7 Congenital and Developmental Abnormalities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Saethre-Chotzen Syndrome
Saethre-Chotzen syndrome Authors: Professor L. Clauser1 and Doctor M. Galié Creation Date: June 2002 Update: July 2004 Scientific Editor: Professor Raoul CM. Hennekam 1Department of craniomaxillofacial surgery, St. Anna Hospital and University, Corso Giovecca, 203, 44100 Ferrara, Italy. [email protected] Abstract Keywords Disease name and synonyms Excluded diseases Definition Prevalence Management including treatment Etiology Diagnostic methods Genetic counseling Antenatal diagnosis Unresolved questions References Abstract Saethre-Chotzen Syndrome (SCS) is an inherited craniosynostotic condition, with both premature fusion of cranial sutures (craniostenosis) and limb abnormalities. The most common clinical features, present in more than a third of patients, consist of coronal synostosis, brachycephaly, low frontal hairline, facial asymmetry, hypertelorism, broad halluces, and clinodactyly. The estimated birth incidence is 1/25,000 to 1/50,000 but because the phenotype can be very mild, the entity is likely to be underdiagnosed. SCS is inherited as an autosomal dominant trait with a high penetrance and variable expression. The TWIST gene located at chromosome 7p21-p22, is responsible for SCS and encodes a transcription factor regulating head mesenchyme cell development during cranial tube formation. Some patients with an overlapping SCS phenotype have mutations in the FGFR3 (fibroblast growth factor receptor 3) gene; especially the Pro250Arg mutation in FGFR3 (Muenke syndrome) can resemble SCS to a great extent. Significant intrafamilial -

Non-Cardiac Manifestations of Marfan Syndrome
Keynote Lecture Series Non-cardiac manifestations of Marfan syndrome Anne H. Child Molecular and Clinical Sciences Research Institute, St George’s University of London, Cranmer Terrace, London, UK Correspondence to: Dr. Anne H. Child, MD, FRCP. Reader in Cardiovascular Genetics, Molecular and Clinical Sciences Research Institute, St George's University of London, Cranmer Terrace, London SW17 0RE, UK. Email: [email protected]. Because of the widespread distribution of fibrillin 1 in the body, Marfan syndrome (MFS) affects virtually every system. The expression of this single dominantly inherited gene is variable within a family, and between families. There is some genotype-phenotype correlation which is helpful in guiding long-term prognosis, and management. In general gene mutations have been reported in clusters, with those having mainly ocular manifestations occurring in exons 1 to 15 of this 65-exon gene; those causing cardiac problems often involving cysteine replacement in a calcium binding EGF-like sequence; the most severe mutations occurring in exons 25–32, causing neonatal MFS diagnosed at birth, and severe enough to cause death frequently before the age of 2. Other correlations will certainly be found in future. This condition is progressive, and the manifestations unfold according to age. For example, if the lens is going to dislocate this usually occurs by age 10; scoliosis usually presents itself between the ages of 8 and 15; height should be monitored carefully between the onset of puberty and cessation of growth approximately age 17 or 18. Holistic care should be offered by one doctor who oversees the patient’s welfare. This should be a paediatrician, paediatric cardiologist, or general practitioner in the case of an affected child. -
Surgical Challenges in Complex Primary Total Hip Arthroplasty
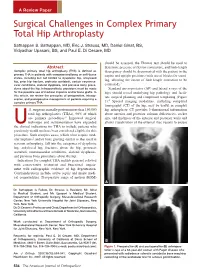
A Review Paper Surgical Challenges in Complex Primary Total Hip Arthroplasty Sathappan S. Sathappan, MD, Eric J. Strauss, MD, Daniel Ginat, BS, Vidyadhar Upasani, BS, and Paul E. Di Cesare, MD should be assessed, the Thomas test should be used to Abstract determine presence of flexion contracture, and limb-length Complex primary total hip arthroplasty (THA) is defined as discrepancy should be documented with the patient in the primary THA in patients with compromised bony or soft-tissue supine and upright positions (with use of blocks for stand- states, including but not limited to dysplastic hip, ankylosed hip, prior hip fracture, protrusio acetabuli, certain neuromus- ing, allowing the extent of limb-length correction to be 3 cular conditions, skeletal dysplasia, and previous bony proce- estimated). dures about the hip. Intraoperatively, provisions must be made Standard anteroposterior (AP) and lateral x-rays of the for the possible use of modular implants and/or bone grafts. In hips should reveal underlying hip pathology and facili- this article, we review the principles of preoperative, intraop- tate surgical planning and component templating (Figure erative, and postoperative management of patients requiring a 4 complex primary THA. 1). Special imaging modalities, including computed tomography (CT) of the hip, may be useful in complex .S. surgeons annually perform more than 150,000 hip arthroplasty. CT provides 3-dimensional information total hip arthroplasties (THAs), 90% of which about anterior and posterior column deficiencies, socket are primary procedures.1 Improved surgical size, and thickness of the anterior and posterior walls and technique and instrumentation have expanded allows visualization of the external iliac vessels to ensure Uthe clinical indications for THA to include patients who previously would not have been considered eligible for this procedure. -

