Everest and Oxygen—Ruminations by a Climber Anesthesiologist by David Larson, M.D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Physiology an Integrated Approach
Gas Exchange and Transport Gas Exchange in the Lungs and Tissues 18 Lower Alveolar P Decreases Oxygen Uptake O2 Diff usion Problems Cause Hypoxia Gas Solubility Aff ects Diff usion Gas Transport in the Blood Hemoglobin Binds to Oxygen Oxygen Binding Obeys the Law of Mass Action Hemoglobin Transports Most Oxygen to the Tissues P Determines Oxygen-Hb Binding O2 Oxygen Binding Is Expressed As a Percentage Several Factors Aff ect Oxygen-Hb Binding Carbon Dioxide Is Transported in Three Ways Regulation of Ventilation Neurons in the Medulla Control Breathing Carbon Dioxide, Oxygen, and pH Infl uence Ventilation Protective Refl exes Guard the Lungs Higher Brain Centers Aff ect Patterns of Ventilation The successful ascent of Everest without supplementary oxygen is one of the great sagas of the 20th century. — John B. West, Climbing with O’s , NOVA Online (www.pbs.org) Background Basics Exchange epithelia pH and buff ers Law of mass action Cerebrospinal fl uid Simple diff usion Autonomic and somatic motor neurons Structure of the brain stem Red blood cells and Giant liposomes hemoglobin of pulmonary Blood-brain barrier surfactant (40X) From Chapter 18 of Human Physiology: An Integrated Approach, Sixth Edition. Dee Unglaub Silverthorn. Copyright © 2013 by Pearson Education, Inc. All rights reserved. 633 Gas Exchange and Transport he book Into Thin Air by Jon Krakauer chronicles an ill- RUNNING PROBLEM fated trek to the top of Mt. Everest. To reach the summit of Mt. Everest, climbers must pass through the “death zone” T High Altitude located at about 8000 meters (over 26,000 ft ). Of the thousands of people who have attempted the summit, only about 2000 have been In 1981 a group of 20 physiologists, physicians, and successful, and more than 185 have died. -
Countries and Continents of the World: a Visual Model
Countries and Continents of the World http://geology.com/world/world-map-clickable.gif By STF Members at The Crossroads School Africa Second largest continent on earth (30,065,000 Sq. Km) Most countries of any other continent Home to The Sahara, the largest desert in the world and The Nile, the longest river in the world The Sahara: covers 4,619,260 km2 The Nile: 6695 kilometers long There are over 1000 languages spoken in Africa http://www.ecdc-cari.org/countries/Africa_Map.gif North America Third largest continent on earth (24,256,000 Sq. Km) Composed of 23 countries Most North Americans speak French, Spanish, and English Only continent that has every kind of climate http://www.freeusandworldmaps.com/html/WorldRegions/WorldRegions.html Asia Largest continent in size and population (44,579,000 Sq. Km) Contains 47 countries Contains the world’s largest country, Russia, and the most populous country, China The Great Wall of China is the only man made structure that can be seen from space Home to Mt. Everest (on the border of Tibet and Nepal), the highest point on earth Mt. Everest is 29,028 ft. (8,848 m) tall http://craigwsmall.wordpress.com/2008/11/10/asia/ Europe Second smallest continent in the world (9,938,000 Sq. Km) Home to the smallest country (Vatican City State) There are no deserts in Europe Contains mineral resources: coal, petroleum, natural gas, copper, lead, and tin http://www.knowledgerush.com/wiki_image/b/bf/Europe-large.png Oceania/Australia Smallest continent on earth (7,687,000 Sq. -

