Predictors of Non-Adherence to Public Health Instructions During the COVID-19 Pandemic in the Democratic Republic of the Congo
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Democratic Republic of the Congo (DRC) Reports Children in Need of Humanitarian Assistance Its First COVID-19 Confirmed Case
ef Democratic Republic of the Congo Humanitarian Situation Report No. 03 © UNICEF/UN0231603/Herrmann Reporting Period: March 2020 Highlights Situation in Numbers 9,100,000 • 10 March, the Democratic Republic of the Congo (DRC) reports children in need of humanitarian assistance its first COVID-19 confirmed case. As of 31 March 2020, 109 confirmed cases have been recorded, of which 9 deaths and 3 (OCHA, HNO 2020) recovered patients have been reported. During the reporting period, the virus has affected the province of Kinshasa and North Kivu 15,600,000 people in need • In addition to UNICEF’s Humanitarian Action for Children (HAC) (OCHA, HNO 2020) 2020 appeal of $262 million, UNICEF’s COVID-19 response plan has a funding appeal of $58 million to support UNICEF’s response 5,010,000 in WASH/Infection Prevention and Control, risk communication, and community engagement. UNICEF’s response to COVID-19 Internally displaced people can be found on the following link (HNO 2020) 6,297 • During the reporting period, 26,789 in cholera-prone zones and cases of cholera reported other epidemic-affected areas benefiting from prevention and since January response WASH packages (Ministry of Health) UNICEF’s Response and Funding Status UNICEF Appeal 2020 9% US$ 262 million 11% 21% Funding Status (in US$) 15% Funds Carry- received forward, 10% $5.5 M $28.8M 10% 49% 21% 15% Funding gap, 3% $229.3M 0% 20% 40% 60% 80% 100% 1 Funding Overview and Partnerships UNICEF appeals for US$ 262M to sustain the provision of humanitarian services for women and children in the Democratic Republic of the Congo (DRC). -

Actor Heatmap
2017 Q3 Report CONTENTS 1. Results & Overall Progress 2. Sectors 3. Regions 4. Cross-Cutting Sectors, Operations & Management 5. Business Development Services 6. Markets in Crisis 7. Women’s Economic Empowerment INTRODUCTION The third quarter was another busy one at ELAN RDC, as the programme balanced a mid-term evaluation and data verification process in addition to ongoing implementation. A number of new consultants contributed to increased activity for the technical team during the quarter, resulting in concrete workstreams on business development services (BDS), the launch of scoping to replicate existing interventions in conflict-affected Kasai Central, and a renewed focus on gender through increased support from our senior gender adviser. A number of large partnerships were finalised thanks to agreement with DFID on an improved non-objection review process, however, several large partnerships remained delayed due to multiple factors including increasing unstable market conditions. Partnerships in the energy and agriculture sectors were finalised during the quarter, while several partnerships in the financial sector faced delays. The programme has initiated a drive to increase and improve communications of programme results, resulting in an increase in visibility across various media. The launch of the Congo Coffee Atlas, completion of research for The Africa Seed Access Index (TASAI), meeting with mobile network operators to establish a lobbying platform and the finalisation of the contract for a renewable energy marketing campaign are all examples of activities through which ELAN RDC has made more market information available to the broader private sector. More details about third quarter results are found in the following slides. -

Introduction Generale
P a g e | 1 INTRODUCTION GENERALE 0.1. Problématique Le présent mémoire porte sur les logotypes et la signification : Analyse de la dénotation et de la connotation des logotypes des banques Trust Merchant Bank (TMB) et Rawbank. En effet, Sperber1 dit qu’il n’y a rien de plus banal que la communication, car les êtres humains sont par nature des êtres communiquant par la parole, le geste, l’écrit, l’habillement et voire le silence, etc. La célèbre école de Palo Alto le dit tout haut aussi: on ne peut pas ne pas communiquer, tout est communication2. La communication, nous la pratiquons tous les jours sans y penser (mais également en y pensant) et généralement avec un succès assez impressionnant, même si parfois nous sommes confrontés à ses limites et à ses échecs. La communication demeure l’élément fondamental et complexe de la vie sociale qui rend possible l’interaction des personnes et dont la caractéristique essentielle est, selon Daniel Lagache3, la réciprocité. Elle est ce par quoi une personne influence une autre et en est influencée, car elle n’est pas indépendante des effets de son action. Morin affirme même que la communication a plusieurs fonctions : l’information, la connaissance, l’explication et la compréhension. Toutefois, pour lui, le problème central dans la communication humaine est celui de la compréhension, car on communique pour comprendre et se comprendre4. Raison pour laquelle, les chercheurs en matière de communication, surtout de notre ère, époque marquée par l’accroissement des entreprises dans la plupart des secteurs de la vie sociale, se trouvent confronté à de nouvelles problématiques qui sont autant d’enjeux pour améliorer la communication. -

