Biomechanical Modeling of Paralympic Wheelchair
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

24 August Opening Ceremony
Paralympic Education Program Presented by Tracking the Tokyo 2020 Paralympic Games As you watch the Tokyo 2020 Paralympic Games, fill out the following information to help keep track of the amazing achievements of our Paralympians. 24 August Opening Ceremony Draw or write about your favourite moment from the Tokyo 2020 Paralympic Games Opening Ceremony. 25 August The team sports – Goalball, Wheelchair Basketball and Wheelchair Rugby started today! How did the Australian teams go? Goalball Australia vs Final score Wheelchair Basketball Australia vs Final score Wheelchair Rugby Australia vs Final score 26 August Who was Australia’s first medal winner? What colour medal did they win and for which event? Name Sport Event Place 1st 2nd 3rd 27 August Swimming is in full swing! Who are two athletes who have won medals for swimming? Name Event Place 1st 2nd 3rd Name It’s medal tally check Event time!! Place 1st 2nd 3rd 28 August Medal tally check! How many gold, silver and bronze medals has Australia won and what rank are they on the overall medal tally? Gold Silver Bronze Rank AUS 29 August Find out some information about one of the following sports and complete a sport profile: Boccia Table Tennis Shooting Rowing Sport name How many Australian athletes are competing in Tokyo? How many medals has Australia 1st 2nd 3rd won in this sport so far? What kinds of impairments do the athletes have in this sport? What is the name of one of the Australian athletes in this sport? When did they first compete for Australia? What is one achievement they have accomplished in their sporting career? 30 August Let’s check on our team sports! Goalball and Wheelchair Basketball are still competing. -
Disability Is the State Pupils May Find Themselves in When the Adjustments Needed to Overcome Their Impairments Don’T Happen
Supporting Secondary Pupils with Physical Disabilities in P.E Disability is the state pupils may find themselves in when the adjustments needed to overcome their impairments don’t happen. (extracted from Games All Children Can Play published by Scope) SEND 0-25 SERVICE Specialist Inclusion Support Service AS MY P.E TEACHER CAN YOU…? Ask me what I like to do in P.E, (in some cases this may mean- both before and after with regards to a medical procedure or an For further infor- mation accident and ask my parents too). please contact :- Don’t be afraid to ask me for ideas on how I can be included. Clare Hope or Jo Walker Always make me feel involved and do not leave me sat on the side -lines, feeling left out or excluded. Sensory and Physical Disabilities Team Try to include as many activities as possible i.e. sports that can be adapted, like basketball or table tennis so I am able to partici- Specialist Inclusion Support Service pate with other pupils. Do a normal P.E lesson, but always adapt it so I can take part. Do Elmwood Place it in such a way that it is not obvious and everyone in the class gets something out of it. 37 Burtons Way If you are doing a team sport or are working in a group make me a Birmingham captain. B36 0UG Be adventurous with your adaptations to an activity. As my P.E teacher, to talk to the school about what they can put in Telephone : 0121 704 6690 place to support me. -

An Investigation of Athletic Buoyancy in Adult Recreational and Sport Club Athletes
Louisiana State University LSU Digital Commons LSU Doctoral Dissertations Graduate School May 2020 An Investigation of Athletic Buoyancy in Adult Recreational and Sport Club Athletes Jackie Rae Victoriano Calhoun Louisiana State University and Agricultural and Mechanical College Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_dissertations Part of the Kinesiology Commons, Other Psychology Commons, and the Sports Studies Commons Recommended Citation Calhoun, Jackie Rae Victoriano, "An Investigation of Athletic Buoyancy in Adult Recreational and Sport Club Athletes" (2020). LSU Doctoral Dissertations. 5265. https://digitalcommons.lsu.edu/gradschool_dissertations/5265 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Doctoral Dissertations by an authorized graduate school editor of LSU Digital Commons. For more information, please [email protected]. AN INVESTIGATION OF ATHLETIC BUOYANCY IN ADULT RECREATIONAL AND SPORT CLUB ATHLETES A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Doctor of Philosophy in The School of Kinesiology by Jackie V. Calhoun B.A., Louisiana State University, 2013 M.S., Louisiana State University, 2016 August 2020 ACKNOWLEDGMENTS I would first like to thank Dr. Alex Garn for your endless patience and thoughtful guidance. I am so thankful that you were willing to hear my interests and give me the opportunity to pursue them. I will forever be grateful for the time that you spent teaching me statistics and research methods, and for the support you provided me through my entire time as a graduate student. -