DEATH ZONE FREERIDE About the Project
DEATH ZONE FREERIDE About the project We are 3 of Snow Leopards, who commit the hardest anoxic high altitude ascents and perform freeride from the tops of the highest mountains on Earth (8000+). We do professional one of a kind filming on the utmost altitude. THE TRICKIEST MOUNTAINS ON EARTH NO BOTTLED OXYGEN CHALLENGES TO HUMAN AND NATURE NO EXTERIOR SUPPORT 8000ERS FREERIDE FROM THE TOPS MOVIES ALONE WITH NATURE FREERIDE DESCENTS 5 3 SNOW LEOS Why the project is so unique? PROFESSIONAL FILMING IN THE HARDEST CONDITIONS ❖ Higher than 8000+ m ❖ Under challenging efforts ❖ Without bottled oxygen & exterior support ❖ Severe weather conditions OUTDOOR PROJECT-OF-THE-YEAR “CRYSTAL PEAK 2017” AWARD “Death zone freeride” project got the “Crystal Peak 2017” award in “Outdoor project-of-the-year” nomination. It is comparable with “Oscar” award for Russian outdoor sphere. Team ANTON VITALY CARLALBERTO PUGOVKIN LAZO CIMENTI Snow Leopard. Snow Leopard. Leader The first Italian Snow Leopard. MC in mountaineering. Manaslu of “Mountain territory” club. Specializes in a ski mountaineering. freeride 8163m. High altitude Ski-mountaineer. Participant cameraman. of more than 20 high altitude expeditions. Mountains of the project Manaslu Annapurna Nanga–Parbat Everest K2 8163m 8091m 8125m 8848m 8611m The highest mountains on Earth ❖ 8027 m Shishapangma ❖ 8167 m Dhaulagiri I ❖ 8035 m Gasherbrum II (K4) ❖ 8201 m Cho Oyu ❖ 8051 m Broad Peak (K3) ❖ 8485 m Makalu ❖ 8080 m Gasherbrum I (Hidden Peak, K5) ❖ 8516 m Lhotse ❖ 8091 m Annapurna ❖ 8586 m Kangchenjunga ❖ 8126 m Nanga–Parbat ❖ 8614 m Chogo Ri (K2) ❖ 8156 m Manaslu ❖ 8848 m Chomolungma (Everest) Mountains that we climbed on MANASLU September 2017 The first and unique freeride descent from the altitude 8000+ meters among Russian sportsmen. -

Deadly High Altitude Pulmonary Disorders: Acute Mountain Sickness
Research Article Int J Pul & Res Sci Volume 1 Issue 1 - April 2016 Copyright © All rights are reserved by Michael Obrowski DOI : 10.19080/IJOPRS.2016.01.555553 Deadly High Altitude Pulmonary Disorders: Acute Mountain Sickness (AMS); High Altitude Pulmonary Edema (HAPE) and High Altitude Cerebral Edema (HACE): A Clinical Review Michael Obrowski1* and Stephanie Obrowski2 1Doctor of Medicine (M.D. – 2000); Assistant Professor of Anatomy; CEO, Chief Physician and Surgeon of Wilderness Physicians, European Union 2Doctor of Medicine (M.D. – 2019); Medical University of Łódź; President of Wilderness Physicians, European Union Submission: January 26, 2016; Published: April 15, 2016 *Corresponding author: Michael Obrowski, M.D., Doctor of Medicine (M.D. – 2000); Assistant Professor of Anatomy; CEO, Chief Physician and Surgeon of Wilderness Physicians, European Union, 43C Żeligowskiego Street, #45, Łódź, Poland 90-644, Email: Abstract Acute Mountain Sickness (AMS); High Altitude Pulmonary Edema (HAPE) and High Altitude Cerebral Edema (HACE). These three disorders, withMountain relatively Sickness, unimportant also smallcalled variationsHigh Altitude seen Sickness, in some isPulmonology specifically aTextbooks, triad of different because disorders, these are inso orderserious, of increasingthey are all seriousness: potentially deadly pulmonary disorders and we will discuss these three major, deadly disorders. Each one, starting with AMS, can progress rapidly to HAPE and then HACE. The two authors of this article have over half a century of high altitude mountaineering experience. They have also alsohad anddisaster still domedicine. have, for Since the lastspring twenty is rapidly years, approaching an NGO, Non-Profit and many Medical “weekend Organization backpackers” (Wilderness will start Physicians going into www.wildernessphysicians. -

