Early Clinical Results of the BOX Ankle Replacement Are Satisfactory: a Multicenter Feasibility Study of 158 Ankles
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Vantage Total Ankle Replacement
Total Ankle Replacement Find out why the Exactech Ankle may be right for you. UNDERSTANDING ANKLE REPLACEMENT This brochure offers a brief overview of ankle anatomy, arthritis and ankle replacement. This information is for educational purposes only and is not intended to replace the expert guidance of your physician. Please direct any questions or concerns you may have to your doctor. 02 ANKLE ARTHRITIS YOUR ANKLE Your ankle is made up of a variety of bones, ligaments, tendons and cartilage that connect at the junction of your leg and foot. The joint works like a hinge and is responsible for moving your foot up and down. The tibia (shinbone), talus and fibula (smaller bone in the lower leg) are the bones that construct the ankle joint. Your ligaments border these bones on either side, holding them together to provide stability. Meanwhile the tendons connect the muscles to the bone and are responsible for the ankle and toe movements. Covering your bones is a smooth substance called cartilage, which acts as a cushion to reduce the friction between your bones as they move. If your cartilage wears down, arthritis can develop and cause loss of motion and pain. TIBIA FIBULA TALUS CALCANEUS METATARSAL V 03 ARTHRITIC ANKLE HEALTHY ANKLE Nearly half of individuals over the age of 60 have foot or ankle arthritis. 04 ARTHRITIS Nearly half of individuals over the age of 60 have foot or ankle arthritis that may not cause symptoms.1 However, for those suffering from ankle arthritis pain the most reported causes are:2 • Rheumatoid arthritis - It is an autoimmune disease that attacks multiple joints and typically starts in the hands and feet. -
Joint Replacement Surgery Table of Contents
Everything You Want to Know About Joint Replacement Surgery Table of Contents Understanding Your Joints: PG.3 How, when and why joint pain occurs Diagnosing Joint Pain: PG.4 The most common conditions and injuries Exploring the Options: PG.5 A look at partial and total joint replacement Seeing What’s New: PG.6 Medical advances in joint replacement surgery Answering Your Questions: PG.7 A discussion with Dr. Donald Hohman, Joint Replacement Program Medical Director Learning More: PG.9 Connecting with Texas Health Center for Diagnostics and Surgery Getting Ready: PG.10 My questions about joint replacement surgery Texas Health Center for Diagnostics & Surgery is a joint venture owned by Texas Health Resources and physicians dedicated to the community and meets the definition under federal law of physician-owned hospital. Physicians on the medical staff practice independently and are not employees or agents of the hospital. PAGE 2 Understanding Your Joints: How, when and why joint pain occurs Healthy joints aren’t just necessary for performing the physical activities we enjoy. They are the mechanical instruments that make virtually every movement possible. When our joints begin to succumb to years of natural wear and tear or degenerative conditions like arthritis, even the most common movements — like walking or climbing stairs — can become painful. Left untreated, joint pain can be potentially debilitating, severely diminishing one’s quality of life. New hope for joint pain Here’s the good news: it is possible to significantly reduce joint pain. Medical advancements in joint surgery have come a long way, particularly partial and total joint replacement. -

Tibiocalcaneal Arthrodesis Using Screws in the Treatment of Equinovarus Deformity of the Foot in Adult: a Retrospective Study of 42 Cases L.Unyendje, M
14699 L.Unyendje et al./ Elixir Human Physio. 58 (2013) 14699-14702 Available online at www.elixirpublishers.com (Elixir International Journal) Human Physiology Elixir Human Physio. 