HIV TRANSMISSION: Guidelines for Assessing Risk
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
View/Method……………………………………………………9
UNIVERSITY OF CINCINNATI Date:___________________July 23, 2007 I, ________________________________________________Julie M. Stewart _________, hereby submit this work as part of the requirements for the degree of: Master of Arts in: Communication It is entitled: The Rhetoric of South Park This work and its defense approved by: Chair: _______________________________Dr. John Lynch _______________________________Dr. Stephen Depoe _______________________________Dr. William Jennings _______________________________ _______________________________ THE RHETORIC OF SOUTH PARK A thesis submitted to the Division of Graduate Studies and Research Of the University of Cincinnati MASTER OF ARTS In the Department of Communication, of the College of Arts and Sciences 2007 by Julie Stewart B.A. Xavier University, 2001 Committee Chair: Dr. John Lynch Abstract This study examines the rhetoric of the cartoon South Park. South Park is a popular culture artifact that deals with numerous contemporary social and political issues. A narrative analysis of nine episodes of the show finds multiple themes. First, South Park is successful in creating a polysemous political message that allows audiences with varying political ideologies to relate to the program. Second, South Park ’s universal appeal is in recurring populist themes that are anti-hypocrisy, anti-elitism, and anti- authority. Third, the narrative functions to develop these themes and characters, setting, and other elements of the plot are representative of different ideologies. Finally, this study concludes -

Emotional and Linguistic Analysis of Dialogue from Animated Comedies: Homer, Hank, Peter and Kenny Speak
Emotional and Linguistic Analysis of Dialogue from Animated Comedies: Homer, Hank, Peter and Kenny Speak. by Rose Ann Ko2inski Thesis presented as a partial requirement in the Master of Arts (M.A.) in Human Development School of Graduate Studies Laurentian University Sudbury, Ontario © Rose Ann Kozinski, 2009 Library and Archives Bibliotheque et 1*1 Canada Archives Canada Published Heritage Direction du Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington OttawaONK1A0N4 OttawaONK1A0N4 Canada Canada Your file Votre reference ISBN: 978-0-494-57666-3 Our file Notre reference ISBN: 978-0-494-57666-3 NOTICE: AVIS: The author has granted a non L'auteur a accorde une licence non exclusive exclusive license allowing Library and permettant a la Bibliotheque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par telecommunication ou par I'lnternet, prefer, telecommunication or on the Internet, distribuer et vendre des theses partout dans le loan, distribute and sell theses monde, a des fins commerciales ou autres, sur worldwide, for commercial or non support microforme, papier, electronique et/ou commercial purposes, in microform, autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriete du droit d'auteur ownership and moral rights in this et des droits moraux qui protege cette these. Ni thesis. Neither the thesis nor la these ni des extraits substantiels de celle-ci substantial extracts from it may be ne doivent etre imprimes ou autrement printed or otherwise reproduced reproduits sans son autorisation. -

City Council Regular Meeting Agenda
Mayor Laura North City of Kingsburg Mayor Pro Tem Vince Palomar Council Member Michelle Roman 1401 Draper Street, Kingsburg, CA 93631-1908 Council Member Jewel Hurtado Phone (559)897-5821 Fax (559)897-5568 Council Member Brandon Pursell, Jr. City Manager Alexander J. Henderson AGENDA KINGSBURG CITY COUNCIL REGULAR MEETING Council Chamber, 1401 Draper Street, Kingsburg, CA 93631 (559) 897-5821 www.cityofkingsburg-ca.gov PURSUANT TO EXECUTIVE ORDER N-29-20 ISSUED BY GOVERNOR GAVIN NEWSOM THE COUNCIL CHAMBER WILL BE OPEN AT 50% CAPACITY (including City Council Members and City Staff) TO THE PUBLIC. PUBLIC WILL ALSO HAVE THE OPTION TO CALL 1 (425) 436-6335 PASSCODE 5290024 TO PROVIDE COMMENTS ON AGENDA ITEMS. WRITTEN COMMENTS CAN STILL BE SUBMITTED BY MAIL OR EMAIL TO APALSGAARD@CITYOFKINGSBURG- CA.GOV. THE CUT OFF FOR WRITTEN COMMENTS IS 05/18/2021 at 4:30pm. THEY WILL NOT BE READ OUT LOUD. Wednesday, May 19, 2021 at 6pm Invocation to be given by Pastor Tim Boynton, of The Kingsburg Covenant Church, followed by the Pledge of Allegiance led by Mayor Laura North. 