Triple Arthrodesis with Internal and External Fixation: Technique Paper
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tibiocalcaneal Arthrodesis Using Screws in the Treatment of Equinovarus Deformity of the Foot in Adult: a Retrospective Study of 42 Cases L.Unyendje, M
14699 L.Unyendje et al./ Elixir Human Physio. 58 (2013) 14699-14702 Available online at www.elixirpublishers.com (Elixir International Journal) Human Physiology Elixir Human Physio. 58 (2013) 14699-14702 Tibiocalcaneal arthrodesis using screws in the treatment of equinovarus deformity of the foot in adult: a retrospective study of 42 cases L.Unyendje, M. Mahfoud, F.Ismael, A.Karkazan, MS. Berrada, M. EL Yaacoubi, A. El Bardouni, M. Kharmaz, MY.O.Lamrani, M.Ouadghiri and A. Lahlou Mohammed V University, Faculty of Medicine and Pharmacy, IBN SINA Hospital, Orthopedic Department Rabat-Morocco. ARTICLE INFO ABSTRACT Article history: The authors have retrospectively studied 42 cases of tibiocalcaneal arthrodesis using large Received: 6 March 2013; cannulated AO screws, staples and iliac crest graft mixed in treatment of fixed equinovarus Received in revised form: deformity of the foot in adult patients. There were 25 men and 17 women aged 22 to 70 17 April 2013; (mean, 45) years. All patients were reviewed with an average of 5 years. The operations Accepted: 3 May 2013; were performed between 2005 and 2012.Preoperatively, all patients had 50° of the mean calcaneal varus deformity and 75° (60-90°) of equinus deformity on Meary’s radiological. Keywords There were 24 idiopathic, 8 post traumatic,6 neurologic associated with IMC,4 polio. Tibiocalcaneal arthrodesis, Clinical and functional outcome was assessed with the kitaoka score, the x-rays included an Screw, AP and lateral view of the ankle and Meary view .Resultats were excellent in 73% , good in Equinovarus foot, 18 % , fair in 9%. X-rays showed 3 nonunions after 2 years and were reported. -

Ankle and Pantalar Arthrodesis
ANKLE AND PANTALAR ARTHRODESIS George E. Quill, Jr., M.D. In: Foot and Ankle Disorders Edited by Mark S. Myerson, M.D. Since reports in the late 19th Century, arthrodesis has been a successful accepted treatment method for painful disorders of the ankle, subtalar, and transverse tarsal joints. While the title of this chapter involves arthrodesis - the intentional fusion of a joint - as a form of reconstruction, this chapter will address not only surgical technique, but nonoperative methods of care as well. We will address the pathophysiology leading to ankle and hindfoot disability, succinctly review the existing literature on the topic of hindfoot and ankle arthrodesis, highlight the pathomechanics involved, and spend considerable time on establishing the diagnosis, indications, and preoperative planning when surgery is indicated. We also will discuss the rehabilitation of the postoperative patient, as well as the management of complications that may arise after ankle and pantalar arthrodesis. There are more than thirty different viable techniques that have been described in order to achieve successful ankle and hindfoot arthrodesis. It is not the purpose of this chapter to serve as compendium of all the techniques ever described. The author will, rather, attempt to distill into a useful amount of clinically applicable material this vast body of information that the literature and clinical experience provide. Ankle arthrodesis is defined as surgical fusion of the tibia to the talus. Surgical fusion of the ankle (tibiotalar) and subtalar (talocalcaneal) joints at the same operative sitting is termed tibiotalocalcaneal arthrodesis. Fusion of the talus to all the bones articulating with it (distal tibia, calcaneus, navicular, and cuboid) is termed pantalar arthrodesis. -
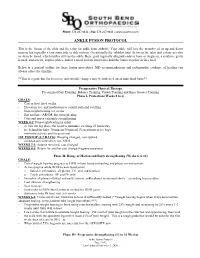
Ankle Fusion Protocol
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -
Consensus of the 3 Round Table Barcelona June 2013
Consensus of the 3rd Round Table Barcelona June 2013 Mark Rogers FRCS (Tr & Orth) Derek Park FRCS (Tr & Orth) Dishan Singh FRCS (Orth) Aspects of Orthopaedic Foot & Ankle Surgery Preface The 1st Round Table meeting was held in Padua in June 2011, followed by the 2nd Round Table meeting in Paris in June 2012. The 3rd Round Table in Barcelona in June 2013 has once again followed a format where all attendees review the literature and present their individual experience on a topic with ample time for an informal discussion of the subject. There is no distinction between faculty and delegates. Mark Rogers and Derek Park were responsible for recording opinions and capturing the essence of the debates, many of which resulted in consensus being reached on areas of foot and ankle practice. This booklet collates the literature review and the views of all those who participated. The opinions on consent, particularly, will hopefully guide practice and form the basis for a wider discussion at BOFAS. This booklet does not represent Level 1 evidence derived from prospective randomized controlled trials but represents the compilation of anecdotal reports and small case studies based on the combined experience of 34 British orthopaedic surgeons as well as Judith Baumhauer from the USA and Harvinder Bedi from Australia. I hope that you will find something of use and relevant to your own practice. Dishan Singh, MBChB, FRCS, FRCS (Orth) Consultant Orthopaedic Surgeon Royal National Orthopaedic Hospital Stanmore, UK Consensus of the 3rd Round Table Barcelona 2013 Mark Rogers Derek Park Dishan Singh Aspects of Orthopaedic Foot & Ankle Surgery 1. -