58 (2013) 14699-14702 Tibiocalcaneal arthrodesis using screws in the treatment of equinovarus deformity of the foot in adult: a retrospective study of 42 cases L.Unyendje, M. Mahfoud, F.Ismael, A.Karkazan, MS. Berrada, M. EL Yaacoubi, A. El Bardouni, M. Kharmaz, MY.O.Lamrani, M.Ouadghiri and A. Lahlou Mohammed V University, Faculty of Medicine and Pharmacy, IBN SINA Hospital, Orthopedic Department Rabat-Morocco. ARTICLE INFO ABSTRACT Article history: The authors have retrospectively studied 42 cases of tibiocalcaneal arthrodesis using large Received: 6 March 2013; cannulated AO screws, staples and iliac crest graft mixed in treatment of fixed equinovarus Received in revised form: deformity of the foot in adult patients. There were 25 men and 17 women aged 22 to 70 17 April 2013; (mean, 45) years. All patients were reviewed with an average of 5 years. The operations Accepted: 3 May 2013; were performed between 2005 and 2012.Preoperatively, all patients had 50° of the mean calcaneal varus deformity and 75° (60-90°) of equinus deformity on Meary’s radiological. Keywords There were 24 idiopathic, 8 post traumatic,6 neurologic associated with IMC,4 polio. Tibiocalcaneal arthrodesis, Clinical and functional outcome was assessed with the kitaoka score, the x-rays included an Screw, AP and lateral view of the ankle and Meary view .Resultats were excellent in 73% , good in Equinovarus foot, 18 % , fair in 9%. X-rays showed 3 nonunions after 2 years and were reported. -

Ankle and Pantalar Arthrodesis
ANKLE AND PANTALAR ARTHRODESIS George E. Quill, Jr., M.D. In: Foot and Ankle Disorders Edited by Mark S. Myerson, M.D. Since reports in the late 19th Century, arthrodesis has been a successful accepted treatment method for painful disorders of the ankle, subtalar, and transverse tarsal joints. While the title of this chapter involves arthrodesis - the intentional fusion of a joint - as a form of reconstruction, this chapter will address not only surgical technique, but nonoperative methods of care as well. We will address the pathophysiology leading to ankle and hindfoot disability, succinctly review the existing literature on the topic of hindfoot and ankle arthrodesis, highlight the pathomechanics involved, and spend considerable time on establishing the diagnosis, indications, and preoperative planning when surgery is indicated. We also will discuss the rehabilitation of the postoperative patient, as well as the management of complications that may arise after ankle and pantalar arthrodesis. There are more than thirty different viable techniques that have been described in order to achieve successful ankle and hindfoot arthrodesis. It is not the purpose of this chapter to serve as compendium of all the techniques ever described. The author will, rather, attempt to distill into a useful amount of clinically applicable material this vast body of information that the literature and clinical experience provide. Ankle arthrodesis is defined as surgical fusion of the tibia to the talus. Surgical fusion of the ankle (tibiotalar) and subtalar (talocalcaneal) joints at the same operative sitting is termed tibiotalocalcaneal arthrodesis. Fusion of the talus to all the bones articulating with it (distal tibia, calcaneus, navicular, and cuboid) is termed pantalar arthrodesis. -

EPO Surgeryplus Plan Amendment
AMENDMENT TO THE COLORADO EMPLOYER BENEFIT TRUST EPO MEDICAL BENEFIT PLAN AND SUMMARY PLAN DESCRIPTION, EFFECTIVE JANUARY 1, 2019 The CEBT EPO Medical Benefit Plan and Summary Plan Description, effective January 1, 2019 (the “Plan”), shall be amended effective July 1, 2019 to include SurgeryPlus Benefits as follows: 1. Medical Covered Expenses: SURGERYPLUS BENEFIT Charges for certain surgeries, procedures, and related travel expenses are payable as shown on the Schedule of Benefits. This plan will pay charges for surgeries, procedures, and related travel as approved by SurgeryPlus for one Episode of Care. The SurgeryPlus benefit terminates upon your discharge from the hospital, ambulatory surgical center, or other facility following the Episode of Care. Any services rendered after the termination of the Episode of Care are subject to the applicable rules of this plan. Travel benefits may be payable if you do not have access to SurgeryPlus surgeons. The travel benefits will be determined by SurgeryPlus based upon the procedure, provider, and geographic distance of the provider in relation to your residence. Travel benefits may also be provided for a companion if your procedure requires inpatient or overnight care. Travel arrangements must be made through your SurgeryPlus Care Advocate for benefits to be payable. Some examples of the surgeries and procedures available through SurgeryPlus, include, but are not limited to the following: Knee: Foot & Ankle: General Surgery: Knee Replacement Ankle Replacement Gallbladder Removal Knee Replacement -
Ankle Fusion Protocol
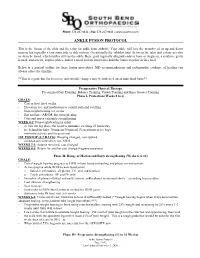
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -
