Semester 4 Handbook
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vendredi 22 Et Samedi 23 Février 2013 À 13 H Vrijdag 22 En Zaterdag 23 Februari 2013 Om 13 U
VENTE PUBLIQUE DE LIVRES ET DE GRAVURES OPENBARE VEILING VAN BOEKEN EN PRENTEN Vendredi 22 et samedi 23 février 2013 à 13 h Vrijdag 22 en zaterdag 23 februari 2013 om 13 u Exposition et vente À LA LIBRAIRIE Ch. de Charleroi 162, 1060 Bruxelles Tentoonstelling en veiling IN DE BOEKHANDEL Charleroisesteenweg 162, 1060 Brussel Exposition : Vendredi 15 et samedi 16 février de 10 à 19 h, du lundi 18 au mercredi 20 février de 10 à 19 h et jeudi 21 février de 10 à 18 h Tentoonstelling : Vrijdag 15 en zaterdag 16 februari van 10 tot 19 u, van maandag 18 tot woensdag 20 februari van 10 tot 19 u en donderdag 21 februari van 10 tot 18 u LE LIBRAIRE ALAIN FERRATON Chaussée de Charleroi, 162/8 – B 1060 Bruxelles Ouvert du mardi au samedi de 10 à 18 h 30 Charleroisesteenweg, 162/8 – B 1060 Brussel Open van dinsdag tot zaterdag van 10 tot 18 u 30 Phone : 00. 32 (0)2.538.69.17 – Fax : 00. 32 (0)2.537.46.05 Mail : [email protected] Internet : www.ferraton.be TABLE DES MATIÈRES PREMIÈRE VACATION : VENDREDI 22 FÉVRIER 2013 À 13 H Livres anciens du 16e au 18e s. – Impressions populaires –Emblemata 1-118 Révolution française et Premier Empire (1789-1815) 120-200 Histoire – Géographie – Voyages 201-232 Autographes historiques, scientifiques et littéraires 233-248 Belgicana 249-306 Bibliographie, histoire du livre et de la gravure, imagerie populaire, ex-libris, manuscrits à miniature 307-358 Sciences et techniques 359-362 Franc-Maçonnerie 363-365 Enfantina et bandes dessinées 366-372 Musique et cinéma 373-376 Asie, Afrique, Amérique, Océanie… : art, histoire, voyages, ethnographie 377-479 Architecture 480-484 Arts appliqués 485-496 Art ancien de l’Antiquité au 18e siècle 497-584 « Univers des Formes » 585-594 SECONDE VACATION : SAMEDI 23 FÉVRIER 2013 À 13 H Cartes postales – Chromos 595-614 Cartes topographiques et gravures anciennes 615-624 Gravures et dessins (19e et 20e siècles) 625-665 Photographies 666-682 Éditions « Pierre d’Alun » 683-699 De Dada à Cobra : Les Avant-gardes artistiques et littéraires du 20e s. -
2020-Commencement-Program.Pdf
THE JOHNS HOPKINS UNIVERSITY COMMENCEMENT 2020 Conferring of degrees at the close of the 144th academic year MAY 21, 2020 1 CONTENTS Degrees for Conferral .......................................................................... 3 University Motto and Ode ................................................................... 8 Awards ................................................................................................. 9 Honor Societies ................................................................................. 20 Student Honors ................................................................................. 25 Candidates for Degrees ..................................................................... 35 2 ConferringDegrees of Degrees for Conferral on Candidates CAREY BUSINESS SCHOOL Masters of Science Masters of Business Administration Graduate Certificates SCHOOL OF EDUCATION Doctors of Education Doctors of Philosophy Post-Master’s Certificates Masters of Science Masters of Education in the Health Professions Masters of Arts in Teaching Graduate Certificates Bachelors of Science PEABODY CONSERVATORY Doctors of Musical Arts Masters of Arts Masters of Audio Sciences Masters of Music Artist Diplomas Graduate Performance Diplomas Bachelors of Music SCHOOL OF NURSING Doctors of Nursing Practice Doctors of Philosophy Masters of Science in Nursing/Advanced Practice Masters of Science in Nursing/Entry into Nursing Practice SCHOOL OF NURSING AND BLOOMBERG SCHOOL OF PUBLIC HEALTH Masters of Science in Nursing/Masters of Public -