6 P.M. REGULAR SESSION MEETING: 1. Call to Order and Roll Call 2. Public Comments: This is the time for any citizen to come forward and address the City Council on any issue within its jurisdiction that is not listed on the Agenda. A maximum of five (5) minutes is allowed for each speaker. 3. Approve Agenda: Action by the Council to approve the agenda or to make modifications. Items that can be added to the agenda is constrained by State law. -

De Representatie Van Leraren En Onderwijs in Populaire Cultuur. Een Retorische Analyse Van South Park
Universiteit Gent, Faculteit Psychologie en Pedagogische Wetenschappen Academiejaar 2014-2015 De representatie van leraren en onderwijs in populaire cultuur. Een retorische analyse van South Park Jasper Leysen 01003196 Promotor: Dr. Kris Rutten Masterproef neergelegd tot het behalen van de graad van master in de Pedagogische Wetenschappen, afstudeerrichting Pedagogiek & Onderwijskunde Voorwoord Het voorwoord schrijven voelt als een echte verlossing aan, want dit is het teken dat mijn masterproef is afgewerkt. Anderhalf jaar heb ik op geregelde basis gezwoegd, gevloekt en getwijfeld, maar het overheersende gevoel is toch voldoening. Voldoening om een werk af te hebben waar veel tijd en moeite is ingekropen. Voldoening om een werk af te hebben waar ik toch wel fier op ben. Voldoening om een werk af te hebben dat ik zelfstandig op poten heb gezet en heb afgewerkt. Althans hoofdzakelijk zelfstandig, want ik kan er niet omheen dat ik regelmatig hulp heb gekregen van mensen uit mijn omgeving. Het is dan ook niet meer dan normaal dat ik ze hier even bedank. In de eerste plaats wil ik mijn promotor, dr. Kris Rutten, bedanken. Ik kon steeds bij hem terecht met vragen en opmerkingen en zijn feedback gaf me altijd nieuwe moed en inspiratie om aan mijn thesis verder te werken. Ik apprecieer vooral zijn snelle en efficiënte manier van handelen. Nooit heb ik lang moeten wachten op een antwoord, nooit heb ik vele uren zitten verdoen op zijn bureau. Bedankt! Ten tweede wil ik ook graag Ayna, Detlef, Diane, Katoo, Laure en Marijn bedanken voor deelname aan mijn focusgroep. Hun inzichten hebben ervoor gezorgd dat mijn analyses meer gefundeerd werden, hun enthousiasme heeft ertoe bijgedragen dat ik besefte dat mijn thesis zeker een bijdrage is voor het onderzoeksveld. -

Safer Sex for Lesbian & Bisexual Women
SAFER SEX FOR LESBIAN & BISEXUAL WOMEN FINGER COTS DENTAL DAM aka finger condoms Square piece of latex that is used to assist in the prevention of Made of latex and worn like a glove on one finger HIV and STI tranmission during oral or anal sex HOW TO USE: Use when fingering. You can also make one by HOW TO USE: Lay the dental dam flat against the entire vulva, the cutting off a finger from a latex glove. vaginal opening and the clitoris. Make sure the entire vaginal area is covered. For rimming (licking the anus), place it against the anus. Once the dam is in place, you can lick away. Use a new dental dam for each new sex act. LATEX GLOVES Disposable fitted gloves used by medical professionals. Latex gloves can be used for oral sex, rimming, fingering, and fisting. Be LUBE sure to NOT use dishwashing gloves. Jellylike substance that reduces friction, which causes tiny tears in the skin and makes HOW TO USE: it more likely to get an infection. Lube can also make Oral sex – Cut the fingers off the glove, leaving the thumb in place. Cut open the side of the glove sex feel better and more exciting, whether having oral opposite the thumb. Hold the glove in place with both hands or penetrative sex, masturbating, or using sex toys. It makes or have your partner hold it, covering her labia. Use your penetration easier and more pleasurablable. tongue to stimulate your partner. Insert your tongue into the thumb for extra fun. After sex, be sure to dispose HOW TO USE: Apply a small amount of lube to the of glove safely. -