Climb Mount Elbrus
climb Mount Elbrus actionchallenge on Mount Elbrus Our ascent of Mount Elbrus begins in the foothills of the lower Caucasus. Elbrus, an inactive volcano, is one of the famous Seven Summits and, at 5,642 m, is the highest mountain in Europe. It’s a fantastic, rewarding challenge - all you need is an adventurous team spirit, good fitness and two weeks out of the office. We begin our challenge from Kislovodsk, in the heart of the lower Caucasus. From here we carry out acclimatisation climbs, ascending progressively higher each day, practicing our crampon, rope and ice axe techniques. From Base Camp we climb through the rocky moraine of the Mikelchiran Glacier to our next camp at 3,600 m far above the grasslands, with stunning views across the glaciers and the lower Caucasus range. Together we make the climb to Lenz Rocks, crossing several crevasses, and prepare for our bid to reach the summit of Mount Elbrus. The ascent to the top is tough but exhilarating, beginning with a glacier climb to the saddle between the two summits at 5,416 m. We work as a team to climb up the next steep section to the ridge and, after a final short push, we reach the summit at 6,642 m. We are rewarded with a breathtaking view over the Caucasus from the highest point in Europe. Back in the spa town of Kislovodsk we celebrate our ascent to the summit of Mount Elbrus with a traditional Russian sauna, dinner and fine chilled vodka with our new friends. at a glance trip highlights ● Activity: Trekking - Altitude ● Take on one of the seven summits of the world ● Location: -

Conditioning: Why Go to the to Pack Light, Gym When You Just Pack Right Can Go Outdoors?
WWW.MOUNTAINEERS.ORG MARCH/APRIL 2011 • VOLUME 105 • NO. 2 MountaineerE X P L O R E • L E A R N • C O N S E R V E Conditioning: Why go to the To pack light, gym when you just pack right can go outdoors? Take your spring skiing to British Columbia’s backcountry inside Mar/Apr 2011 » Volume 105 » Number 2 9 How to best lighten your pack Enriching the community by helping people explore, conserve, learn about, and enjoy the 11 Sailing? Mountaineers? lands and waters of the Pacific Northwest. A carload of climbers said, why not? 18 B.C.’s best for spring skiing 11 Heading north? Check these lodges and huts 21 Train outdoors to get ready Why go to the gym when you can go to the beach? 24 Doing the PCT piece by piece This Foothills course is all about logistics 6 reaching OUT Mountaineers with sea legs Connecting the community to the outdoors 7 conservation currents 18 News about conservation and recreational access 14 OUR fRIENdS Goings on in the broader outdoor community 16 GEAR grist Making the turn from downhill to backcountry skiing 17 stepping UP Help prepare Kitsap Cabin for Earth Day! Best of British Columbia’s backcountry 26 bookMARkS Tasty trail food you don’t need to pack 24 27 PLAyGROUNd A place for kids to solve the puzzles of nature 28 CLIff notes New column looks at what’s up in the alpine 37 GO GUIdE Trips, outings, events, courses, seminars Taking on Washington’s Pacific Crest Trail DISCOVER THE MOUntaINEERS If you are thinking of joining — or have joined and aren’t sure where to The Mountaineer uses . -

Radiological Protection and Radioactive Waste Management
Occupational radiation doses of United Kingdom high altitude mountain guides as a result of cosmic ray exposures. Robert W Kerra* aRP Alba Ltd, Geanies House, Fearn, Tain, Ross-shire, Scotland, IV20 1TW, UK. Abstract UK based mountain guides lead multiple expeditions throughout the course of a year. They will receive radiation doses from cosmic rays during air travel and their time spent at elevated altitudes in the mountains of the world. These radiation doses are received as part of their employment. This paper illustrates that UK based high altitude mountain guides can potentially receive greater than 1 milliSv per year of cosmic radiation dose in excess of what they would have received at ground level. These individuals are “occupationally exposed” to cosmic radiation as a result of their profession. The European Community Basic Safety Standards Directive 96/29/EURATOM does not apply to exposure to cosmic radiation prevailing at ground level. The highest “ground level” that a UK mountain guide may be working at is 8848m. The maximum flying altitude of some internal flights in the UK is 7925m. 96/29/EURATOM does apply to cosmic radiations being received by aircrews therefore there is an anomaly in radiation protection where the cosmic radiation exposures of aircrew operating for short durations at altitudes lower than mountain guides operating at high altitudes for prolonged times have to be taken into account. UK based high altitude mountain guides are undergoing planned occupational exposures to cosmic radiation whilst still on the ground. Consideration should be given by the legislative authorities to include the control and assessment of cosmic radiation exposures of professionals likely to receive greater than 1 milliSv per year of cosmic radiation in excess of what would have been received in their home country at ground level. -