Triple Arthrodesis
DR JEFF LING MBBS BSc (Med) FRACS (Orth) Adult and Paediatric Orthopaedic Surgeon Specialising in the Foot and Ankle Triple Arthrodesis INTRODUCTION Triple arthrodesis (fusion) involves fusing 3 joints, hence the use of the term “triple”. The 3 joints are the “subtalar joint”, the “calcaneocuboid joint”, and the “talonavicular joint”. The indications for this operation include correction of a fixed cavovarus deformity (See Information Sheet on Cavovarus Foot Reconstruction) or a fixed flatfoot deformity (See Information Sheet on Flatfoot Correction), or end-stage arthritis. After a triple arthrodesis, most patients are much more comfortable and have an improved quality of life. THE PROCEDURE There are a number of steps to this procedure: 1. General Anaesthetic 2. Administration of intravenous antibiotics 3. Nerve block at knee for post-operative pain relief 4. Bone graft taken from small 1cm incision at side of heel 5. Incisions made over subtalar joint/calcaneocuboid joint/talonavicular joint and diseased cartilage removed 6. Bone graft and growth hormone inserted into joints to stimulate fusion 7. Above joints held in appropriate position and stabilized with screws and staples 8. Intra-operative check xray 9. Wound Closure with sutures 10. Plaster Backslab RISKS & COMPLICATIONS Every surgical procedure carries some risk. These risks are largely uncommon and many are rare. They include: Anaesthetic complications Drug reactions Wound infection Deep Vein Thrombosis (DVT)/Pulmonary embolism (PE) Sensory nerve injury Chronic Regional Pain -