Peds Ortho: What Is Normal, What Is Not, and When to Refer
Peds Ortho: What is normal, what is not, and when to refer Future of Pedatrics June 10, 2015 Matthew E. Oetgen Benjamin D. Martin Division of Orthopaedic Surgery AGENDA • Definitions • Lower Extremity Deformity • Spinal Alignment • Back Pain LOWER EXTREMITY ALIGNMENT DEFINITIONS coxa = hip genu = knee cubitus = elbow pes = foot varus valgus “bow-legged” “knock-knee” apex away from midline apex toward midline normal varus hip (coxa vara) varus humerus valgus ankle valgus hip (coxa valga) Genu varum (bow-legged) Genu valgum (knock knee) bow legs and in toeing often together Normal Limb alignment NORMAL < 2 yo physiologic = reassurance, reevaluate @ 2 yo Bow legged 7° knock knee normal Knock knee physiologic = reassurance, reevaluate in future 4 yo abnormal 10 13 yo abnormal + pain 11 Follow-up is essential! 12 Intoeing 1. Femoral anteversion 2. Tibial torsion 3. Metatarsus adductus MOST LIKELY PHYSIOLOGIC AND WILL RESOLVE! BRACES ARE HISTORY! Femoral Anteversion “W” sitters Internal rotation >> External rotation knee caps point in MOST LIKELY PHYSIOLOGIC AND MAY RESOLVE! Internal Tibial Torsion Thigh foot angle MOST LIKELY PHYSIOLOGIC AND WILL RESOLVE BY SCHOOL AGE Foot is rotated inward Internal Tibial Torsion (Fuchs 1996) Metatarsus Adductus • Flexible = correctible • Observe vs. casting CURVED LATERAL BORDER toes point in NOT TO BE CONFUSED WITH… Clubfoot talipes equinovarus adductus internal varus rotation equinus CAN’T DORSIFLEX cavus Clubfoot START19 CASTING JUST AFTER BIRTH Calcaneovalgus Foot • Intrauterine positioning • Resolve -

SKELETAL DYSPLASIA Dr Vasu Pai
SKELETAL DYSPLASIA Dr Vasu Pai Skeletal dysplasia are the result of a defective growth and development of the skeleton. Dysplastic conditions are suspected on the basis of abnormal stature, disproportion, dysmorphism, or deformity. Diagnosis requires Simple measurement of height and calculation of proportionality [<60 inches: consideration of dysplasia is appropriate] Dysmorphic features of the face, hands, feet or deformity A complete physical examination Radiographs: Extremities and spine, skull, Pelvis, Hand Genetics: the risk of the recurrence of the condition in the family; Family evaluation. Dwarf: Proportional: constitutional or endocrine or malnutrition Disproportion [Trunk: Extremity] a. Height < 42” Diastrophic Dwarfism < 48” Achondroplasia 52” Hypochondroplasia b. Trunk-extremity ratio May have a normal trunk and short limbs (achondroplasia), Short trunk and limbs of normal length (e.g., spondylo-epiphyseal dysplasia tarda) Long trunk and long limbs (e.g., Marfan’s syndrome). c. Limb-segment ratio Normal: Radius-Humerus ratio 75% Tibia-Femur 82% Rhizomelia [short proximal segments as in Achondroplastics] Mesomelia: Dynschondrosteosis] Acromelia [short hands and feet] RUBIN CLASSIFICATION 1. Hypoplastic epiphysis ACHONDROPLASTIC Autosomal Dominant: 80%; 0.5-1.5/10000 births Most common disproportionate dwarfism. Prenatal diagnosis: 18 weeks by measuring femoral and humeral lengths. Abnormal endochondral bone formation: zone of hypertrophy. Gene defect FGFR fibroblast growth factor receptor 3 . chromosome 4 Rhizomelic pattern, with the humerus and femur affected more than the distal extremities; Facies: Frontal bossing; Macrocephaly; Saddle nose Maxillary hypoplasia, Mandibular prognathism Spine: Lumbar lordosis and Thoracolumbar kyphosis Progressive genu varum and coxa valga Wedge shaped gaps between 3rd and 4th fingers (trident hands) Trident hand 50%, joint laxity Pathology Lack of columnation Bony plate from lack of growth Disorganized metaphysis Orthopaedics 1. -