Of the United Nations Mission in the DRC / MONUC – MONUSCO
Assessing the of the United Nations Mission in the DRC / MONUC – MONUSCO REPORT 3/2019 Publisher: Norwegian Institute of International Affairs Copyright: © Norwegian Institute of International Affairs 2019 ISBN: 978-82-7002-346-2 Any views expressed in this publication are those of the author. Tey should not be interpreted as reflecting the views of the Norwegian Institute of International Affairs. Te text may not be re-published in part or in full without the permission of NUPI and the authors. Visiting address: C.J. Hambros plass 2d Address: P.O. Box 8159 Dep. NO-0033 Oslo, Norway Internet: effectivepeaceops.net | www.nupi.no E-mail: [email protected] Fax: [+ 47] 22 99 40 50 Tel: [+ 47] 22 99 40 00 Assessing the Efectiveness of the UN Missions in the DRC (MONUC-MONUSCO) Lead Author Dr Alexandra Novosseloff, International Peace Institute (IPI), New York and Norwegian Institute of International Affairs (NUPI), Oslo Co-authors Dr Adriana Erthal Abdenur, Igarapé Institute, Rio de Janeiro, Brazil Prof. Tomas Mandrup, Stellenbosch University, South Africa, and Royal Danish Defence College, Copenhagen Aaron Pangburn, Social Science Research Council (SSRC), New York Data Contributors Ryan Rappa and Paul von Chamier, Center on International Cooperation (CIC), New York University, New York EPON Series Editor Dr Cedric de Coning, NUPI External Reference Group Dr Tatiana Carayannis, SSRC, New York Lisa Sharland, Australian Strategic Policy Institute, Canberra Dr Charles Hunt, Royal Melbourne Institute of Technology (RMIT) University, Australia Adam Day, Centre for Policy Research, UN University, New York Cover photo: UN Photo/Sylvain Liechti UN Photo/ Abel Kavanagh Contents Acknowledgements 5 Acronyms 7 Executive Summary 13 Te effectiveness of the UN Missions in the DRC across eight critical dimensions 14 Strategic and Operational Impact of the UN Missions in the DRC 18 Constraints and Challenges of the UN Missions in the DRC 18 Current Dilemmas 19 Introduction 21 Section 1. -