Men Who Have Sex with Men Management a Management Approach for Gps
CLINICAL PRACTICE Men who have sex with men Management A management approach for GPs BACKGROUND At least one in 20 Australian men report sexual contact with another man in their lifetime. Men who have sex with other James Baber men have higher rates of sexually transmitted infections, and are more likely to experience mental health problems and BHB, MBChB, is a sexual use recreational drugs and alcohol. health registrar, Department of Sexual Health, Royal North OBJECTIVE Shore Hospital, Sydney, New This article describes the health problems and sexual behaviour of men who have sex with men and provides an outline South Wales. jbaber@nsccahs. health.nsw.gov.au and an approach to discussing sexuality in general practice. Linda Dayan DISCUSSION BMedSc, MBBS, DipRACOG, Sexuality can be difficult to discuss in general practice. A nonjudgmental approach to men who have sex with men may MM(VenSci), FAChSHM, facilitate early identification of the relevant health issues. MRCMA, is Head, Department of Sexual Health, Royal North Shore Hospital, Director, Sexual Health Services, Northern Sydney Central Coast Area Health Service, Clinical Lecturer, Department of A recent Australian study has shown that 1.7% of men GP is a marker of increased numbers of sexual partners Community and Public Health, identify as exclusively homosexual,1 while 5% of all and higher sexual risk.4 University of Sydney, and in private practice, Darlinghurst, men reported genital homosexual experience through Barriers to discussing sexual health matters with New South Wales. their lifetime.2 nonheterosexuals identified by GPs in the United Kingdom in 2005, included a lack of knowledge of sexual practices Men who have sex with men (MSM) face societal prejudice and terminology.5 Several doctors also recognised that in their lives, and many experience discrimination. -
Hiv/Aids Basics for Ngos and Family Planning Program Managers
THE CEDPA TRAINING MANUAL SERIES family planning plus: hiv/aids basics for ngos and family planning program managers Integrating Reproductive Health and HIV/AIDS for NGOs, FBOs & CBOs Vol. I THE enable PROJECT ENABLING CHANGE FOR WOMEN'S THE CENTRE FOR DEVELOPMENT REPRODUCTIVE HEALTH AND POPULATION ACTIVITIES Family Planning Plus: HIV/AIDS Basics for Non-Governmental Organizations and Family Planning Program Managers Integrating Reproductive Health and HIV/AIDS for Non-Governmental Organizations, Faith-Based Organizations and Community-Based Organizations Volume I Family Planning Plus: HIV/AIDS Basics for NGOs and Family Planning Program Managers Authors Kathleen Callahan, MA Laurette Cucuzza, MPH This publication was supported by the United States Agency for International Development under Cooperative Agreement # HRN-A-00-98-00009-00. The contents of this document do not necessarily reflect the views or policies of the U.S. Agency for International Development or The Centre for Development and Population Activities (CEDPA). ii Family Planning Plus Abbreviations AIDS Acquired Immune Deficiency Syndrome ARV Antiretroviral CEDPA The Centre for Development and Population Activities HIV Human Immunodeficiency Virus MTCT Mother-to-Child Transmission NGO Non-Governmental Organization PLWHA People Living with HIV/AIDS RH Reproductive Health STI Sexually Transmitted Infection WHO World Health Organization UNAIDS Joint United Nations Program on AIDS UNDP United Nations Development Programme USAID United States Agency for International Development VCT Voluntary Counseling and Testing Overview iii Acknowledgements Headquartered in Washington, DC, The Centre for Development and Population Activities (CEDPA) is an international nonprofit organization that seeks to empower women at all levels of society to be full partners in development. -