Thieme: Teaching Atlas of Musculoskeletal Imaging
Teaching Atlas of Musculoskeletal Imaging Teaching Atlas of Musculoskeletal Imaging Peter L. Munk, M.D., C.M., F.R.C.P.C. Professor Departments of Radiology and Orthopaedics University of British Columbia Head Section of Musculoskeletal Radiology Vancouver General Hospital and Health Science Center Vancouver, British Columbia, Canada Anthony G. Ryan, M.B., B.C.H., B.A.O., F.R.C.S.I., M.Sc. (Engineering and Physical Sciences in Medicine), D.I.C., F.R.C.R., F.F.R.R.C.S.I. Consultant Musculoskeletal and Interventional Radiologist Waterford Regional Teaching Hospital Ardkeen, Waterford City, Republic of Ireland Radiologic Tutor and Clinical Instructor in Radiology The Royal College of Surgeons in Ireland Dublin, Republic of Ireland Thieme New York • Stuttgart [email protected] 66485438-66485457 Thieme Medical Publishers, Inc. 333 Seventh Ave. New York, NY 10001 Editor: Birgitta Brandenburg Assistant Editor: Ivy Ip Vice President, Production and Electronic Publishing: Anne T. Vinnicombe Production Editor: Print Matters, Inc. Vice President, International Marketing: Cornelia Schulze Sales Director: Ross Lumpkin Chief Financial Officer: Peter van Woerden President: Brian D. Scanlan Compositor: Compset, Inc. Printer: The Maple-Vail Book Manufacturing Group Library of Congress Cataloging-in-Publication Data Munk, Peter L. Teaching atlas of musculoskeletal imaging / Peter L. Munk, Anthony G. Ryan. p. ; cm. Includes bibliographical references and index. ISBN-13: 978-1-58890-372-3 (alk. paper) ISBN-10: 1-58890-372-9 (alk. paper) ISBN-13: 978-3-13-141981-1 (alk. paper) ISBN-10: 3-13-141981-4 (alk. paper) 1. Musculoskeletal system—Diseases—Imaging—Atlases. 2. Musculoskeletal system—Diseases—Case studies. -

Arthrogryposis Multiplex Congenita Part 1: Clinical and Electromyographic Aspects
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.35.4.425 on 1 August 1972. Downloaded from Journal ofNeurology, Neurosurgery, anid Psychiatry, 1972, 35, 425-434 Arthrogryposis multiplex congenita Part 1: Clinical and electromyographic aspects E. P. BHARUCHA, S. S. PANDYA, AND DARAB K. DASTUR From the Children's Orthopaedic Hospital, and the Neuropathology Unit, J.J. Group of Hospitals, Bombay-8, India SUMMARY Sixteen cases with arthrogryposis multiplex congenita were examined clinically and electromyographically; three of them were re-examined later. Joint deformities were present in all extremities in 13 of the cases; in eight there was some degree of mental retardation. In two cases, there was clinical and electromyographic evidence of a myopathic disorder. In the majority, the appearances of the shoulder-neck region suggested a developmental defect. At the same time, selective weakness of muscles innervated by C5-C6 segments suggested a neuropathic disturbance. EMG revealed, in eight of 13 cases, clear evidence of denervation of muscles, but without any regenerative activity. The non-progressive nature of this disorder and capacity for improvement in muscle bulk and power suggest that denervation alone cannot explain the process. Re-examination of three patients after two to three years revealed persistence of the major deformities and muscle Protected by copyright. weakness noted earlier, with no appreciable deterioration. Otto (1841) appears to have been the first to ventricles, have been described (Adams, Denny- recognize this condition. Decades later, Magnus Brown, and Pearson, 1953; Fowler, 1959), in (1903) described it as multiple congenital con- addition to the spinal cord changes. -