Lista De Espera Para Chamada Presencial
LISTA DE ESPERA PARA CHAMADA PRESENCIALDO SISU 2013/2 - UFSJ - CONFORME ITEM 3 DO EDITAL COMPLEMENTAR 013/2013 A Chamada Presencial será feita nos dias e horário, conforme especificado no Quadro 1.2 do Edital 013/2013 As informações para a Chamada Presencial estão especificadas no item 3 do Edital 013/2013 Documentos a serem apresentados para a matrícula na Chamada Presencial, verificar subitens 3.10, 3.11 e 3.13 do Edital 013/2013 Colocação Nova reclassificação Nota no Campus Curso Turno Formação Nome do Candidato RG Tipo de Vaga por tipo de conforme subitens 3.1 e ENEM vaga 3.2, do Edital 013/2013 CAMPUS ALTO PARAOPEBA - CAP ENG. CIVIL Integral Bacharelado CASSIO LUIZ SIQUEIRA 17436858 663.24 AC 63 1 CAMPUS ALTO PARAOPEBA - CAP ENG. CIVIL Integral Bacharelado ISMAEL RAMALHO DA COSTA SOARES 6299841 663.11 AC 64 2 CAMPUS ALTO PARAOPEBA - CAP ENG. CIVIL Integral Bacharelado BRUNO AMANCIO TEIXEIRA SILVA 6019538 663.05 AC 65 3 CAMPUS ALTO PARAOPEBA - CAP ENG. CIVIL Integral Bacharelado DIEGO HENRIQUE OLIVEIRA ARAUJO MG-18.676.459 663.04 AC 66 4 CAMPUS ALTO PARAOPEBA - CAP ENG. CIVIL Integral Bacharelado BERNARDO MICHEL SLAILATI MG-15.988.911 662.00 AC 67 5 CAMPUS ALTO PARAOPEBA - CAP ENG. CIVIL Integral Bacharelado DANIELY EL MOALLEM MG - 11483469 661.47 AC 68 6 CAMPUS ALTO PARAOPEBA - CAP ENG. CIVIL Integral Bacharelado PEDRO AUGUSTO DA SILVA BRAGA MG-18.359.459 661.39 AC 69 7 CAMPUS ALTO PARAOPEBA - CAP ENG. CIVIL Integral Bacharelado MIRIAM ZAIDAN DE SOUZA MG13737677 659.55 AC 70 8 CAMPUS ALTO PARAOPEBA - CAP ENG. -

Madonna and Child with Saint John the Baptist, Saint Peter, and Two Angels C
National Gallery of Art NATIONAL GALLERY OF ART ONLINE EDITIONS Italian Paintings of the Thirteenth and Fourteenth Centuries Tuscan 13th Century Madonna and Child with Saint John the Baptist, Saint Peter, and Two Angels c. 1290 tempera on panel painted surface (original panel including painted frame): 34.3 × 24.7 cm (13 1/2 × 9 3/4 in.) overall (including added wooden strips): 36 × 26 cm (14 3/16 × 10 1/4 in.) Inscription: on the scroll held by Saint John the Baptist: E[C]CE / AGNU[S] / DEI:[ECCE] / [Q]UI [TOLLIT PECCATUM MUNDI] (from John 1:29) Samuel H. Kress Collection 1952.5.60 ENTRY The enthroned Madonna supports her son, seated on her left knee, with both hands. The child, in a frontal position, blesses with his right hand, holding a roll of parchment in his left. The composition is a variant of the type of the Hodegetria Virgin; in the present case, she does not point towards her son, as in the Byzantine prototype, but instead presents him to the spectator. [1] Her affectionate maternal pose is thus given precedence over her more ritual and impersonal role. But Mary’s pose perhaps has another sense: she seems to be rearranging her son’s small legs to conform them to the cross-legged position considered suitable for judges and sovereigns in the Middle Ages. [2] The panel is painted in a rapid, even cursory manner. The artist omits the form of the throne’s backrest, which remains hidden by the cloth of honor, supported by angels and decorated with bold motifs of popular taste (an interlocking pattern of quatrefoils and octagons). -

Zbwleibniz-Informationszentrum
A Service of Leibniz-Informationszentrum econstor Wirtschaft Leibniz Information Centre Make Your Publications Visible. zbw for Economics Eklund, Jana; Karlsson, Sune Working Paper Forecast Combination and Model Averaging using Predictive Measures Sveriges Riksbank Working Paper Series, No. 191 Provided in Cooperation with: Central Bank of Sweden, Stockholm Suggested Citation: Eklund, Jana; Karlsson, Sune (2005) : Forecast Combination and Model Averaging using Predictive Measures, Sveriges Riksbank Working Paper Series, No. 191, Sveriges Riksbank, Stockholm This Version is available at: http://hdl.handle.net/10419/82428 Standard-Nutzungsbedingungen: Terms of use: Die Dokumente auf EconStor dürfen zu eigenen wissenschaftlichen Documents in EconStor may be saved and copied for your Zwecken und zum Privatgebrauch gespeichert und kopiert werden. personal and scholarly purposes. Sie dürfen die Dokumente nicht für öffentliche oder kommerzielle You are not to copy documents for public or commercial Zwecke vervielfältigen, öffentlich ausstellen, öffentlich zugänglich purposes, to exhibit the documents publicly, to make them machen, vertreiben oder anderweitig nutzen. publicly available on the internet, or to distribute or otherwise use the documents in public. Sofern die Verfasser die Dokumente unter Open-Content-Lizenzen (insbesondere CC-Lizenzen) zur Verfügung gestellt haben sollten, If the documents have been made available under an Open gelten abweichend von diesen Nutzungsbedingungen die in der dort Content Licence (especially Creative Commons -

