranial Dura, Dural Folds, & Dural Venous Sinuses Slide 13 Arterial Blood Supply to the Head: Aortic Arch Branches The head and neck receive their blood supply from https://3d4medic.al/PXGmbxEt branches of the right and left common carotid and right and left subclavian arteries. • On the right side, the subclavian and common carotid arteries arise from the brachiocephalic trunk. • On the left side, these two arteries originate from the arch of the aorta. Arterial Blood Supply to the Head: Carotid Arteries On each side of the neck, the common carotid arteries ascend in the neck to the upper border of the thyroid cartilage (vertebral level C3/C4) where they divide into eXternal and internal carotid arteries at the carotid bifurcation.