What Happens in a Hook Up?: Young Women’S Behaviors, Emotions, and Pleasures
What Happens in a Hook Up?: Young Women’s Behaviors, Emotions, and Pleasures by Sarah N. Bell A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Psychology and Women’s Studies) in the University of Michigan 2018 Doctoral Committee: Assistant Professor Sara I. McClelland, Chair Associate Professor Terri D. Conley Professor Lilia M. Cortina Professor L. Monique Ward Sarah N. Bell [email protected] ORCID iD: 0000-0002-8796-7892 Dedication This dissertation is dedicated to my parents, Eileen and Dr. David Davies, whose unwavering support and endless sacrifices made this possible. ii Acknowledgements I would like to acknowledge the incredible feedback and guidance given to me by my advisor and mentor, Dr. Sara McClelland, throughout my time at the University of Michigan, and especially during the dissertation process. Her immeasurable wisdom guided me through some of the most difficult phases of this process. I would also like to acknowledge the other members of my dissertation committee, Dr. Lilia Cortina, Dr. Monique Ward, and Dr. Terri Conley. Their advice and support contributed immensely to the quality and rigor of this dissertation. Thank you for sharing your knowledge with me. iii Table of Contents Dedication ii Acknowledgements iii List of Tables v List of Appendices vii Abstract viii Chapter 1 Introduction 1 Chapter 2 Literature Review 12 Chapter 3 Women's Actual and Desired Hook Up Experiences 34 Chapter 4 Women's Sexual Pleasure in Hook Ups 86 Chapter 5 What Happens in a Typical Hook Up? 134 Chapter 6 Women's Complex Negotiation of Sexual and Gender Norms 185 Appendices 193 References 216 iv List of Tables Table 1 Women Receiving Oral and Manual Sex 74 Table 2 Rates of Orgasm 75 Table 3 Protected Vs. -

The ICD-10 Classification of Mental and Behavioural Disorders : Clinical Descriptions and Diagnostic Guidelines
ICD-10 ThelCD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines | World Health Organization I Geneva I 1992 Reprinted 1993, 1994, 1995, 1998, 2000, 2002, 2004 WHO Library Cataloguing in Publication Data The ICD-10 classification of mental and behavioural disorders : clinical descriptions and diagnostic guidelines. 1.Mental disorders — classification 2.Mental disorders — diagnosis ISBN 92 4 154422 8 (NLM Classification: WM 15) © World Health Organization 1992 All rights reserved. Publications of the World Health Organization can be obtained from Marketing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications — whether for sale or for noncommercial distribution — should be addressed to Publications, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers' products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Sexuality, Intimacy & Chronic Illness
FACT SHEET SEXUALITY, INTIMACY & CHRONIC ILLNESS Relationships and sexual satisfaction are important to quality of life. This is especially true for people coping with chronic illness. Sex is an act that can bring satisfaction and release. Even though ALS does not directly affect sexual function, for a person with ALS, sex may also bring pain, frustration and embarrassment. There are methods and techniques available to help people with ALS and their partners cope with their changing sex life and maintain intimacy. BENEFITS OF SEX SEXUAL RESPONSE CYCLE AND Chronic illness can restrict the activities of daily living. CHRONIC ILLNESS Maintaining a sexual relationship can be a source of com- Chronic illness can affect sexual satisfaction and the fort, pleasure and intimacy and an affirmation of one’s true sexual relationship for both partners. ALS does not impair self when other roles have been stripped away. A satisfying sexual function but medications, immobility, respiratory sex life, for the person