Learning from SHOGUN
Learning from Shǀgun Japanese History and Western Fantasy Edited by Henry Smith Program in Asian Studies University of California, Santa Barbara Santa Barbara, California 93106 Contents Designed by Marc Treib Contributors vi Copyright © 1980 by Henry D. Smith II Maps viii for the authors Preface xi Distributed by the Japan Society, 333 East 47th Street, New York, Part I: The Fantasy N.Y. 10017 1 James Clavell and the Legend of the British Samurai 1 Henry Smith 2 Japan, Jawpen, and the Attractions of an Opposite 20 Illustrations of samurai armor are David Plath from Murai Masahiro, Tanki yǀryaku 3 Shǀgun as an Introduction to Cross-Cultural Learning 27 (A compendium for the mounted Elgin Heinz warrior), rev. ed., 1837, woodblock edition in the Metropolitan Museum Part II: The History of Art, New York 4 Blackthorne’s England 35 Sandra Piercy 5 Trade and Diplomacy in the Era of Shǀgun 43 Ronald Toby 6 The Struggle for the Shogunate 52 Henry Smith 7 Hosokawa Gracia: A Model for Mariko 62 Chieko Mulhern This publication has been supported by Part III: The Meeting of Cultures grants from: 8 Death and Karma in the World of Shǀgun 71 Consulate General of Japan, Los William LaFleur Angeles 9 Learning Japanese with Blackthorne 79 Japan-United States Susan Matisoff Friendship Commission 10 The Paradoxes of the Japanese Samurai 86 Northeast Asia Council, Henry Smith Association for Asian Studies 11 Consorts and Courtesans: The Women of Shǀgun 99 USC-UCLA Joint East Asia Henry Smith Studies Center 12 Raw Fish and a Hot Bath: Dilemmas of Daily Life 113 Southern California Conference on Henry Smith International Studies Who’s Who in Shǀgun 127 Glossary 135 For Further Reading 150 Postscript: The TV Transformation 161 vi Contributors vii Sandra Piercy is a graduate student in English history of the Tudor- Stuart period at the University of California, Santa Barbara. -
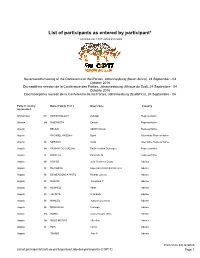
List of Participants As Entered by Participant* * Excludes Over 1,500 Visitors and Media
List of participants as entered by participant* * excludes over 1,500 visitors and media Seventeenth meeting of the Conference of the Parties, Johannesburg (South Africa), 24 September - 04 October 2016 Dix-septième session de la Conférence des Parties, Johannesbourg (Afrique du Sud), 24 Septembre - 04 Octobre 2016 Decimoséptima reunión de la Conferencia de las Partes, Johannesburg (Sudáfrica), 24 Septiembre - 04 Party or country Name (Family, First ) Given name Category represented Afghanistan Mr KARIMI BALOCH Zolfaqar Representative Albania Ms RABDHISTA Eneida Representative Algeria BELAID Abd-El-Naceur Representative Algeria KACIMIEL HASSANI Djalal Alternative Representative Algeria Mr MESBAH Reda Alternative Representative Angola Ms FRANCISCO COELHO Paula Cristina Domingos Representative Angola Dr NICOLAU Benvindo M Representative Angola Mr BANGO Julio Cristóvao Diogo Adviser Angola Dr DA COSTA Esperanca Maria E Francisco Adviser Angola Mr DE MENDONCA PINTO Nivaldo Lukeny Adviser Angola Mr DIAKITE Josephina P Adviser Angola MrHUONGO Abias Adviser Angola MrJACINTO D Orlando Adviser Angola Mr MANUEL Joaquim Lourenzo Adviser Angola MrMIAKONGO Lusanga Adviser Angola Ms NOBRE Luana Nayole Silva Adviser Angola Ms NZUZI MATIAS Albertina Adviser Angola DrRON Tamar Adviser Angola SAMBO Jose A Adviser Printed on 12/12/2016 List of participants/Lista de participantes/Liste des participants (COP17) Page: 1 Antigua and Barbuda Mr JOSEPH Daven C Representative Argentina Mr FIGUEROA Javier Esteban Representative Argentina Ms HURTADO Patricia Edith -