Sports N Spokes-July-2020.Pdf
The Magazine for Wheelchair Sports and Recreation Vol. 46 No. 4 July 2020 ADAPTIVE TRAINING Athletes modify workouts during pandemic MIND GAMES Adjusting to Paralympic postponement En Garde! The art of wheelchair fencing Inside SPORTS ’N SPOKES Features 16 Mental Shift Following the postponement of the 2020 Tokyo Paralympics until 2021 because of the novel coronavirus (COVID-19) pandemic, some hopeful athletes have had to refocus. by Shelly Anderson 22 Parafencing Prowess Team USA Parafencers say there’s an art to the sport — which involves blades, instinct and timing. As they prepare for the Tokyo Paralympics, they want to get others involved, too. by Jonathan Gold 28 Staying Strong With the novel coronavirus (COVID-19) pandemic shutting sports events and gyms down across the country, some Paralympians found ways to adapt and still practice their training — albeit differently. by John Groth 28 on sportsnspokes.com Scan This! Digital Highlights Or go to JUNIOR ATHLETE OF THE YEAR WHEELCHAIR SOFTBALL TOURNEY sportsnspokes.com SPORTS ’N SPOKES will announce The Kansas City Royals Wheelchair Softball Club is hosting a its Junior Athlete of the Year wheelchair softball tournament July 11 at Pleasant Valley Park in award winner later this summer, Kansas City, Mo., and SPORTS ’N SPOKES will be there. Interested so visit the website to find out players can sign up at softball.registerKC.com. Check out our who received the honor. Facebook page and the website for photo and video coverage. July 2020 | SPORTS ’N SPOKES 3 Inside SPORTS ’N SPOKES 6 MY OPINION Digital Change by Tom Fjerstad 14 THE EXTRA POINT Making A Major Move by John Groth 33 PEOPLE You Can Still Be An Athlete by Bill Huber 16 36 OUTDOORS Working Outside The Box by Shelly Anderson Also in This Issue 8 In The Game 13 Spokes Stars 27 Sports Associations 38 On The Sidelines 41 Classifieds 41 ProShop 42 Final Frame 22 On the cover: Four-time SPORTS ’N SPOKES (ISSN 0161-6706). -

Coaching Manual Mark Walker
WHEELCHAIR BASKETBALL COACHING MANUAL MARK WALKER CONTENTS 1. Biography – Mark Walker .......................................... 1 2. Introduction .............................................................. 2 3. Coaching ................................................................... 3 Philosophy ................................................................ 3 The Pyramid of Success ............................................. 4 Coaching Styles ......................................................... 4 Communication ........................................................ 5 Discipline .................................................................. 5 Points of Emphasis/Don’t just run Drills .................... 5 Planning Effective Training Sessions .......................... 6 Basketball training Planning Sheet ............................ 7 Training for Peak Performance .................................. 8 Individual Players Evaluation .................................... 9 Final Thoughts .......................................................... 10 4. Classification of Athletes .......................................... 11 IWBF Guidelines ....................................................... 11-17 5. Equipment ............................................................... 18 Wheelchair Set Up ................................................... 18 Wheelchair set up and strapping by Tim Maloney .... 18 Common Sense Equipment ...................................... 19-20 6. Chair Skills .............................................................. -
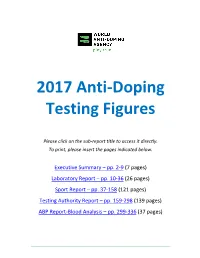
2017 Anti-Doping Testing Figures Report
2017 Anti‐Doping Testing Figures Please click on the sub‐report title to access it directly. To print, please insert the pages indicated below. Executive Summary – pp. 2‐9 (7 pages) Laboratory Report – pp. 10‐36 (26 pages) Sport Report – pp. 37‐158 (121 pages) Testing Authority Report – pp. 159‐298 (139 pages) ABP Report‐Blood Analysis – pp. 299‐336 (37 pages) ____________________________________________________________________________________ 2017 Anti‐Doping Testing Figures Executive Summary ____________________________________________________________________________________ 2017 Anti-Doping Testing Figures Samples Analyzed and Reported by Accredited Laboratories in ADAMS EXECUTIVE SUMMARY This Executive Summary is intended to assist stakeholders in navigating the data outlined within the 2017 Anti -Doping Testing Figures Report (2017 Report) and to highlight overall trends. The 2017 Report summarizes the results of all the samples WADA-accredited laboratories analyzed and reported into WADA’s Anti-Doping Administration and Management System (ADAMS) in 2017. This is the third set of global testing results since the revised World Anti-Doping Code (Code) came into effect in January 2015. The 2017 Report – which includes this Executive Summary and sub-reports by Laboratory , Sport, Testing Authority (TA) and Athlete Biological Passport (ABP) Blood Analysis – includes in- and out-of-competition urine samples; blood and ABP blood data; and, the resulting Adverse Analytical Findings (AAFs) and Atypical Findings (ATFs). REPORT HIGHLIGHTS • A analyzed: 300,565 in 2016 to 322,050 in 2017. 7.1 % increase in the overall number of samples • A de crease in the number of AAFs: 1.60% in 2016 (4,822 AAFs from 300,565 samples) to 1.43% in 2017 (4,596 AAFs from 322,050 samples). -