Approved Surgical Procedures
UNION MEDICAL BENEFITS SOCIETY LTD APPROVED SURGICAL PROCEDURES The following list of surgical procedures should be read in conjunction with your policy document. If you are intending to have one of the listed procedures, please call our surgical team on 0800 600 666 so we can guide you through the prior approval process. If a surgical procedure is not listed below, it will not be covered unless UniMed decides, in its sole discretion, to offer cover. CARDIAC GENERAL • Pericardiotomy Breast • Pericardiocentesis • Breast Cyst Aspiration or Needle Biopsy • Drainage of Pericaridal Effusion • Breast Biopsy • Coronary Artery Bypass (using vein or artery) • Core Biopsy of Breast • Open Repair of Atrial Septal Defect (ASD) • Excision Accessary Breast Tissue • Valvuloplasty • Mastectomy • Aortic/ Mitral Valve Replacement via Sternotomy • Sentinel Node Biopsy with/without Axillary Dissection • Pulmonary Valve Replacement via Sternotomy • Breast Microdochotomy • Tricuspid Valve Replacement via Sternotomy • Balloon Valvuloplasty – Mitral/ Aortic Reconstruction Post Mastectomy • Pacemaker Surgery – Initial Implantation (Excluding the Cost • Breast/ Nipple Reconstruction of the Pacemaker) • Nipple Areolar Tattoo • Removal of Sternal Wire • Maze Arrhythmia Surgery Gastrointestinal • Removal & Rewiring of Sternal Wire • Anal Sphincterotomy • Maze Arrhythmia Surgery (Standalone procedure) • Simple Repair of Anal Fistula – Special approval only • Maze Procedure – Thoracoscopic • Anal Fistula Repair with Mucosal Advancement Flap • Bentall’s Procedure (includes -

John Shirk Kirchner, M.D. Curriculum Vitae
JOHN SHIRK KIRCHNER, M.D. CURRICULUM VITAE OFFICE ADDRESS: MedPlex Medical Building 4517 Southlake Parkway Hoover, Alabama 35244 205.985.4111 Southlakeorthopaedics.com Grandview Physicians Plaza 3686 Grandview Parkway, Suite 430 Birmingham, Alabama 35243 205.605.8180 CREDENTIALS AND LICENSURE: ABOS Board Certified 2001, re-certification 2011 NBME Diplomat Alabama – 1997 – Present Pennsylvania – 1995 – 2002 MEMBERSHIPS AND COMMITEES: Fellow in the American Academy of Orthopaedic Surgeons Foot & Ankle Evaluation Subcommittee of the AAOS (2000-2008) AOFAS AAOFAS Mid-America Orthopaedic Society American College of Sports Medicine Medical Association of the State of Alabama Alabama Orthopaedic Society Jefferson County Medical Society UNDERGRADUATE EDUCATION: The Hill School, Pottstown, PA Diploma – May 20, 1984 Washington and Lee University, Lexington, VA B.A. in Chemistry (Cum Laude) – June 2, 1988 1 MEDICAL EDUCATION: Hahnemann University, Philadelphia, PA M.D. – June 1992 POSTGRADUATE EDUCATION: Internship General Surgery, Hahnemann University Hospital, Philadelphia, PA July 1, 1992 – June 30, 1993 Residency Orthopaedic Surgery, Allegheny University of the Health Sciences, Philadelphia, PA July 1, 1993 – June 30, 1997 Fellowship Foot and Ankle Surgery, American Sports Medicine Institute, Birmingham, AL August 1, 1997 – July 31, 1998 EMPLOYMENT: Southlake Orthopaedics Sports Medicine & Spine Center, PC, Birmingham AL. November 2015 – present Assistant Professor, University of Alabama Birmingham, Department of Surgery, Division of Orthopaedic -