Consensus of the 3 Round Table Barcelona June 2013
Consensus of the 3rd Round Table Barcelona June 2013 Mark Rogers FRCS (Tr & Orth) Derek Park FRCS (Tr & Orth) Dishan Singh FRCS (Orth) Aspects of Orthopaedic Foot & Ankle Surgery Preface The 1st Round Table meeting was held in Padua in June 2011, followed by the 2nd Round Table meeting in Paris in June 2012. The 3rd Round Table in Barcelona in June 2013 has once again followed a format where all attendees review the literature and present their individual experience on a topic with ample time for an informal discussion of the subject. There is no distinction between faculty and delegates. Mark Rogers and Derek Park were responsible for recording opinions and capturing the essence of the debates, many of which resulted in consensus being reached on areas of foot and ankle practice. This booklet collates the literature review and the views of all those who participated. The opinions on consent, particularly, will hopefully guide practice and form the basis for a wider discussion at BOFAS. This booklet does not represent Level 1 evidence derived from prospective randomized controlled trials but represents the compilation of anecdotal reports and small case studies based on the combined experience of 34 British orthopaedic surgeons as well as Judith Baumhauer from the USA and Harvinder Bedi from Australia. I hope that you will find something of use and relevant to your own practice. Dishan Singh, MBChB, FRCS, FRCS (Orth) Consultant Orthopaedic Surgeon Royal National Orthopaedic Hospital Stanmore, UK Consensus of the 3rd Round Table Barcelona 2013 Mark Rogers Derek Park Dishan Singh Aspects of Orthopaedic Foot & Ankle Surgery 1. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Triple Arthrodesis
DR JEFF LING MBBS BSc (Med) FRACS (Orth) Adult and Paediatric Orthopaedic Surgeon Specialising in the Foot and Ankle Triple Arthrodesis INTRODUCTION Triple arthrodesis (fusion) involves fusing 3 joints, hence the use of the term “triple”. The 3 joints are the “subtalar joint”, the “calcaneocuboid joint”, and the “talonavicular joint”. The indications for this operation include correction of a fixed cavovarus deformity (See Information Sheet on Cavovarus Foot Reconstruction) or a fixed flatfoot deformity (See Information Sheet on Flatfoot Correction), or end-stage arthritis. After a triple arthrodesis, most patients are much more comfortable and have an improved quality of life. THE PROCEDURE There are a number of steps to this procedure: 1. General Anaesthetic 2. Administration of intravenous antibiotics 3. Nerve block at knee for post-operative pain relief 4. Bone graft taken from small 1cm incision at side of heel 5. Incisions made over subtalar joint/calcaneocuboid joint/talonavicular joint and diseased cartilage removed 6. Bone graft and growth hormone inserted into joints to stimulate fusion 7. Above joints held in appropriate position and stabilized with screws and staples 8. Intra-operative check xray 9. Wound Closure with sutures 10. Plaster Backslab RISKS & COMPLICATIONS Every surgical procedure carries some risk. These risks are largely uncommon and many are rare. They include: Anaesthetic complications Drug reactions Wound infection Deep Vein Thrombosis (DVT)/Pulmonary embolism (PE) Sensory nerve injury Chronic Regional Pain -

Total Ankle Replacement Postoperative Recovery Protocol Jeffrey Seybold, M.D
Total Ankle Replacement Postoperative Recovery Protocol Jeffrey Seybold, M.D. Twin Cities Orthopedics – Foot and Ankle Surgery Type of Procedure: overnight hospital stay or possible outpatient Length of Procedure: 2 hours Anesthesia: general w/ nerve block Total ankle replacement: what is it? Replacement of the ankle joint is a relatively modern approach to treatment of arthritis in the ankle joint. Instead of fusing or gluing the ankle bones together, a jig is used to cut the bones and secure metal and plastic components that move together like the native ankle joint. This surgery is intended to provide pain relief, restore some motion in the ankle, and allow patients to return to some of their normal activities. The principle benefit of ankle replacement over ankle fusion is keeping some motion in the ankle joint, which may help preserve the other joints in the foot and prevent the development of or worsening arthritis. That said, patients who do not have any motion in their ankle due to arthritis are unlikely to gain motion back