Wheelchair Curling
WHEELCHAIR CURLING Skill: I will push the rock as close to the center of the house Safety First as possible. Control the Delivery Stick Cognitive: I will discuss the skill components of curling. Push and Follow Through to Fitness: I will be actively engaged during the entire activity. Target Personal & Social Responsibility: I will follow all rules and etiquette of curling. Equipment: 8 rocks (bean bags) per rink 1–2 scooters per rink 8 low-profile cones per rink (4 per color to designate teams) 1 delivery stick (hockey stick, lacrosse stick, noodle) per rink 1 chair or wheelchair per rink Floor tape Set-Up: 1. Create rinks and house targets with tape/cones. 2. Use floor tape to make targets (houses) at 1 end of each rink. 3. Place a chair, delivery stick, and 8 bean bags at the opposite end of the house for each rink. 4. Create equal teams, 2 teams at each rink. Activity Procedures: 1. It’s time for Wheelchair Curling, a Paralympic event that matches Olympic Curling. The only adaptation from Olympic curling is the elimination of sweepers. 2. The objective of today’s activity is to place your team’s rock closest to the button during each end. 3. 1 student from the 1st team will sit in the chair (or wheelchair) and use the delivery stick to push the rock (scooter carrying a bean bag) toward the house. Try to get your rock closest to the button. Take turns sending scooters. When each scooter stops, the team will place a low-profile cone on the floor as a marker of the send. -
Wheelchair Delivery Strategy Sweeping Basic
learn to curl Spirit Delivery Sweeping Strategy wheelchair Stick BaSic ruleS Dare to curl Curling in the United States has experienced great growth in the past decade, thanks in great part to TV coverage during the Olympic Winter Games. Membership in the U.S. Curling Association has increased from just over 10,000 in 2002 to nearly 16,000 in 2012. USA Curling currently boasts 165 member clubs in 40 states. Many of these new curling clubs are termed “arena” clubs, meaning that the clubs are housed at facilities were multiple sports are offered as opposed to a dedicated curling rink. Having existing curling arena owners embrace curling has been another significant factor in the growth of curling in the U.S. as it brought the sport to many warmer climates in southern states where curling never was played before, including South Carolina, Georgia, Florida, Texas, and Arizona, just to name a few. Some Fun Facts about Curling: • It is generally agreed that curling was developed in Scotland in the 16th century on frozen marshes • Curling was first an Olympic medal sport in 1924, but did not obtain full medal status again until 1998 • Curling is played in 48 countries worldwide. Canada leads the way with around 1 million active curlers • The modern curling stone is round, made of granite, and weighs about 42 pounds • The first known U.S. curling clubs were located in New York City, Detroit, Milwaukee, and Portage, Wis. • Sweeping can help a stone slide up to an additional 15 feet • On average, an athlete can walk up to 2 miles in an 8-end game Brochure production is made possible through grants from the World Curling Federation and The Chicago Community Trust. -

Rules for Wheelchair Rugby – Rishi Sharma
Here are some rules and regulations of Wheelchair Rugby (there are many more but here are the important ones): 1. Everyone is given a classification based on their physical function of either 0.5, 1.0, 1.5, 2.0, 2.5, 3.0, or 3.5. This point value is determined by highly skilled physical therapists, known as classifiers, that perform a variety of manual muscle tests and observations of watching an athlete play to determine an appropriate point value. The higher the point value (3.5 being the highest and 0.5 being the lowest) the more function that player has. I am a 2.0 and I have seen other players with CMT be as high as 3.5 or as low as a 1.0. This is because CMT affects everyone differently. Players who are 45 or older or are female get an automatic 0.5 deduction. 2. Only 4 players on each team are allowed on the court at one time and the combined point value of those players on court for each team can not exceed 8 points. For instance, if all the players on court, for one of the two teams, have all their players have the same point value of 3.0 (3-point value x 4 players = 12 points on court which exceeds the 8 points allowed) this is considered an illegal lineup and will result in the team forfeiting the game. This rule is there to make sure all players get a chance to play. 3. Left: Offensive Chair | Right: Defensive Chair There are two types of chairs used to play this game. -

