Female Reproductive System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ovarian Cancer and Cervical Cancer
What Every Woman Should Know About Gynecologic Cancer R. Kevin Reynolds, MD The George W. Morley Professor & Chief, Division of Gyn Oncology University of Michigan Ann Arbor, MI What is gynecologic cancer? Cancer is a disease where cells grow and spread without control. Gynecologic cancers begin in the female reproductive organs. The most common gynecologic cancers are endometrial cancer, ovarian cancer and cervical cancer. Less common gynecologic cancers involve vulva, Fallopian tube, uterine wall (sarcoma), vagina, and placenta (pregnancy tissue: molar pregnancy). Ovary Uterus Endometrium Cervix Vagina Vulva What causes endometrial cancer? Endometrial cancer is the most common gynecologic cancer: one out of every 40 women will develop endometrial cancer. It is caused by too much estrogen, a hormone normally present in women. The most common cause of the excess estrogen is being overweight: fat cells actually produce estrogen. Another cause of excess estrogen is medication such as tamoxifen (often prescribed for breast cancer treatment) or some forms of prescribed estrogen hormone therapy (unopposed estrogen). How is endometrial cancer detected? Almost all endometrial cancer is detected when a woman notices vaginal bleeding after her menopause or irregular bleeding before her menopause. If bleeding occurs, a woman should contact her doctor so that appropriate testing can be performed. This usually includes an endometrial biopsy, a brief, slightly crampy test, performed in the office. Fortunately, most endometrial cancers are detected before spread to other parts of the body occurs Is endometrial cancer treatable? Yes! Most women with endometrial cancer will undergo surgery including hysterectomy (removal of the uterus) in addition to removal of ovaries and lymph nodes. -

Sexual Reproduction & the Reproductive System Visual
Biology 202: Sexual Reproduction & the Reproductive System 1) Label the diagram below. Some terms may be used more than once. Spermatozoa (N) Mitosis Spermatogonium (2N) Spermatids (N) Primary Oocyte (2N) Polar bodies (N) Ootid (N) Second polar body (N) Meiosis I Primary spermatocyte (2N) Oogonium (2N) Secondary oocyte (2N) Ovum (N) Secondary spermatocytes (2N) First polar body Meiosis II Source Lesson: Gametogenesis & Meiosis: Process & Differences 2) Label the diagram of the male reproductive system below. Seminal vesicle Testis Scrotum Pubic bone Penis Prostate gland Urethra Epididymis Vas deferens Bladder Source Lesson: Male Reproductive System: Structures, Functions & Regulation 3) Label the image below. Rectum Testis Ureter Bulbourethral gland Urethra Urinary bladder Pubic bone Penis Seminal vesicle Ductus deferens Epididymis Prostate gland Anus Source Lesson: Semen: Composition & Production 4) Label the structures below. Inner and outer lips of the vagina Mons pubis Vaginal opening Clitoris Anus Urethral opening Perineum Vulva Source Lesson: Female Reproductive System: Structures & Functions 5) Label the diagram below. Some terms may be used more than once. Clitoris Vulva Labia majora Labia minora Perineum Clitoral hood Vaginal opening Source Lesson: Female Reproductive System: Structures & Functions 6) Label the internal organs that make up the female reproductive system. Uterus Fallopian tubes Ovaries Cervix Vagina Endometrium Source Lesson: Female Reproductive System: Structures & Functions 7) Label the diagram below. LH Follicular -

Chapter 28 *Lecture Powepoint
Chapter 28 *Lecture PowePoint The Female Reproductive System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • The female reproductive system is more complex than the male system because it serves more purposes – Produces and delivers gametes – Provides nutrition and safe harbor for fetal development – Gives birth – Nourishes infant • Female system is more cyclic, and the hormones are secreted in a more complex sequence than the relatively steady secretion in the male 28-2 Sexual Differentiation • The two sexes indistinguishable for first 8 to 10 weeks of development • Female reproductive tract develops from the paramesonephric ducts – Not because of the positive action of any hormone – Because of the absence of testosterone and müllerian-inhibiting factor (MIF) 28-3 Reproductive Anatomy • Expected Learning Outcomes – Describe the structure of the ovary – Trace the female reproductive tract and describe the gross anatomy and histology of each organ – Identify the ligaments that support the female reproductive organs – Describe the blood supply to the female reproductive tract – Identify the external genitalia of the female – Describe the structure of the nonlactating breast 28-4 Sexual Differentiation • Without testosterone: – Causes mesonephric ducts to degenerate – Genital tubercle becomes the glans clitoris – Urogenital folds become the labia minora – Labioscrotal folds -