Deforestation and Forest Degradation Activities in the DRC
E4838 V5 DEMOCRATIC REPUBLIC OF THE CONGO MINISTRY FOR THE ENVIRONMENT, NATURE CONSERVATION AND TOURISM Public Disclosure Authorized STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ PROCESS Public Disclosure Authorized BASELINE REPORT STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ Public Disclosure Authorized PROCESS Public Disclosure Authorized October 2014 STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ PROCESS in the DRC INDEX OF REPORTS Environmental Analysis Document Assessment of Risks and Challenges REDD+ National Strategy of the DRC Strategic Environmental and Social Assessment Report (SESA) Framework Document Environmental and Social Management Framework (ESMF) O.P. 4.01, 4.04, 4.37 Policies and Sector Planning Documents Pest and Pesticide Cultural Heritage Indigenous Peoples Process Framework Management Management Planning Framework (FF) Resettlement Framework Framework (IPPF) O.P.4.12 Policy Framework (PPMF) (CHMF) O.P.4.10 (RPF) O.P.4.09 O.P 4.11 O.P. 4.12 Consultation Reports Survey Report Provincial Consultation Report National Consultation of June 2013 Report Reference and Analysis Documents REDD+ National Strategy Framework of the DRC Terms of Reference of the SESA October 2014 Strategic Environmental and Social Assessment SESA Report TABLE OF CONTENTS Introductory Note ........................................................................................................................................ 9 1. Preface ............................................................................................................................................ -
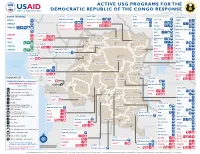
ACTIVE USG PROGRAMS for the DEMOCRATIC REPUBLIC of the CONGO RESPONSE Last Updated 07/27/20
ACTIVE USG PROGRAMS FOR THE DEMOCRATIC REPUBLIC OF THE CONGO RESPONSE Last Updated 07/27/20 BAS-UELE HAUT-UELE ITURI S O U T H S U D A N COUNTRYWIDE NORTH KIVU OCHA IMA World Health Samaritan’s Purse AIRD Internews CARE C.A.R. Samaritan’s Purse Samaritan’s Purse IMA World Health IOM UNHAS CAMEROON DCA ACTED WFP INSO Medair FHI 360 UNICEF Samaritan’s Purse Mercy Corps IMA World Health NRC NORD-UBANGI IMC UNICEF Gbadolite Oxfam ACTED INSO NORD-UBANGI Samaritan’s WFP WFP Gemena BAS-UELE Internews HAUT-UELE Purse ICRC Buta SCF IOM SUD-UBANGI SUD-UBANGI UNHAS MONGALA Isiro Tearfund IRC WFP Lisala ACF Medair UNHCR MONGALA ITURI U Bunia Mercy Corps Mercy Corps IMA World Health G A EQUATEUR Samaritan’s NRC EQUATEUR Kisangani N Purse WFP D WFPaa Oxfam Boende A REPUBLIC OF Mbandaka TSHOPO Samaritan’s ATLANTIC NORTH GABON THE CONGO TSHUAPA Purse TSHOPO KIVU Lake OCEAN Tearfund IMA World Health Goma Victoria Inongo WHH Samaritan’s Purse RWANDA Mercy Corps BURUNDI Samaritan’s Purse MAI-NDOMBE Kindu Bukavu Samaritan’s Purse PROGRAM KEY KINSHASA SOUTH MANIEMA SANKURU MANIEMA KIVU WFP USAID/BHA Non-Food Assistance* WFP ACTED USAID/BHA Food Assistance** SA ! A IMA World Health TA N Z A N I A Kinshasa SH State/PRM KIN KASAÏ Lusambo KWILU Oxfam Kenge TANGANYIKA Agriculture and Food Security KONGO CENTRAL Kananga ACTED CRS Cash Transfers For Food Matadi LOMAMI Kalemie KASAÏ- Kabinda WFP Concern Economic Recovery and Market Tshikapa ORIENTAL Systems KWANGO Mbuji T IMA World Health KWANGO Mayi TANGANYIKA a KASAÏ- n Food Vouchers g WFP a n IMC CENTRAL y i k -

Questions Concerning the Situation in the Republic of the Congo (Leopoldville)
QUESTIONS CONCERNING THE SITUATION IN THE CONGO (LEOPOLDVILLE) 57 QUESTIONS RELATING TO Guatemala, Haiti, Iran, Japan, Laos, Mexico, FUTURE OF NETHERLANDS Nigeria, Panama, Somalia, Togo, Turkey, Upper NEW GUINEA (WEST IRIAN) Volta, Uruguay, Venezuela. A/4915. Letter of 7 October 1961 from Permanent Liberia did not participate in the voting. Representative of Netherlands circulating memo- A/L.371. Cameroun, Central African Republic, Chad, randum of Netherlands delegation on future and Congo (Brazzaville), Dahomey, Gabon, Ivory development of Netherlands New Guinea. Coast, Madagascar, Mauritania, Niger, Senegal, A/4944. Note verbale of 27 October 1961 from Per- Togo, Upper Volta: amendment to 9-power draft manent Mission of Indonesia circulating statement resolution, A/L.367/Rev.1. made on 24 October 1961 by Foreign Minister of A/L.368. Cameroun, Central African Republic, Chad, Indonesia. Congo (Brazzaville), Dahomey, Gabon, Ivory A/4954. Letter of 2 November 1961 from Permanent Coast, Madagascar, Mauritania, Niger, Senegal, Representative of Netherlands transmitting memo- Togo, Upper Volta: draft resolution. Text, as randum on status and future of Netherlands New amended by vote on preamble, was not adopted Guinea. by Assembly, having failed to obtain required two- A/L.354 and Rev.1, Rev.1/Corr.1. Netherlands: draft thirds majority vote on 27 November, meeting resolution. 1066. The vote, by roll-call was 53 to 41, with A/4959. Statement of financial implications of Nether- 9 abstentions, as follows: lands draft resolution, A/L.354. In favour: Argentina, Australia, Belgium, Bolivia, A/L.367 and Add.1-4; A/L.367/Rev.1. Bolivia, Congo Brazil, Cameroun, Canada, Central African Re- (Leopoldville), Guinea, India, Liberia, Mali, public, Chad, Chile, China, Colombia, Congo Nepal, Syria, United Arab Republic: draft reso- (Brazzaville), Costa Rica, Dahomey, Denmark, lution and revision. -