Inclusion Case Studies Designed by Iain Sangster Examples of Inclusive Practice That Supports Children, Players and Athletes to Become Involved in Sport
Inclusion case studies Designed by Iain Sangster Examples of inclusive practice that supports children, players and athletes to become involved in sport Putting sport first Photography: Rob Eyton-Jones; David McIntyre; Scottish Disability Sport Photography: Rob Eyton-Jones; David McIntyre; Contents Introduction and acknowledgements Introduction and acknowledgements .................p3 The case studies set out in this document have been collated by sportscotland – the national agency for sport – and have been written by Scottish Disability Sport and a number of local and national partners Inclusion within Active Schools ..........................p4 across the country. Inclusive facilities for world class athletes ...........p6 We would like to acknowledge the input of the following organisations for their energy, time and Inclusive coaching .............................................p8 commitment in highlighting these best practice examples around inclusion in sport: Inclusive approach to sports development .........p9 • Scottish Disability Sport • JudoScotland Inclusive support for an emerging sport ...........p10 • Active Schools Network • Scottish Football Association • City of Edinburgh Council • Scottish Disability Equality Forum • Lothian Disability Sport • PAMIS • Sport 4 All Club • Fife Sports and Leisure Trust • Disability Sport Fife • Royal Caledonian Curling Club • Basketball Scotland • Inverclyde Council sportscotland Doges Templeton on the Green 62 Templeton Street Glasgow G40 1DA Tel: 0141 534 6500 Fax: 0141 534 6501 www.sportscotland.org.uk -

List of Sports
List of sports The following is a list of sports/games, divided by cat- egory. There are many more sports to be added. This system has a disadvantage because some sports may fit in more than one category. According to the World Sports Encyclopedia (2003) there are 8,000 indigenous sports and sporting games.[1] 1 Physical sports 1.1 Air sports Wingsuit flying • Parachuting • Banzai skydiving • BASE jumping • Skydiving Lima Lima aerobatics team performing over Louisville. • Skysurfing Main article: Air sports • Wingsuit flying • Paragliding • Aerobatics • Powered paragliding • Air racing • Paramotoring • Ballooning • Ultralight aviation • Cluster ballooning • Hopper ballooning 1.2 Archery Main article: Archery • Gliding • Marching band • Field archery • Hang gliding • Flight archery • Powered hang glider • Gungdo • Human powered aircraft • Indoor archery • Model aircraft • Kyūdō 1 2 1 PHYSICAL SPORTS • Sipa • Throwball • Volleyball • Beach volleyball • Water Volleyball • Paralympic volleyball • Wallyball • Tennis Members of the Gotemba Kyūdō Association demonstrate Kyūdō. 1.4 Basketball family • Popinjay • Target archery 1.3 Ball over net games An international match of Volleyball. Basketball player Dwight Howard making a slam dunk at 2008 • Ball badminton Summer Olympic Games • Biribol • Basketball • Goalroball • Beach basketball • Bossaball • Deaf basketball • Fistball • 3x3 • Footbag net • Streetball • • Football tennis Water basketball • Wheelchair basketball • Footvolley • Korfball • Hooverball • Netball • Peteca • Fastnet • Pickleball -

Living Your Life: Sports and Fitness
Useful Resources The Simon Foundation Hollister Continence Care for Continence The American Urological www.simonfoundation.org Association 1.800.23SIMON (237.4666) www.auanet.org 1.866.RING AUA Spina Bifida Living Your Life (1.866.746.4282) Association Sports and Fitness www.sbaa.org Christopher 1.800.621.3141 and Dana Reeve Foundation Spinal Cord Injury www.crpf.org Information Network 1.800.225.0292 www.spinalcord.uab.edu 1.205.934.3283 The Buoniconti Fund to Cure Paralysis Us Too International, Inc. www.thebuonicontifund.com www.ustoo.org 1.888.STANDUP (782.6387) 1.800.80.USTOO (1.800.808.7866) The Miami Project to Cure Paralysis www.miamiproject.miami.edu 1.800.STANDUP (782.6387) National Association for Continence (NAFC) www.nafc.org 1.800.BLADDER (252.3337) National Rehabilitation Information Center www.naric.com 1.800.346.2742 National Spinal Cord Hollister Incorporated Injury Association 2000 Hollister Drive Libertyville, Illinois 60048 USA www.spinalcord.org 1.888.740.8999 1.800.913.6370 Distributed by Paralyzed Veterans Hollister Limited of America 95 Mary Street Aurora, Ontario L4G 1G3 www.pva.org 1.800.263.7400 1.800.555.9140 www.hollister.com Information for people living with Hollister and logo is a trademark of Hollister Incorporated. mobility issues and bladder dysfunction ©2010 Hollister Incorporated. 910831-611 Table of Contents If you worked hard to keep fit before your spinal cord injury (SCI), you will find that there are still many ways to stay active. Sports and fitness can still be a big part Introduction. 3 of your life.