with ALS and their partner, is one problems, fatigue and body image factors may negatively way to feel “normal” when so many other areas in their affect sexuality. lives have changed. Documented benefits of sex include the following: PSYCHOLOGICAL EFFECTS • Orgasm frequency is inversely related to risk of death. • Reduction of stress. • Anxiety, loss of self-esteem, grief and depression • Improved sleep post-orgasm. associated with chronic illness may impair sexual • Increased relationship satisfaction and stability. fulfillment. • Chronic illness alters relationship dynamics. Partners EFFECTS OF ALS ON SEXUALITY become caregivers, as well as lovers. Role changes may Understanding the sexual response cycle is important to cause sexual activity to decrease. -

Saliva Use As a Lubricant for Anal Sex Is a Risk Factor for Rectal Gonorrhoea
Downloaded from http://sti.bmj.com/ on March 27, 2016 - Published by group.bmj.com STI Online First, published on March 3, 2016 as 10.1136/sextrans-2015-052502 Epidemiology ORIGINAL ARTICLE Saliva use as a lubricant for anal sex is a risk factor for rectal gonorrhoea among men who have sex with men, a new public health message: a cross-sectional survey Eric P F Chow,1,2 Vincent J Cornelisse,1,2 Tim R H Read,1,2 David Lee,1 Sandra Walker,1,2 Jane S Hocking,3 Marcus Y Chen,1,2 Catriona S Bradshaw,1,2 Christopher K Fairley1,2 1Melbourne Sexual Health ABSTRACT that sexual practices other than penile–anal sex, Centre, Alfred Health, Background Apart from penile–anal intercourse, other such as digital–anal (‘fingering’) and oral–anal Melbourne, Victoria, Australia 2 anal sexual practices (rimming, fingering and saliva use (‘rimming’) sex, may play a key role in gonorrhoea Faculty of Medicine, Central 8 Clinical School, Nursing and as a lubricant for anal sex) are common among men transmission in MSM. Health Sciences, Monash who have sex with men (MSM). The aim of this study is Gonorrhoea transmission is still occurring in the University, Melbourne, Victoria, to evaluate whether these anal sexual practices are risk setting of condom use for penile–anal sex. If, Australia factors for rectal gonorrhoea in MSM. however, the penis is not solely involved in the 3Melbourne School of Population and Global Health, Method A cross-sectional survey was conducted acquisition of rectal gonorrhoea, a plausible alter- University of Melbourne, among MSM attending Melbourne Sexual Health Centre native mechanism is required. -
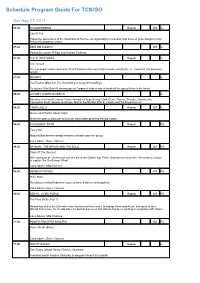
Program Guide Report
Schedule Program Guide For TCN/GO Sun Aug 21, 2011 06:00 THUNDERBIRDS Repeat WS G City Of Fire Follow the adventures of the International Rescue, an organisation created to help those in grave danger in this marionette puppetry classic. 07:00 KIDS WB SUNDAY WS G Hosted by Lauren Phillips and Andrew Faulkner. 07:05 THE FLINTSTONES Repeat G The Tycoon The fun begins when commoner Fred Flintstone discovers that he looks exactly like J.L. Gotrocks, the business tycoon. 07:30 SMURFS G The Fastest Wizard In The World/Sing A Song Of Smurflings To counter Wild Smurf's blazing speed Gargamel finds a way to break all the speed limits in the forest. 08:00 LOONEY TUNES CLASSICS G Adventures of iconic Looney Tunes characters Bugs Bunny, Daffy Duck, Tweety, Silvester, Granny, the Tasmanian Devil, Speedy Gonzales, Marvin the Martian Wile E. Coyote and the Road Runner. 08:30 CAMP LAZLO Repeat WS G Beans and Pranks/ Movie Night Slinkman goes undercover to find out who's been pranking the big moose. 09:00 SYM-BIONIC TITAN Repeat PG Tashy 497 Modula finds another deadly beast to unleash upon the group. Cons.Advice: Some Violence 09:30 BATMAN: THE BRAVE AND THE BOLD Repeat WS PG Trials Of The Demon! After taking on the Scarecrow with the aid of the Golden Age Flash, Batman must travel to 19th century London to capture the Gentleman Ghost. Cons.Advice: Mild Violence 10:00 GENERATOR REX WS PG Robo Bobo Rex discovers that Bobo has replaced himself with a robot duplicate.