Bilateral Both Bone Leg Fracture in a Case of Hereditary Multiple Exostoses with Bilateral Proximal and Distal Tibiofibular Synostosis
JMSCR Volume||2 ||Issue||5||Pages 1054-1058||May 2014 2014 www.jmscr.igmpublication.org Impact Factor-1.1147 ISSN (e)-2347-176x Bilateral Both Bone Leg Fracture in a Case of Hereditary Multiple Exostoses with Bilateral Proximal and Distal Tibiofibular Synostosis Authors Ganesh Singh1, Anshuman Vijay Roy2, Shailendra Singh Bhandari3, Pankaj Singh4 Author / Corresponding author Dr . Ganesh Singh M.S. (Orthopaedics) Assistant Professor , Department of Orthopaedics Room # 25 , New Resident Hostel , Medical Campus Government Medical College , Haldwani ( Uttarakhand ) . PIN -263139 Mobile no – 91-9319616456 , E mail – [email protected] Co –Authors Dr . Anshuman Vijay Roy M.S. (Orthopaedics ) Assistant Professor , Department of Orthopaedics Government Medical College , Haldwani ( Uttarakhand ). PIN – 263139 Mobile no. – 91-9927973777 E mail - [email protected] Dr Shailendra Singh Bhandari M.S.(Orthopaedics) Associatet Professor , Department of Orthopaedics Government Medical College , Haldwani ( Uttarakhand ). PIN – 263139 Mobile no. – 91-9837251168 E mail – [email protected] Dr . Pankaj Singh M.S. (Orthopaedics ) Professor , Department ofOrthopaedics Government Medical College , Haldwani ( Uttarakhand ). PIN – 263139 Mobile no. – 91-9927973777 E mail – [email protected] Ganesh Singh et al JMSCR Volume 2 Issue 5 May 2014 Page 1054 JMSCR Volume||2 ||Issue||5||Pages 1054-1058||May 2014 2014 Abstract The Hereditary Multiple Exostoses ( HME) is a neoplastic disorder affecting multiple skeletal sites in the form of bony protuberances of varying sizes and shapes . The clinical features are site specific and mostly relate to the effect of swelling on the adjacent tissues . Associated abnormalities like bowing deformities of bones, shortening and mechanical axes deviations may lead to increased risk of stresses over the bones . -

Mackenzie's Mission Gene & Condition List
Mackenzie’s Mission Gene & Condition List What conditions are being screened for in Mackenzie’s Mission? Genetic carrier screening offered through this research study has been carefully developed. It is focused on providing people with information about their chance of having children with a severe genetic condition occurring in childhood. The screening is designed to provide genetic information that is relevant and useful, and to minimise uncertain and unclear information. How the conditions and genes are selected The Mackenzie’s Mission reproductive genetic carrier screen currently includes approximately 1300 genes which are associated with about 750 conditions. The reason there are fewer conditions than genes is that some genetic conditions can be caused by changes in more than one gene. The gene list is reviewed regularly. To select the conditions and genes to be screened, a committee comprised of experts in genetics and screening was established including: clinical geneticists, genetic scientists, a genetic pathologist, genetic counsellors, an ethicist and a parent of a child with a genetic condition. The following criteria were developed and are used to select the genes to be included: • Screening the gene is technically possible using currently available technology • The gene is known to cause a genetic condition • The condition affects people in childhood • The condition has a serious impact on a person’s quality of life and/or is life-limiting o For many of the conditions there is no treatment or the treatment is very burdensome for the child and their family. For some conditions very early diagnosis and treatment can make a difference for the child. -

Health Supervision for Children with Marfan Syndrome Abstract
FROM THE AMERICAN ACADEMY OF PEDIATRICS Guidance for the Clinician in Rendering Pediatric Care CLINICAL REPORT Health Supervision for Children With Marfan Syndrome Brad T. Tinkle, MD, PhD, Howard M. Saal, MD, and the COMMITTEE ON GENETICS abstract KEY WORD Marfan syndrome is a systemic, heritable connective tissue disorder Marfan syndrome that affects many different organ systems and is best managed by us- This document is copyrighted and is property of the American ing a multidisciplinary approach. The guidance in this report is Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American designed to assist the pediatrician in recognizing the features of Mar- Academy of Pediatrics. Any conflicts have been resolved through fan syndrome as well as caring for the individual with this disorder. a process approved by the Board of Directors. The American Pediatrics 2013;132:e1059–e1072 Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication. The guidance in this report does not indicate an exclusive INTRODUCTION course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be Marfan syndrome is a heritable, multisystem disorder of connective appropriate. tissue with extensive clinical variability. It is a relatively common condition, with approximately 1 in 5000 people affected.1 Cardinal features involve the ocular, musculoskeletal, and cardiovascular systems. Because of the high degree of variability of this disorder, many of these clinical features can be present at birth or can man- ifest later in childhood or even adulthood. -