Le Président Du Conseil De Sécurité Présente
Le Président du Conseil de sécurité présente ses compliments aux membres du Conseil et a l'honneur de transmettre, pour information, le texte d'une lettre datée du 2 juin 2020, adressée au Président du Conseil de sécurité, par le Groupe d’experts sur la République démocratique du Congo reconduit suivant la résolution 2478 (2019) du Conseil de sécurité, ainsi que les pièces qui y sont jointes. Cette lettre et les pièces qui y sont jointes seront publiées comme document du Conseil de sécurité sous la cote S/2020/482. Le 2 juin 2020 The President of the Security Council presents his compliments to the members of the Council and has the honour to transmit herewith, for their information, a copy of a letter dated 2 June 2020 from the Group of Experts on the Democratic Republic of the Congo extended pursuant to Security Council resolution 2478 (2019) addressed to the President of the Security Council, and its enclosures. This letter and its enclosures will be issued as a document of the Security Council under the symbol S/2020/482. 2 June 2020 UNITED NATIONS NATIONS UNIES POSTAL ADDRESS-ADRESSE POSTALE: UNITED NATIONS, N.Y. 10017 CABLE ADDRESS -ADRESSE TELEGRAPHIQUE: UNATIONS NEWYORK REFERENCE: S/AC.43/2020/GE/OC.171 2 juin 2020 Monsieur Président, Les membres du Groupe d’experts sur la République démocratique du Congo, dont le mandat a été prorogé par le Conseil de sécurité dans sa résolution 2478 (2019), ont l’honneur de vous faire parvenir leur rapport final, conformément au paragraphe 4 de ladite résolution. -

Cycles Approved by OHRM for S
Consolidated list of duty stations approved by OHRM for rest and recuperation (R & R) (as of 1 July 2015) Duty Station Frequency R & R Destination AFGHANISTAN Entire country 6 weeks Dubai ALGERIA Tindouf 8 weeks Las Palmas BURKINA FASO Dori 12 weeks Ouagadougou BURUNDI Bujumbura, Gitega, Makamba, Ngozi 8 weeks Nairobi CENTRAL AFRICAN REPUBLIC Entire country 6 weeks Yaoundé CHAD Abeche, Farchana, Goré, Gozbeida, Mao, N’Djamena, Sarh 8 weeks Addis Ababa COLOMBIA Quibdo 12 weeks Bogota COTE D’IVOIRE Entire country except Abidjan and Yamoussoukro 8 weeks Accra DEMOCRATIC REPUBLIC OF THE CONGO Aru, Beni, Bukavu, Bunia, Butembo, Dungu, Goma, Kalemie, Mahagi, Uvira 6 weeks Entebbe Bili, Bandundu, Gemena, Kamina, Kananga, Kindu, Kisangani, Matadi, Mbandaka, Mbuji-Mayi 8 weeks Entebbe Lubumbashi 12 weeks Entebbe DEMOCRATIC PEOPLE’S REPUBLIC OF KOREA Pyongyang 8 weeks Beijing ETHIOPIA Kebridehar 6 weeks Addis Ababa Jijiga 8 weeks Addis Ababa GAZA Gaza (entire) 8 weeks Amman GUINEA Entire country 6 weeks Accra HAITI Entire country 8 weeks Santo Domingo INDONESIA Jayapura 12 weeks Jakarta IRAQ Baghdad, Basrah, Kirkuk, Dohuk 4 weeks Amman Erbil, Sulaymaniah 8 weeks Amman KENYA Dadaab, Wajir, Liboi 6 weeks Nairobi Kakuma 8 weeks Nairobi KYRGYZSTAN Osh 8 weeks Istanbul LIBERIA Entire country 8 weeks Accra LIBYA Entire country 6 weeks Malta MALI Gao, Kidal, Tesalit 4 weeks Dakar Tombouctou, Mopti 6 weeks Dakar Bamako, Kayes 8 weeks Dakar MYANMAR Sittwe 8 weeks Yangon Myitkyina (Kachin State) 12 weeks Yangon NEPAL Bharatpur, Bidur, Charikot, Dhunche, -