Book Reviews 1988 COMPILED by GEOFFREY TEMPLEMAN
Book Reviews 1988 COMPILED BY GEOFFREY TEMPLEMAN Touching the Void Joe Simpson ]onathan Cape, 1988, Pp174, £10·95 In 1985 Joe Simpson and Simon Yates set out to climb the W face of Siula Grande in the Peruvian Andes. They succeeded in their objective after three days and started on the descent of the N ridge in atrocious snow conditions. After a night on the ridge they continued their slow progress, breaking through cornices and having short falls, until one such fall resulted in Simpson breaking his leg. Yates started lowering Simpson down the W face, and they had almost reached the bottom when Simpson shot off over an overhanging cliff and was left hanging. After a considerable length of time in which nothing could be done, Yates cut the rope. Giving Simpson up for dead, he made his way back to Base Camp and, during the next three days, sorted out Simpson's belongings, burnt his clothes and prepared to leave camp. It was then that Simpson arrived in a state of exhausted delirium, having escaped from the deep crevasse into which he had fallen and crawled and hopped over the long glacier and moraine. The book recounts the story in a graphic and frank way. The psycho logical trauma following the decision to cut the rope; the thoughts engendered by being trapped in a deep crevasse with a broken leg; the embarrassment of the eventual meeting: these things are written about in depth and with a clarity that is only too well understood. You know Simpson will survive, but the tale is like a thriller - I almost said, a cliff-hanger - progressing from one dramatic situation to the next. -

Outcomes from the 2015 Round Table on Sepsis
The official daily newsletter of the 35th ISICEM Thursday 19 March 2015 Day 3 Outcomes from the 2015 Round Table on sepsis uring the opening session on Tues- day morning, Simon Finfer (Royal North Shore Hospital of Sydney and Sydney Adventist Hospital, Sydney, Australia) was joined by Steven DOpal (Memorial Hospital of Rhode Island, RI, USA) to summarize the major outcomes of the two-day Round Table discussion “This will be a on sepsis. This was a joint conference significant part of our conducted between ISICEM and the Inter- national Sepsis Forum, with representa- research agenda in the tives from every continent highlighting the future – making sure global nature of the problem. Beginning by addressing the current that our patients are state of knowledge in the epidemiology of doing well after they sepsis, Professor Finfer noted that we know leave the hospital.” surprising little, but that obtaining this data will be crucial if any meaningful strategy is Steven Opal to be developed: “To some degree we have data from developed countries, possibly far less than you would expect or think,” he said. “But there are certainly places in, notably, Africa, where we are completely devoid of data.” The reasons for this lack of data can in part be understood by an appreciation of how patient data are currently characterized and treated, with the Global Burden of Disease Project emerging as a central player in generating evidence and guiding is surprising because we believe that sepsis kills one comes into your ICU with community-acquired global health policy. more people than prostate cancer, breast cancer, pneumonia, you treat the pneumonia; maybe they “The only reference to sepsis in these sta- and many other high profile diseases. -

Mount Everest's Death Zone
Mount Everest’s Death Zone Climate change and crowds of climbers are making the world’s tallest mountain more dangerous than ever Mara Grunbaum ast year, 73-year-old Tamae Watanabe of Japan became the oldest woman to climb Mount Everest, the world’s tallest mountain. In L 2010, 13-year-old Jordan Romero of California became the youngest to reach the top. All sorts of people of varying abilities scale the massive mountain in Asia these days. That may not be a good thing—for Everest or the climbers. Last year, more than 500 people reached the top of the Himalayan mountain, which towers 8,850 meters (29,035 feet) above sea level. Hundreds more climbed partway up. While it’s a great achievement to scale Everest, it can sometimes cause problems for the climbers and the mountain itself. Everest is changing. Warming Up Why is Everest becoming more dangerous to climb? One reason is changes in its environment. Much of the mountain is covered in huge sheets of ice called glaciers. Lately, warmer temperatures in the region have been melting these glaciers. Some places that used to be covered in ice year-round are now completely ice-free in the summer. Shrinking glaciers put climbers at risk. As glaciers melt, snow, ice, and rock are more likely to tumble down the mountain in huge avalanches. These snowslides can injure or even kill climbers. “As it gets warmer, more debris tends to fall down,” says American climbing guide Freddie Wilkinson. He’s one of a number of people who think that climbing Everest is becoming too risky. -