A Case of Non-Communicating Uterine Horn Containing Functional Endometrium
logy & Ob o st ec e tr n i y c s G Rani et al., Gynecol Obstet (Sunnyvale) 2015, 5:9 Gynecology & Obstetrics DOI: 10.4172/2161-0932.1000320 ISSN: 2161-0932 Case Report Open Access A Case of Non-Communicating Uterine Horn Containing Functional Endometrium Anjali Rani*, Madhu Kumari and Shipra Department of Obstetrics and Gynaecology, Institute Of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India Abstract Uterine anoamalies are very rare. They can present with complains of amebnorrhoea, dysmenorrhoea, bad obstetrical outcome and infertility etc. Unicornuate uterus with rudimentary horn is very rare. The incidence of this is 1/100,000. Normally rudimentary horns are non- functional and non-communicating. But if they have functional endometrium they can develop hematometra. We are presenting a case of hematometra and pain in a patient with rudimentary non communicating horn with functional endometrium. Rudimentary horn should be kept as a differential diagnosis in pelvic pain. Keywords: Unicornuate uterus; Rudimentary horn; Dysmenorrhea were found in the pelvis. Exploratory laparotomy was decided and the rudimentary horn was excised by applying clamps (Figure 2). Histo- Introduction pathological examination of the specimen was reported as uterine Uterine anomalies are very rarely seen. Unicornuate uterus is a very udimentary horn with functional endometrium with haematometra. rare uterine anomaly. The incidence of congenital uterine anomalies The patient was discharged on the fifth postoperative day. She came in in fertile population is 1/200 to 1/600. The incidence of rudimentary follow up her nomal menses after 6 weeks. horn is very very rare (1:100,000). -

The Cyclist's Vulva
The Cyclist’s Vulva Dr. Chimsom T. Oleka, MD FACOG Board Certified OBGYN Fellowship Trained Pediatric and Adolescent Gynecologist National Medical Network –USOPC Houston, TX DEPARTMENT NAME DISCLOSURES None [email protected] DEPARTMENT NAME PRONOUNS The use of “female” and “woman” in this talk, as well as in the highlighted studies refer to cis gender females with vulvas DEPARTMENT NAME GOALS To highlight an issue To discuss why this issue matters To inspire future research and exploration To normalize the conversation DEPARTMENT NAME The consensus is that when you first start cycling on your good‐as‐new, unbruised foof, it is going to hurt. After a “breaking‐in” period, the pain‐to‐numbness ratio becomes favourable. As long as you protect against infection, wear padded shorts with a generous layer of chamois cream, no underwear and make regular offerings to the ingrown hair goddess, things are manageable. This is wrong. Hannah Dines British T2 trike rider who competed at the 2016 Summer Paralympics DEPARTMENT NAME MY INTRODUCTION TO CYCLING Childhood Adolescence Adult Life DEPARTMENT NAME THE CYCLIST’S VULVA The Issue Vulva Anatomy Vulva Trauma Prevention DEPARTMENT NAME CYCLING HAS POSITIVE BENEFITS Popular Means of Exercise Has gained popularity among Ideal nonimpact women in the past aerobic exercise decade Increases Lowers all cause cardiorespiratory mortality risks fitness DEPARTMENT NAME Hermans TJN, Wijn RPWF, Winkens B, et al. Urogenital and Sexual complaints in female club cyclists‐a cross‐sectional study. J Sex Med 2016 CYCLING ALSO PREDISPOSES TO VULVAR TRAUMA • Significant decreases in pudendal nerve sensory function in women cyclists • Similar to men, women cyclists suffer from compression injuries that compromise normal function of the main neurovascular bundle of the vulva • Buller et al. -

