Holiday Plants with Toxic Misconceptions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix Color Plates of Solanales Species
Appendix Color Plates of Solanales Species The first half of the color plates (Plates 1–8) shows a selection of phytochemically prominent solanaceous species, the second half (Plates 9–16) a selection of convol- vulaceous counterparts. The scientific name of the species in bold (for authorities see text and tables) may be followed (in brackets) by a frequently used though invalid synonym and/or a common name if existent. The next information refers to the habitus, origin/natural distribution, and – if applicable – cultivation. If more than one photograph is shown for a certain species there will be explanations for each of them. Finally, section numbers of the phytochemical Chapters 3–8 are given, where the respective species are discussed. The individually combined occurrence of sec- ondary metabolites from different structural classes characterizes every species. However, it has to be remembered that a small number of citations does not neces- sarily indicate a poorer secondary metabolism in a respective species compared with others; this may just be due to less studies being carried out. Solanaceae Plate 1a Anthocercis littorea (yellow tailflower): erect or rarely sprawling shrub (to 3 m); W- and SW-Australia; Sects. 3.1 / 3.4 Plate 1b, c Atropa belladonna (deadly nightshade): erect herbaceous perennial plant (to 1.5 m); Europe to central Asia (naturalized: N-USA; cultivated as a medicinal plant); b fruiting twig; c flowers, unripe (green) and ripe (black) berries; Sects. 3.1 / 3.3.2 / 3.4 / 3.5 / 6.5.2 / 7.5.1 / 7.7.2 / 7.7.4.3 Plate 1d Brugmansia versicolor (angel’s trumpet): shrub or small tree (to 5 m); tropical parts of Ecuador west of the Andes (cultivated as an ornamental in tropical and subtropical regions); Sect. -

Solanum Pseudocapsicum
Solanum pseudocapsicum COMMON NAME Jerusalem cherry FAMILY Solanaceae AUTHORITY Solanum pseudocapsicum L. FLORA CATEGORY Vascular – Exotic STRUCTURAL CLASS Trees & Shrubs - Dicotyledons NVS CODE SOLPSE HABITAT Bartons Bush, Trentham. Apr 2006. Terrestrial. Photographer: Jeremy Rolfe FEATURES Erect, unarmed shrub, glabrous or sometimes with few branched hairs on very young shoots; stems wiry, 40~120cm tall. Petiole to 2cm long, slender. Lamina 3~12 x 1~3cm, lanceolate or elliptic-lanceolate, glossy above; margins usu. undulate; base narrowly attenuate; apex obtuse or acute. Flowers 1~several; peduncle 0~8mm long; pedicels 5~10mm long, erect at fruiting. Calyx 4~5mm long; lobes lanceolate to ovate, slightly accrescent. Corolla approx. 15mm diam., white, glabrous; lobes oblong- ovate to triangular. Anthers 2.5~3mm long. Berry 1.5~2cm diam., globose, glossy, orange to scarlet, long-persistent; stone cells 0. Seeds approx. Bartons Bush, Trentham. Apr 2006. 3mm diam., suborbicular to reniform or obovoid, rather asymmetric; Photographer: Jeremy Rolfe margin thickened. (-Webb et. al., 1988) SIMILAR TAXA A plant with attractive glossy orange or red berries around 1-2 cm diameter (Department of Conservation 1996). FLOWERING October, November, December, January, February, March, April, May FLOWER COLOURS White, Yellow YEAR NATURALISED 1935 ORIGIN Eastern Sth America ETYMOLOGY solanum: Derivation uncertain - possibly from the Latin word sol, meaning “sun,” referring to its status as a plant of the sun. Another possibility is that the root was solare, meaning “to soothe,” or solamen, meaning “a comfort,” which would refer to the soothing effects of the plant upon ingestion. Reason For Introduction Ornamental Life Cycle Comments Perennial. Dispersal Seed is bird dispersed (Webb et al., 1988; Department of Conservation 1996). -
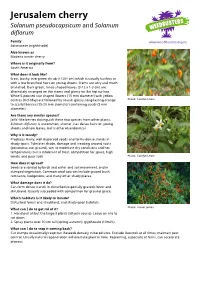
Jerusalem Cherry Solanum Pseudocapsicum and Solanum Diflorum
Jerusalem cherry Solanum pseudocapsicum and Solanum diflorum Family Solanaceae (nightshade) Also known as Madeira winter cherry Where is it originally from? South America What does it look like? Erect, bushy, evergreen shrub (<120+ cm) which is usually hairless or with a few branched hairs on young shoots. Stems are wiry and much branched. Dark green, lance-shaped leaves (3-12 x 1-3 cm) are alternately arranged on the stems and glossy on the top surface. White 5-pointed star shaped flowers (15 mm diameter) with yellow centres (Oct-May) are followed by round, glossy, long-lasting orange Photo: Carolyn Lewis to scarlet berries (15-20 mm diameter) containing seeds (3 mm diameter). Are there any similar species? Jaffa'-like berries distinguish these two species from other plants. Solanum diflorum is uncommon, shorter, has dense hairs on young shoots and new leaves, but is otherwise identical. Why is it weedy? Produces many, well dispersed seeds and forms dense stands in shady spots. Tolerates shade, damage and treading around roots (poisonous, not grazed), wet to moderate dry conditions and hot temperatures but is intolerant of frost, competition for space, high winds, and poor soils. Photo: Carolyn Lewis How does it spread? Seeds are spread by birds and water and soil movement, and in dumped vegetation. Common seed sources include grazed bush remnants, hedgerows, and many other shady places. What damage does it do? Can form dense stands in disturbed (especially grazed) forest and shrubland. Usually succeeded with competition for ground space. Which habitats is it likely to invade? Disturbed forest and shrubland, and shady open habitats. -