Annual Report
Honor Roll of DONORS Fiscal Year 2010, July1, 2009 to June 30, 2010 College of Staten Island FOUNDATION Message from the President Greetings! It is my pleasure as the President of the College of Staten Island to introduce the CSI Foundation’s 2009-2010 Honor Roll of Donors. Honor Roll of DONORS of Roll Honor The Honor Roll of Donors showcases the invaluable support provided by CSI’s generous donors over the past year. As for many, this year has highlighted several continued challenging economic conditions. For CSI, we mark this year for its many successes: from touching the lives of thousands of students as Staten Island’s only public institution for higher education to supporting cutting-edge research through the CUNY High- Performance Computing Facility, as well as the Staten Island Breast Cancer Research Initiative. CSI has a long and well-grounded history of success and achievement, and we continue to strive ever upward. With each passing year, CSI makes remarkable strides in its efforts to nurture a diverse learning environment, while enhancing the student learning experience. We look forward to making even greater advancements this year with your continued assistance. Thank you to our outstanding faculty, our hard-working students and their very supportive families, our caring staff, the tireless Foundation Board, and, of course, our tremendously involved and generous family of alumni and donors! Together, you continue to help write CSI’s story of success. Sincerely, Tomás D. Morales, PhD President CSI FOUNDATION DONORS Judith K. Greene and Robert W. Greene Mary F. Regan ‘72 and James F. -

Mosaic Magazine Fall 2018
MERCY HIGH SCHOOL MAGAZINE PUBLISHED TWICE YEARLY FOR ALUMNAE, PARENTS & FRIENDS FALL / WINTER 2018 INSIDE THIS I SSUE Madame Joyce Smetanka Campbell 2017-18 Honor Roll of Donors Grandparents Mass Advancing Mercy mhsmi.org LETTER FROM MERCY’S PRESIDENT CREATED BY MERCY’S FOUNDING MOTHER OF ART MARY IGNATIUS DENAY, RSM A MOSAIC IS AN ARRAY OF DIVERSE ELEMENTS JOINED TOGETHER TO CREATE A GREATER WHOLE. Dearest Mercy Family, Mercy High School Board of Trustees Nancy A. Auffenberg - Chair Each day, the lives of our young women are transformed through the MHSMI.ORG Cheryl Delaney Kreger, Ed.D. ’66 - President Visit Karla E. Rose Middlebrooks ’76 - Treasurer gift of a Mercy education. I am grateful for your time and treasure on Stay connected with what's happening at Judith A. VanderVeen, RSM - Secretary Mercy. Read and sign up to receive alumnae Anne Blake Ph.D. behalf of our school through giving, volunteering, attending events and parent e-newsletters, browse Jared P. Buckley and spreading good news about Mercy. Our cherished community Mercy High School the school year calendar, and check out Margaret Dimond, Ph.D. ’76 is sustained and advanced by the active support of all members and 29300 W. 11 Mile Road Mercy event photos and news articles. Anne Fleming, RSM Dave Hall Farmington Hills, MI 48336-1409 friends. Because of you, this past year has been another great one Susan Hartmus Hiser Email: [email protected] Brigid Johnson, RSM ’53 filled with accomplishments and opportunities for our Mercy students. Tel: (248) 476-8020 Diana Mercer-Pryor Fax: (248) 476-3691 Carla LaFave O’Malley ’70 Because of you: Students form a meaningful relationship with God Mercy Sharon Sanderson Anita M. -