Seven Summits. Four Months. One Dream
ADVENTURE SEVEN SUMMITS. FOUR MONTHS. ONE DREAM. n December 2014, after being dumped by a wave SpinalCure Australia and Surf Life Saving WA. and driven head first into the sand at Cottesloe And so, his Project 7in4 was born. Beach in Perth, Western Australia, local Steve “Lying in a hospital bed with an uncertain prognosis Plain laid partially paralysed, face-down in the after my accident was frustrating and frightening — water. Unable to breathe, his initial concern I had never felt so weak or hopeless,” explains Steve. Iwas drowning. Fortunately, Steve’s life was saved by “I made the decision not to accept the doctor’s diagnosis, the quick work of volunteer surf lifesavers Lara and and managed to overcome significant spinal injury to STEVE’S The Gary Matier and friend Dave Field. He was rushed to walk again, but others are not as lucky. My goal is to hospital under full spinal precautions and eventually raise awareness and funds for the organisations ASCENSIONS Incredible told he had sustained multiple unstable fractures at providing vital assistance to these people. SpinalCure the C2, C3 and C7 vertebrae as well as a contorted Australia is funding some world-first neuroscience Journey of a spinal cord, ruptured disc, dissected arterial artery, research using neurostimulation to give life-changing MT VINSON ANTARCTICA torn ligaments and more. benefits to people currently living with spinal cord summited True Aussie The prognosis was initially very poor as Steve was injuries. Through Project 7in4, I hope to drive enough January 16, 2018 told by doctor’s he may never regain full movement. -
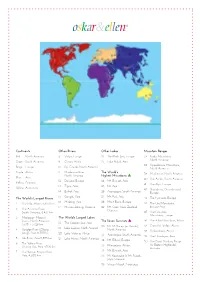
Other Rivers
Continents Other Rivers Other Lakes Mountain Ranges Red North America 8 Volga, Europe 22 The Black Sea, Europe 37 Rocky Mountains, North America Green South America 9 Congo, Africa 23 Lake Bajkal, Asia 38 Appalachian Mountains, Beige Europe 10 Rio Grande, North America North America Purple Africa 11 Mackenzie River, The World’s 39 Mackenzie, North America North America Highest Mountains s Blue Asia 40 The Andes, South America 12 Danube, Europe 24 Mt. Everest, Asia Yellow Oceania 41 The Alps, Europe 13 Tigris, Asia 25 K2, Asia White Antarctica 42 Skanderna, (Scandinavia) 14 Eufrat, Asia 26 Aconcagua, South America Europe 15 Ganges, Asia 27 Mt. Fuji, Asia The World’s Longest Rivers 43 The Pyrenees, Europe 16 Mekong, Asia 28 Mont Blanc, Europe 1 The Nile, Africa, 6,650 km 44 The Ural Mountains, 17 Murray-Darling, Oceania 29 Mt. Cook, New Zealand, Europe-Asia 2 The Amazon River, Oceania South America, 6,437 km 45 The Caucasus Mountains, Europe 3 Mississippi- Missouri The World’s Largest Lakes Rivers, North America, The Seven Summits s 46 The Atlas Mountains, Africa 3,778 + 3,726 km 18 The Caspian Sea, Asia 30 Mt. McKinley (or Denali), 47 Great Rift Valley, Africa 19 Lake Superior, North America 4 Yangtze River (Chang North America 48 Drakensberg, Africa Jiang), Asia, 6,300 km 20 Lake Victoria, Africa 31 Aconcagua, South America 49 The Himalayas, Asia 5 Ob River, Asia 5,570 km 21 Lake Huron, North America 32 Mt. Elbrus, Europe 50 The Great Dividing Range 6 The Yellow River 33 Kilimanjaro, Africa (or Eastern Highlands), (Huang Ho), Asia, 4,700 km Australia 7 The Yenisei-Angara River, 34 Mt.