A Molecular Phylogeny of the Solanaceae
TAXON 57 (4) • November 2008: 1159–1181 Olmstead & al. • Molecular phylogeny of Solanaceae MOLECULAR PHYLOGENETICS A molecular phylogeny of the Solanaceae Richard G. Olmstead1*, Lynn Bohs2, Hala Abdel Migid1,3, Eugenio Santiago-Valentin1,4, Vicente F. Garcia1,5 & Sarah M. Collier1,6 1 Department of Biology, University of Washington, Seattle, Washington 98195, U.S.A. *olmstead@ u.washington.edu (author for correspondence) 2 Department of Biology, University of Utah, Salt Lake City, Utah 84112, U.S.A. 3 Present address: Botany Department, Faculty of Science, Mansoura University, Mansoura, Egypt 4 Present address: Jardin Botanico de Puerto Rico, Universidad de Puerto Rico, Apartado Postal 364984, San Juan 00936, Puerto Rico 5 Present address: Department of Integrative Biology, 3060 Valley Life Sciences Building, University of California, Berkeley, California 94720, U.S.A. 6 Present address: Department of Plant Breeding and Genetics, Cornell University, Ithaca, New York 14853, U.S.A. A phylogeny of Solanaceae is presented based on the chloroplast DNA regions ndhF and trnLF. With 89 genera and 190 species included, this represents a nearly comprehensive genus-level sampling and provides a framework phylogeny for the entire family that helps integrate many previously-published phylogenetic studies within So- lanaceae. The four genera comprising the family Goetzeaceae and the monotypic families Duckeodendraceae, Nolanaceae, and Sclerophylaceae, often recognized in traditional classifications, are shown to be included in Solanaceae. The current results corroborate previous studies that identify a monophyletic subfamily Solanoideae and the more inclusive “x = 12” clade, which includes Nicotiana and the Australian tribe Anthocercideae. These results also provide greater resolution among lineages within Solanoideae, confirming Jaltomata as sister to Solanum and identifying a clade comprised primarily of tribes Capsiceae (Capsicum and Lycianthes) and Physaleae. -

Evolutionary Routes to Biochemical Innovation Revealed by Integrative
RESEARCH ARTICLE Evolutionary routes to biochemical innovation revealed by integrative analysis of a plant-defense related specialized metabolic pathway Gaurav D Moghe1†, Bryan J Leong1,2, Steven M Hurney1,3, A Daniel Jones1,3, Robert L Last1,2* 1Department of Biochemistry and Molecular Biology, Michigan State University, East Lansing, United States; 2Department of Plant Biology, Michigan State University, East Lansing, United States; 3Department of Chemistry, Michigan State University, East Lansing, United States Abstract The diversity of life on Earth is a result of continual innovations in molecular networks influencing morphology and physiology. Plant specialized metabolism produces hundreds of thousands of compounds, offering striking examples of these innovations. To understand how this novelty is generated, we investigated the evolution of the Solanaceae family-specific, trichome- localized acylsugar biosynthetic pathway using a combination of mass spectrometry, RNA-seq, enzyme assays, RNAi and phylogenomics in different non-model species. Our results reveal hundreds of acylsugars produced across the Solanaceae family and even within a single plant, built on simple sugar cores. The relatively short biosynthetic pathway experienced repeated cycles of *For correspondence: [email protected] innovation over the last 100 million years that include gene duplication and divergence, gene loss, evolution of substrate preference and promiscuity. This study provides mechanistic insights into the † Present address: Section of emergence of plant chemical novelty, and offers a template for investigating the ~300,000 non- Plant Biology, School of model plant species that remain underexplored. Integrative Plant Sciences, DOI: https://doi.org/10.7554/eLife.28468.001 Cornell University, Ithaca, United States Competing interests: The authors declare that no Introduction competing interests exist. -