TERMS of REFERENCE Air OPS Assistant DUTY STATION
Nations Unies FUNDAMENTAL VALUES: INTEGRITY, PROFESSIONALISM, RESPECT FOR DIVERSITY TERMS OF REFERENCE Air OPS Assistant DUTY STATION: Democratic Republic of Congo Bandundu Beni Bunia Bukavu Dungu Gemena Goma Kalemie Kamina Kananga Kindu Kinshasa Kisangani Lubumbashi Mbandaka TYPE OF CONTRACT: Individual Consultant (IC) LENGTH OF CONTRACT: XXXX to 15 January 2019 Administrative structure and reporting: This position is located in the Mission Support Division the United Nations Organization Stabilization Mission in the Democratic Republic of Congo (MONUSCO), across multiple duty stations. The incumbent will be deployed to one of the above MONUSCO operational hubs for the elections. The United Nations Security Council Resolution 2348 (2017) refocused the mandate of MONUSCO from a broader mandate to the support to the protection of civilians and the support to the electoral process. On the 5 November 2017, the electoral calendar was published by the Independent National Electoral Commission (CENI), which identified a number of enablers, including logistics support from MONUSCO. The incumbent will be part of Mission Support Division and will report to the Chief Logistics Officer (Elections), or his or her designate for day to day operations, and for functional coordination the incumbents will work closely with the Chief Aviation Officer. Responsibilities: • Assists in coordinating routine (regular passenger/cargo, logistics resupply) flights, special (casualty and medical evacuation, VIP) flights, and other operational flights in support of the elections. • Assists in flight following and coordinating the integrated search and rescue operations for UN air assets. • Assists in coordinating diplomatic over flight/landing clearances, ground handling support and hotel accommodation/meal/transportation arrangements for aircrews. -

The Evolution of an Armed Movement in Eastern Congo Rift Valley Institute | Usalama Project
RIFT VALLEY INSTITUTE | USALAMA PROJECT UNDERSTANDING CONGOLESE ARMED GROUPS FROM CNDP TO M23 THE EVOLUTION OF AN ARMED MOVEMENT IN EASTERN CONGO rift valley institute | usalama project From CNDP to M23 The evolution of an armed movement in eastern Congo jason stearns Published in 2012 by the Rift Valley Institute 1 St Luke’s Mews, London W11 1Df, United Kingdom. PO Box 30710 GPO, 0100 Nairobi, Kenya. tHe usalama project The Rift Valley Institute’s Usalama Project documents armed groups in the Democratic Republic of the Congo. The project is supported by Humanity United and Open Square and undertaken in collaboration with the Catholic University of Bukavu. tHe rift VALLEY institute (RVI) The Rift Valley Institute (www.riftvalley.net) works in Eastern and Central Africa to bring local knowledge to bear on social, political and economic development. tHe AUTHor Jason Stearns, author of Dancing in the Glory of Monsters: The Collapse of the Congo and the Great War of Africa, was formerly the Coordinator of the UN Group of Experts on the DRC. He is Director of the RVI Usalama Project. RVI executive Director: John Ryle RVI programme Director: Christopher Kidner RVI usalama project Director: Jason Stearns RVI usalama Deputy project Director: Willy Mikenye RVI great lakes project officer: Michel Thill RVI report eDitor: Fergus Nicoll report Design: Lindsay Nash maps: Jillian Luff printing: Intype Libra Ltd., 3 /4 Elm Grove Industrial Estate, London sW19 4He isBn 978-1-907431-05-0 cover: M23 soldiers on patrol near Mabenga, North Kivu (2012). Photograph by Phil Moore. rigHts: Copyright © The Rift Valley Institute 2012 Cover image © Phil Moore 2012 Text and maps published under Creative Commons license Attribution-Noncommercial-No Derivative www.creativecommons.org/licenses/by/nc-nd/3.0. -

ICV20 Lupant.Pub
Emblems of the State of Katanga (1960-1963) Michel Lupant On June 30 1960 the Belgian Congo became the Republic of Congo. At that time Ka- tanga had 1,654,000 inhabitants, i.e. 12.5% of the population of the Congo. On July 4 the Congolese Public Force (in fact the Army) rebelled first in Lower-Congo, then in Leopoldville. On July 8 the mutiny reached Katanga and some Europeans were killed. The leaders of the rebels were strong supporters of Patrice Lumumba. Faced with that situation on July 11 1960 at 2130 (GMT), Mr. Tschombe, Ka- tanga’s President, delivered a speech on a local radio station. He reproached the Cen- tral government with its policies, specially the recruitment of executives from commu- nist countries. Because of the threats of Katanga submitting to the reign of the arbitrary and the communist sympathies of the central government, the Katangese Government decided to proclaim the independence of Katanga.1 At that time there was no Katan- gese flag. On July 13 President Kasa Vubu and Prime Minister Lumumba tried to land at Elisabethville airport but they were refused permission to do so. Consequently, they asked United Nations to put an end to the Belgian agression. On July 14 the Security Council of the United Nations adopted a resolution asking the Belgian troops to leave the Congo, and therefore Katanga. Mr. Hammarskjöld, Secretary-General, considered the United Nations forces had to enter Katanga. Mr. Tschombe opposed that interpreta- tion and affirmed that his decision would be executed by force it need be.