Pregnancy and Cesarean Delivery After Multimodal Therapy for Vulvar Carcinoma: a Case Report
MOLECULAR AND CLINICAL ONCOLOGY 5: 583-586, 2016 Pregnancy and cesarean delivery after multimodal therapy for vulvar carcinoma: A case report KUNIAKI TORIYABE1,2, HARUKI TANIGUCHI2, TOKIHIRO SENDA2,3, MASAKO NAKANO2, YOSHINARI KOBAYASHI2, MIHO IZAWA2, HIROHIKO TANAKA2, TETSUO ASAKURA2, TSUTOMU TABATA1 and TOMOAKI IKEDA1 1Department of Obstetrics and Gynecology, Mie University Graduate School of Medicine, Tsu, Mie 514-8507; 2Department of Obstetrics and Gynecology, Mie Prefectural General Medical Center, Yokkaichi, Mie 510-8561; 3Department of Obstetrics and Gynecology, Kinan Hospital, Mihama, Mie 519-5293, Japan Received November 4, 2015; Accepted September 12, 2016 DOI: 10.3892/mco.2016.1021 Abstract. Reports of pregnancy following treatment for vulvectomy, may have an increased incidence of caesarean vulvar carcinoma are extremely uncommon, as the main delivery (2). In the literature, vulvar scarring following radical problem of subsequent pregnancy is vulvar scarring following vulvectomy was the major reason for pregnant women under- radical surgery. We herein report the case of a patient who was going caesarean section (2-7). To date, no cases of pregnancy diagnosed with stage I squamous cell carcinoma of the vulva following vulvar carcinoma have been reported in patients at the age of 17 years and was treated with multimodal therapy, who had undergone surgery and radiotherapy. including neoadjuvant chemotherapy, wide local excision with We herein describe a case in which caesarean section was bilateral inguinal lymph node dissection and adjuvant radio- performed due to the presence of extensive vulvar scarring therapy. The patient became pregnant spontaneously 9 years following multimodal therapy for vulvar carcinoma, including after her initial diagnosis and the antenatal course was good, chemotherapy, surgery and radiotherapy. -
Womens Health Requisition Forms
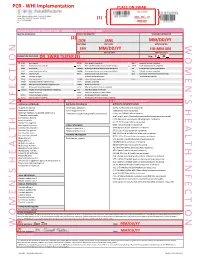
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Female Perineum Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Female Perineum Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the student should be able to describe the: ✓ Boundaries of the perineum. ✓ Division of perineum into two triangles. ✓ Boundaries & Contents of anal & urogenital triangles. ✓ Lower part of Anal canal. ✓ Boundaries & contents of Ischiorectal fossa. ✓ Innervation, Blood supply and lymphatic drainage of perineum. Lecture Outline ‰ Introduction: • The trunk is divided into 4 main cavities: thoracic, abdominal, pelvic, and perineal. (see image 1) • The pelvis has an inlet and an outlet. (see image 2) The lowest part of the pelvic outlet is the perineum. • The perineum is separated from the pelvic cavity superiorly by the pelvic floor. • The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue. (see image 3) We will talk about them more in the next lecture. Image (1) Image (2) Image (3) Note: this image is seen from ABOVE Perineum (In this lecture the boundaries and relations are important) o Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) o It is a diamond shaped area between the thighs. Boundaries: (these are the external or surface boundaries) Anteriorly Laterally Posteriorly Medial surfaces of Intergluteal folds Mons pubis the thighs or cleft Contents: 1. Lower ends of urethra, vagina & anal canal 2. External genitalia 3. Perineal body & Anococcygeal body Extra (we will now talk about these in the next slides) Perineum Extra explanation: The perineal body is an irregular Perineal body fibromuscular mass. -

Sexual Assault
Sexual Assault Victimization Across the Life Span A Color Atlas Barbara W. Girardin, RN, PhD Forensic Health Care Palomar Pomerado Health Escondido, California Diana K. Faugno, RN, BSN, CPN, FAAFS, SANE-A District Director Pediatrics/Nicu Forensic Health Service Palomar Pomerado Health Escondido, California Mary J. Spencer, MD Clinical Professor of Pediatrics University of California San Diego School of Medicine Medical Director Child Abuse Prevention and Sexual Assault Response Team Palomar Pomerado Health Escondido, California Angelo P. Giardino, MD, PhD Associate Chair - Pediatrics Associate Physician-in-Chief St. Christopher's Hospital for Children Associate Professor in Pediatrics Drexel University College of Medicine Philadelphia, Pennsylvania G.W. Medical Publishing, Inc. St. Louis FOREWORD Whether in the pediatric emergency room, the adult sexual assault clinic, the nursing home or even the morgue, high quality photography of visible lesions remains an essential documentation and investigation tool. The value of photographic documentation cannot be overstated. Indeed, all medical providers who evaluate sexual assault victims should be familiar with the basic principles and techniques of clinical photography and should assure adequate photographic documentation of visible lesions. Such images, whether still or video, may be used in court, although less commonly than photographs of physical abuse (sometimes judges and juries have a hard time understanding the significance of, for example, a subtle hymenal tear). Photographs are also important for peer review, peer consultation and teaching. Perhaps most significantly, photographs may allow a second opinion by opposing council experts without subjecting the victim to a repeat examination. The evolution in photodocumentation techniques in sexual assault has often followed, sometimes paralleled, and even sometimes led the evolution in the medical examination and interpretation of sexual assault injuries. -