Computational Simulations of Biomechanical Kinematics in WSU Total Ankle Replacement Systems
Wright State University CORE Scholar Browse all Theses and Dissertations Theses and Dissertations 2017 Computational Simulations of Biomechanical Kinematics in WSU Total Ankle Replacement Systems Dinesh Gundapaneni Wright State University Follow this and additional works at: https://corescholar.libraries.wright.edu/etd_all Part of the Engineering Commons Repository Citation Gundapaneni, Dinesh, "Computational Simulations of Biomechanical Kinematics in WSU Total Ankle Replacement Systems" (2017). Browse all Theses and Dissertations. 1885. https://corescholar.libraries.wright.edu/etd_all/1885 This Thesis is brought to you for free and open access by the Theses and Dissertations at CORE Scholar. It has been accepted for inclusion in Browse all Theses and Dissertations by an authorized administrator of CORE Scholar. For more information, please contact [email protected]. COMPUTATIONAL SIMULATIONS OF BIOMECHANICAL KINEMATICS IN WSU TOTAL ANKLE REPLACEMENT SYSTEMS A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy By DINESH GUNDAPANENI B.Tech., Sathyabama University, India, 2010 M.S.E.G, Wright State University, 2012 _________________________________________________ 2017 Wright State University WRIGHT STATE UNIVERSITY GRADUATE SCHOOL DECEMBER 08, 2017 I HEREBY RECOMMEND THAT THE DISSERTATION PREPARED UNDER MY SUPERVISION BY Dinesh Gundapaneni ENTITLED Computational Simulations of Biomechanical Kinematics in WSU Total Ankle Replacement Systems BE ACCEPTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF Doctor of Philosophy. ___________________________________ Tarun Goswami, D.Sc. Dissertation Director ___________________________________ Frank W. Ciarallo, Ph.D. Director, Ph.D. Engineering ___________________________________ Barry Milligan, Ph.D. Interim Dean of the Graduate School Committee on Final Examination ________________________________ Tarun Goswami, D.Sc. ________________________________ Jennie J. -

Midterm Follow-Up of Talectomy for Severe Rigid Equinovarus Feet
The Journal of Foot & Ankle Surgery 54 (2015) 1093–1098 Contents lists available at ScienceDirect The Journal of Foot & Ankle Surgery journal homepage: www.jfas.org Midterm Follow-Up of Talectomy for Severe Rigid Equinovarus Feet Mostafa H. El-Sherbini, MD, PhD 1, Ahmed A. Omran, MD, MSc 2 1 Assistant Professor, Department of Orthopaedics, National Institute of Neuromotor System (NINMS, GOTHI), Imbaba, Giza, Great Cairo, Egypt 2 Senior Specialist, Department of Orthopaedics, National Institute of Neuromotor System (NINMS, GOTHI), Imbaba, Giza, Great Cairo, Egypt article info abstract Level of Clinical Evidence: 4 Rigid equinovarus foot is a challenging problem. Talectomy has been advocated as a salvage procedure to achieve a plantigrade painless foot in the treatment of rigid equinovarus deformity. The present prospective Keywords: arthrogryposis observational study evaluated the effectiveness of talectomy in the treatment of Dimeglio grade IV rigid calcaneal osteotomy equinovarus feet. Nineteen feet in 13 patients were treated by talectomy from September 2001 through Dimeglio grade January 2012 (10-year, 2-month period). Of the 13 patients, 9 (69.23%) had a foot deformity due to arthrog- equinovarus deformity ryposis multiplex congenita and 1 (7.69%) each due to sacral agenesis, spastic cerebral palsy, neglected navicular excision congenital talipes equinovarus, and post-traumatic contracture. Of the 13 patients, 9 (69.23%) were male and 4 (30.77%) were female. Their mean age was 7.7 (range 3 to 26) years. The mean follow-up duration was 6.4 (range 2 to 11) years. Along with talectomy, excision of the navicular was performed in 8 feet (42.11%), calcaneal osteotomy with a laterally based wedge in 8 (42.11%), and calcaneocuboid fusion in 3 feet (15.79%). -