after a total ankle replacement. As the technology in total ankle designs has progressed over the past few decades, the length of time a total ankle replacement survives has improved as well. Most studies suggest that 15% of patients will require an additional surgery on their ankle within 10 years of their replacement. That includes anything from replacement of the plastic component, bone grafting cysts that can form around the metal components, completely revising the prosthetic ankle or converting to an ankle fusion, or even amputation. For this reason, I am very careful to offer a total ankle replacement, since the risks of complications or need for a second surgery can be unacceptably high for certain patients, including patients under 50 years of age, patients with diabetes, patients with a heavy labor job or high activity demands for their ankle, patients with previous infections around the ankle, or patients with a lot of deformity around the ankle. -

Treatment of Isolated Ankle Osteoarthritis with Arthrodesis Or the Total Ankle Replacement: a Comparison of Early Outcomes Charles L
Original Article Clinics in Orthopedic Surgery 2010;2:1-7 • doi:10.4055/cios.2010.2.1.1 Treatment of Isolated Ankle Osteoarthritis with Arthrodesis or the Total Ankle Replacement: A Comparison of Early Outcomes Charles L. Saltzman, MD, Robert G. Kadoko, MD*, Jin Soo Suh, MD† Department of Orthopaedic Surgery, University of Utah, Salt Lake City, UT, *Orthopedic Institute of Texas, Hurst, TX, USA, †Department of Orthopaedic Surgery, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea Background: Ankle arthrodesis and replacement are two common surgical treatment options for end-stage ankle osteoarthritis. However, the relative value of these alternative procedures is not well defi ned. This study compared the clinical and radiographic outcomes as well as the early perioperative complications of the two procedures. Methods: Between January 2, 1998 and May 31, 2002, 138 patients were treated with ankle fusion or replacements. Seventy one patients had isolated posttraumatic or primary ankle arthritis. However, patients with infl ammatory arthritis, neuropathic arthritis, concomitant hind foot fusion, revision procedures and two component system ankle replacement were excluded. Among them, one group of 42 patients had a total ankle replacement (TAR), whereas the other group of 29 patients underwent ankle fusion. A complete follow-up could be performed on 89% (37/42) and 73% (23/29) of the TAR and ankle fusion group, respectively. The mean follow-up period was 4.2 years (range, 2.2 to 5.9 years). Results: The outcomes of both groups were compared using a student’s t-test. Only the short form heath survery mental component summary score and Ankle Osteoarthritis Scale pain scale showed significantly better outcomes in the TAR group (p < 0.05). -

Approved Surgical Procedures
UNION MEDICAL BENEFITS SOCIETY LTD APPROVED SURGICAL PROCEDURES The following list of surgical procedures should be read in conjunction with your policy document. If you are intending to have one of the listed procedures, please call our surgical team on 0800 600 666 so we can guide you through the prior approval process. If a surgical procedure is not listed below, it will not be covered unless UniMed decides, in its sole discretion, to offer cover. CARDIAC GENERAL • Pericardiotomy Breast • Pericardiocentesis • Breast Cyst Aspiration or Needle Biopsy • Drainage of Pericaridal Effusion • Breast Biopsy • Coronary Artery Bypass (using vein or artery) • Core Biopsy of Breast • Open Repair of Atrial Septal Defect (ASD) • Excision Accessary Breast Tissue • Valvuloplasty • Mastectomy • Aortic/ Mitral Valve Replacement via Sternotomy • Sentinel Node Biopsy with/without Axillary Dissection • Pulmonary Valve Replacement via Sternotomy • Breast Microdochotomy • Tricuspid Valve Replacement via Sternotomy • Balloon Valvuloplasty – Mitral/ Aortic Reconstruction Post Mastectomy • Pacemaker Surgery – Initial Implantation (Excluding the Cost • Breast/ Nipple Reconstruction of the Pacemaker) • Nipple Areolar Tattoo • Removal of Sternal Wire • Maze Arrhythmia Surgery Gastrointestinal • Removal & Rewiring of Sternal Wire • Anal Sphincterotomy • Maze Arrhythmia Surgery (Standalone procedure) • Simple Repair of Anal Fistula – Special approval only • Maze Procedure – Thoracoscopic • Anal Fistula Repair with Mucosal Advancement Flap • Bentall’s Procedure (includes