The Reproductive System
27 The Reproductive System PowerPoint® Lecture Presentations prepared by Steven Bassett Southeast Community College Lincoln, Nebraska © 2012 Pearson Education, Inc. Introduction • The reproductive system is designed to perpetuate the species • The male produces gametes called sperm cells • The female produces gametes called ova • The joining of a sperm cell and an ovum is fertilization • Fertilization results in the formation of a zygote © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • Overview of the Male Reproductive System • Testis • Epididymis • Ductus deferens • Ejaculatory duct • Spongy urethra (penile urethra) • Seminal gland • Prostate gland • Bulbo-urethral gland © 2012 Pearson Education, Inc. Figure 27.1 The Male Reproductive System, Part I Pubic symphysis Ureter Urinary bladder Prostatic urethra Seminal gland Membranous urethra Rectum Corpus cavernosum Prostate gland Corpus spongiosum Spongy urethra Ejaculatory duct Ductus deferens Penis Bulbo-urethral gland Epididymis Anus Testis External urethral orifice Scrotum Sigmoid colon (cut) Rectum Internal urethral orifice Rectus abdominis Prostatic urethra Urinary bladder Prostate gland Pubic symphysis Bristle within ejaculatory duct Membranous urethra Penis Spongy urethra Spongy urethra within corpus spongiosum Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Scrotum Testis © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • The Testes • Testes hang inside a pouch called the scrotum, which is on the outside of the body -

MR Imaging of Vaginal Morphology, Paravaginal Attachments and Ligaments
MR imaging of vaginal morph:ingynious 05/06/15 10:09 Pagina 53 Original article MR imaging of vaginal morphology, paravaginal attachments and ligaments. Normal features VITTORIO PILONI Iniziativa Medica, Diagnostic Imaging Centre, Monselice (Padova), Italy Abstract: Aim: To define the MR appearance of the intact vaginal and paravaginal anatomy. Method: the pelvic MR examinations achieved with external coil of 25 nulliparous women (group A), mean age 31.3 range 28-35 years without pelvic floor dysfunctions, were compared with those of 8 women who had cesarean delivery (group B), mean age 34.1 range 31-40 years, for evidence of (a) vaginal morphology, length and axis inclination; (b) perineal body’s position with respect to the hymen plane; and (c) visibility of paravaginal attachments and lig- aments. Results: in both groups, axial MR images showed that the upper vagina had an horizontal, linear shape in over 91%; the middle vagi- na an H-shape or W-shape in 74% and 26%, respectively; and the lower vagina a U-shape in 82% of cases. Vaginal length, axis inclination and distance of perineal body to the hymen were not significantly different between the two groups (mean ± SD 77.3 ± 3.2 mm vs 74.3 ± 5.2 mm; 70.1 ± 4.8 degrees vs 74.04 ± 1.6 degrees; and +3.2 ± 2.4 mm vs + 2.4 ± 1.8 mm, in group A and B, respectively, P > 0.05). Overall, the lower third vaginal morphology was the less easily identifiable structure (visibility score, 2); the uterosacral ligaments and the parau- rethral ligaments were the most frequently depicted attachments (visibility score, 3 and 4, respectively); the distance of the perineal body to the hymen was the most consistent reference landmark (mean +3 mm, range -2 to + 5 mm, visibility score 4). -

The Mythical G-Spot: Past, Present and Future by Dr
Global Journal of Medical research: E Gynecology and Obstetrics Volume 14 Issue 2 Version 1.0 Year 2014 Type: Double Blind Peer Reviewed International Research Journal Publisher: Global Journals Inc. (USA) Online ISSN: 2249-4618 & Print ISSN: 0975-5888 The Mythical G-Spot: Past, Present and Future By Dr. Franklin J. Espitia De La Hoz & Dra. Lilian Orozco Santiago Universidad Militar Nueva Granada, Colombia Summary- The so-called point Gräfenberg popularly known as "G-spot" corresponds to a vaginal area 1-2 cm wide, behind the pubis in intimate relationship with the anterior vaginal wall and around the urethra (complex clitoral) that when the woman is aroused becomes more sensitive than the rest of the vagina. Some women report that it is an erogenous area which, once stimulated, can lead to strong sexual arousal, intense orgasms and female ejaculation. Although the G-spot has been studied since the 40s, disagreement persists regarding the translation, localization and its existence as a distinct structure. Objective: Understand the operation and establish the anatomical points where the point G from embryology to adulthood. Methodology: A literature search in the electronic databases PubMed, Ovid, Elsevier, Interscience, EBSCO, Scopus, SciELO was performed. Results: descriptive articles and observational studies were reviewed which showed a significant number of patients. Conclusion: Sexual pleasure is a right we all have, and women must find a way to feel or experience orgasm as a possible experience of their sexuality, which necessitates effective stimulation. Keywords: G Spot; vaginal anatomy; clitoris; skene’s glands. GJMR-E Classification : NLMC Code: WP 250 TheMythicalG-SpotPastPresentandFuture Strictly as per the compliance and regulations of: © 2014.