TIBIOTALOCALCANEAL and PANTALAR ARTHRODESIS Foot
TIBIOTALOCALCANEAL AND PANTALAR ARTHRODESIS Foot and Ankle Clinics Author: George E. Quill, Jr., M.D. Since the report by Albert in 1882, arthrodesis has been an accepted treatment for painful arthritis of the ankle and subtalar joints.3 For the purpose of this and other orthopaedic articles, surgical fusion of the ankle (tibiotalar) and subtalar (talocalcaneal) joints at the same operative sitting will be termed tibiotalocalcaneal arthrodesis. Fusion of the talus to all the bones articulating with it (distal tibia, calcaneus, tarsonavicular, and cuboid) is termed pantalar arthrodesis.13,20 Numerous techniques exist describing fusion approaches and implants, all having in common a similar goal: a solid, pain free arthrodesis in a biomechanically stable and functional position.1-31 The indications for tibiotalocalcaneal arthrodesis include avascular necrosis of the talus or a failed total ankle arthroplasty with subtalar intrusion.14,16,20,21 The failed ankle fusion with insufficient talar body, as well as patients with rheumatoid or osteoarthritic involvement of these joints are also candidates for tibiotalocalcaneal fusion.8,16,23,25,30 Other indications include the sequelae of trauma and the severe deformity of untreated clubfoot and neuromuscular disease.5,7,20,23,24 Patients with Charcot arthropathy, skeletal defects after tumor reconstruction, pseudarthrosis, as well as fixed and various flail deformities about the hindfoot and ankle are also candidates for tibiotalocalcaneal and, in certain instances, pantalar arthrodesis.4,9,18,20,22,27,28 -

Triple Arthrodesis Following Your Consultation You Are Considering a Triple Arthrodesis Otherwise Known As a Triple Fusion (Or Variation of This Procedure)
Triple Arthrodesis Following your consultation you are considering a triple arthrodesis otherwise known as a triple fusion (or variation of this procedure). This section aims to give you additional information about your condition and the treatment. It is designed to give you some general details about the recovery from surgery if necessary and the common risks and complications. This section is not for self-diagnosis. Please ask your surgeon if you have any further questions. What is it? This is an operation to “fuse” or stiffen the three main joints of the back part of the foot (hence “triple fusion”). Why would it be performed? Triple fusions are performed for two main reasons: - Arthritis of the joints. Because of a previous injury that has damaged the joints, a generalised condition such as osteoarthritis or rheumatoid arthritis or because the joint is just wearing out for some other reason. - Severe deformity of the foot such as a flat foot, high-arched or “cavus” foot, a club foot or other deformity. Sometimes, these can be corrected by breaking and reshaping the bones, but, in other cases, it is best to stiffen the joints in the corrected position, particularly if the joints are already stiff or the foot is weak. If the damage or deformity is limited to 1 or 2 of the foot joints, it may be possible to treat it by a more limited operation. However, as these joints work together, damage to one is often accompanied by damage to others. We often inject local anaesthetic or steroid into damaged joints before surgery is considered, to see whether this helps ease the pain. -

REARFOOT ARTHRODESIS: the Podiatry Institute Technique
CHAPTER 4 REARFOOT ARTHRODESIS: The Podiatry Institute Technique Gerard V, Yu, D.P.M. In 7923, Ryerson introduced the procedure known literature has emphasized the complications of today as triple arthrodesis. At that time he sought residual deformity or recuffence of deformity, few an alternative procedure which would produce have emphasized steps which should be taken to satisfying long term results in patients affected by avoid these complications. Consequently triple infantile paralysis or similar disabilities. Since that arthrodesis has often been viewed as a "salvage time there has been a divergence of opinion procedure." regarding many aspects of triple arthrodesis. Over the years, The Podiatry Institute has However, its indication for the management of consistently searched for ways to improve both the painful conditions in the hindfoot has nor been techniques and the end results of triple afihrodesis, disputed. Surgeons agree that single, double or as well as isolated or double joint fusions in the triple joint arthrodesis of the foor have many indi- hindfoot. Because of the continuing efforts of The cations. These include traumatic or degenerative Podiatry Institute facuhy, triple afthrodesis has arthritic changes of the joints, malalignment of the become a very suitable and reliable means of foot, such as seen with a valgus or varus foot stabilizing the foot, thus providing longJasting deformity, or gross instability of the same joints. improved function. Any rearfoot fusion entails There are numerous conditions which can result in significant complexity; many factors must be deformities necessitating rearfoot fusion including constantly assessed and reassessed preoperatively, tarsal coalitions, congenital vertical talus, systemic intraoperatively, and postoperatively in order to arthritis, and neuromuscular diseases such as achieve the desired outcome.