Surnames in the Master Index. Names Were Transcribed from Many
Surnames in the Master Index. Names were transcribed from many different sources including: Birth Records, Cemetery Records, Census, Church Records, Death Certificates, Funeral Home Records, High School Graduation Records, Historical Books, Land Records, Marriage Records, Military Records, Museum Records, Newspaper Clippings, Obituaries, Passport Applications. For additional information contact the Excelsior Springs Museum & Archives at [email protected] Aaron Achenbach Adkison Aid Albriecht Allee Aastrom Achtenberg Adkisson Aiken Albright Allegrini Abanishe Acimoff Adle Aikers Albrighton Alleman Abar Acker Adlen Aikmus Albrigts Allen Abbas Ackerly Adler Ailor Albritton Allenbrand Abbe Ackerman Adlich Ailshier Albro Allender Abbett Ackers Admire Ailshire Alburtis Aller Abbey Ackerson Admires Aimmlath Alcoorn Alley Abbiatti Acklane Adock Aines Alcorn Allgaier Abbington Ackley Adrain Ainsworth Alcott Allie Abbot Acklin Adrews Aires Alcox Alliet Abbott Ackromavich Adrian Airhart Aldana Alliott Abdoler Acord Adriany Airvin Alden Allison Abdullah Acre Aethis Aitkens Alder Allman Abdy Acree Afer Akagi Aldera Allmon Abel Acreg Affalter Ake Alderdice Allnutt Abele Acres Afflack Aken Alderman Allon Abell Action Affolter Aker Alderson Allred Abeln Acton Affronti Akerman Aldred Allres Aber Acuff Affult Akers Aldredge Allsman Aberle Adair Afromob Akerson Aldrete Allspan Abernathy Adam Agans Akes Aldrich Allspaugh Abernethy Adames Agderian Akimoto Aldrick Allstat Abertson Adamoli Agee Akin Aldridge Allstate Abfalder Adams Agey Akins Alee Allton -

Copyright by the American Historical Society of Germans from Russia, International (AHSGR)
GEDLIST Copyright by The American Historical Society of Germans from Russia, International (AHSGR). All rights reserved. Compiled August 1, 2018, from GEDCOMS submitted to The American Historical Society of Germans from Russia. International (AHSGR) Submit corrections to: [email protected] None of this data may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the copyright holder. For information about obtaining a copy of this data, contact The American Historical Society of Germans from Russia, International (AHSGR); www.ahsgr.org Click the back button on your browser to return to the GEDLIST home page. Birth/*Chr Date and Place not listed for living persons! Surname, Given | Birth or *Chr Date | Birth or *Chr Place | Death or *Burial Date | Death or *Burial Place C, Danette -B899 C, Edison -S1395 C, Edwin -S1395 C., Sarah -L303 1866 1895 Liberty Cemetery; Shelbyville, Indiana C.C.WEIS, -F224 CAALIM, Edward -K147 CABANISS, Michael -M-F170 Jan-64 CABEL, Conrad -O074 CABEL, Wendy -B483 CABINESS, Jane (Jincy) -G506 Abt 1775 CABLE, Alice Adelpa -S329 CABLE, Gordon -R210 CABLE, Louise Dinvee -C134 7-Feb-49 Winchester, Wolf Co, Kentucky CABLE, Robert -C134 Abt 1925 CABRALOFF, Armand -S850 Private CABRERA, Blaise -L277 1882 CABRERA, Marie-Rose -L277 29-Nov-12 Algiers, Algeria 27-Mar-54 Algiers, Algeria CACEK, Edward -C-C032 CACICIA, Charles -P-F027 22-Aug-08 Portland, Multnomah Co, Oregon 22-May-69 Portland, -

3Rd Schizophrenia International Research Society Conference Schizophrenia: the Globalization of Research
3rd Schizophrenia International Research Society Conference Schizophrenia: The Globalization of Research FLORENCE, ITALY 14 - 18 APRIL 2012 This meeting is jointly sponsored by the Vanderbilt University School of Medicine and the Schizophrenia International Research Society 3rd Schizophrenia International Research Society Conference Schizophrenia: The Globalization of Research Opening letter Dear Attendees, It is our great pleasure to welcome you to the 3rd Biennial Schizophrenia International Research Society (SIRS) Conference. SIRS is a non-profit organization dedicated to promoting research and communication about schizophrenia among research scientists internationally. We sincerely appreciate your interest in the Society and in our conference. The second congress in 2010 was a major success for the field attracting more than 1500 attendees from 53 countries. We anticipate an even higher attendance at this congress with most of the best investigators in the world in attendance. SIRS was founded in 2005 with the goal of bringing together scientists from around the world to exchange the latest advances in biological and psychosocial research in schizophrenia. The Society strives to facilitate international collaboration to discover the causes of, and better treatments for, schizophrenia and related disorders. Part of the mission of the Society is to promote educational programs in order to effectively disseminate new research findings and to expedite the publication of new research on schizophrenia. In addition to the Biennial Congress, the Society hosted the first regional meeting in São Paulo, Brazil in August of 2011. The meeting was a great success with over 150 presenters and 400 attendees. Under the outstanding leadership of Program Committee Chair Jim van Os and Co-Chair Dawn Velligan, we have an exciting scientific program planned for the 3rd Biennial Conference.