Cementless Surgical Technique
Surgical Technique Comprehensive. Simple. Efficient. It’s easy to understand why SYNERGY Hip System is one of orthopaedics’ great success stories. Its rapid adoption by surgeons has been due to the system’s significant advances over previous tapered implants, including its unique stem geometry, choice of surface treatments, innovative neck design, true dual offsets and efficient, easy-to-use instrumentation. The SYNERGY Hip System also provides the surgeon a choice of cementless, cemented and fracture management systems that use the same 2 trays of instrumentation. In addition, the cementless system offers the valuable options of a porous stem, a hydroxyapatite (HA) stem, an HA porous stem and a titanium press-fit stem. 2 SYNERGY Cementless Stem Surgical technique completed in conjunction with: Robert B. Bourne, MD, FRCS(C) London, Ontario, Canada Professor Ernesto DeSantis Rome, Italy Wayne M. Goldstein, MD Chicago, Illinois Gianni L. Maistrelli, MD, FRCS(C) Toronto, Ontario, Canada John W. McCutchen, MD Orlando, Florida Cecil H. Rorabeck, MD, FRCS(C) London, Ontario, Canada James P. Waddell, MD Toronto, Ontario, Canada Nota Bene: The technique description herein is made available to the healthcare professional to illustrate the authors’ suggested treatment for the uncomplicated procedure. In the final analysis, the preferred treatment is that which addresses the needs of the patient. 3 SYNERGY Cementless Stem Introduction The SYNERGY Tapered Hip System capitalizes on the excellent clinical results of proximal to distal tapered stem designs. The SYNERGY system features a variety of stem designs that provide different methods of stem fixation and that also address different patient demand types. All of the stems in the SYNERGY system are implanted with 1 simple set of surgical instruments. -

A Total Hip Replacement Toolbox: from CT-Scan to Patient-Specific
A Total Hip Replacement Toolbox: From CT-Scan to Patient-Specific FE Analysis Diogo Moreira Campos Ferreira de Almeida Promotors: Prof B. Verhegghe, PhD, Prof M. De Beule, PhD Prof J. Folgado, PhD, Prof R. Ruben, PhD Doctoral thesis submitted in order to obtain the academic degrees of Doctor of Biomedical Engineering (Ghent University) and Doutor em Engenharia Biomédica (Universidade de Lisboa) Department of Electronics and Information Systems Head of Department: Prof R. Van de Walle, PhD Faculty of Engineering and Architecture Department of Bioengineering Head of Department: Prof J. P. Conde, PhD Instituto Superior Técnico Academic year 2016 - 2017 ISBN 978-90-8578-980-2 NUR 954 Wettelijk depot: D/2017/10.500/15 Supervisors: Prof. dr. ir. Rui B. Ruben Prof. dr. ir. Benedict Verhegghe Prof. dr. ir. Jo~aoFolgado Prof. dr. ir. Matthieu de Beule Research institutions: Institute Biomedical Technology Biofluid, Tissue and Solid Mechanics for Medical Applications (bioMMeda) Ghent University De Pintelaan 185 - Blok B B{9000 Gent Belgium Institute of Mechanical Engineering (IDMEC-IST) Associated Laboratory for Energy,Transports and Aeronautics (laeta) University of Lisbon Av. Rovisco Pais, 1 1049-001 Lisbon Portugal Members of the exam committee: Chairman: Prof. dr. ir. Rik Van de Walle Faculty of Engineering and Architecture, UGent, Belgium Secretaries: Prof. dr. ir. Jan Belis Faculty of Engineering and Architecture, UGent, Belgium Prof. dr. ir. Paulo Rui Fernandes Instituto Superior T´ecnico, ULisbon, Portugal Other members: Dr. ir. Toon Huysmans Department of Physics, Universiteit Antwerpen, Belgium Prof. dr. ir. Jef Vandemeulebroucke Department of Electronics and Informatics, Vrije Universiteit Brussel, Belgium Prof.