Harmful Garden Plants in Western Australia
Research Library Bulletins 4000 - Research Publications 4-2005 Harmful garden plants in Western Australia Department of Agriculture and Food, Western Australia Follow this and additional works at: https://researchlibrary.agric.wa.gov.au/bulletins Part of the Botany Commons, and the Pharmacology, Toxicology and Environmental Health Commons Recommended Citation Department of Agriculture and Food, Western Australia. (2005), Harmful garden plants in Western Australia. Department of Primary Industries and Regional Development, Western Australia, Perth. Bulletin 4641. This bulletin is brought to you for free and open access by the Research Publications at Research Library. It has been accepted for inclusion in Bulletins 4000 - by an authorized administrator of Research Library. For more information, please contact [email protected]. Bulletin No. 4641 ISSN 1448-0352 April 2005 Harmful garden plants inWestern Australia JJ1631-DeptOfAg-20pp-FA.indd1631-DeptOfAg-20pp-FA.indd I 222/04/20052/04/2005 112:04:552:04:55 PPMM Disclaimer 1. The information, representations and statements contained in this publication (“Information”) are provided for general information purposes only. 2. The State of Western Australia, the Minister for Agriculture, the Chief Executive Officer of Agriculture and their respective officers, employees and agents: (a) do not make any representation or warranty as to the accuracy, reliability, completeness or currency of the Information; and (b) shall not be liable, in negligence or otherwise, to any person for any loss, liability, damage, personal injury or death arising out of any act or failure to act by any person in using or relying on the Information. 3. Any person who uses the Information does so at his or her own risk. -

SOLANACEAE 茄科 Qie Ke Zhang Zhi-Yun, Lu An-Ming; William G
Flora of China 17: 300–332. 1994. SOLANACEAE 茄科 qie ke Zhang Zhi-yun, Lu An-ming; William G. D'Arcy Herbs, shrubs, small trees, or climbers. Stems sometimes prickly, rarely thorny; hairs simple, branched, or stellate, sometimes glandular. Leaves alternate, solitary or paired, simple or pinnately compound, without stipules; leaf blade entire, dentate, lobed, or divided. Inflorescences terminal, overtopped by continuing axes, appearing axillary, extra-axillary, or leaf opposed, often apparently umbellate, racemose, paniculate, clustered, or solitary flowers, rarely true cymes, sometimes bracteate. Flowers mostly bisexual, usually regular, 5-merous, rarely 4- or 6–9-merous. Calyx mostly lobed. Petals united. Stamens as many as corolla lobes and alternate with them, inserted within corolla, all alike or 1 or more reduced; anthers dehiscing longitudinally or by apical pores. Ovary 2–5-locular; placentation mostly axile; ovules usually numerous. Style 1. Fruiting calyx often becoming enlarged, mostly persistent. Fruit a berry or capsule. Seeds with copious endosperm; embryo mostly curved. About 95 genera with 2300 species: best represented in western tropical America, widespread in temperate and tropical regions; 20 genera (ten introduced) and 101 species in China. Some species of Solanaceae are known in China only by plants cultivated in ornamental or specialty gardens: Atropa belladonna Linnaeus, Cyphomandra betacea (Cavanilles) Sendtner, Brugmansia suaveolens (Willdenow) Berchtold & Presl, Nicotiana alata Link & Otto, and Solanum jasminoides Paxton. Kuang Ko-zen & Lu An-ming, eds. 1978. Solanaceae. Fl. Reipubl. Popularis Sin. 67(1): 1–175. 1a. Flowers in several- to many-flowered inflorescences; peduncle mostly present and evident. 2a. Fruit enclosed in fruiting calyx. -

Revision of Solanum Section Cyphomandropsis (Solanaceae) Author(S): Lynn Bohs Source: Systematic Botany Monographs, Vol
Revision of Solanum Section Cyphomandropsis (Solanaceae) Author(s): Lynn Bohs Source: Systematic Botany Monographs, Vol. 61, Revision of Solanum Section Cyphomandropsis ( Solanaceae) (Aug. 30, 2001), pp. 1-85 Published by: American Society of Plant Taxonomists Stable URL: http://www.jstor.org/stable/25027891 Accessed: 02-03-2016 19:03 UTC Your use of the JSTOR archive indicates your acceptance of the Terms & Conditions of Use, available at http://www.jstor.org/page/ info/about/policies/terms.jsp JSTOR is a not-for-profit service that helps scholars, researchers, and students discover, use, and build upon a wide range of content in a trusted digital archive. We use information technology and tools to increase productivity and facilitate new forms of scholarship. For more information about JSTOR, please contact [email protected]. American Society of Plant Taxonomists is collaborating with JSTOR to digitize, preserve and extend access to Systematic Botany Monographs. http://www.jstor.org This content downloaded from 169.237.45.23 on Wed, 02 Mar 2016 19:03:20 UTC All use subject to JSTOR Terms and Conditions REVISION OF SOLANUM SECTION CYPHOMANDROPSIS (SOLANACEAE) Lynn Bohs Department of Biology University of Utah Salt Lake City, Utah 84112 ABSTRACT. Solanum section Cyphomandropsis (Solanaceae) includes 13 species native to South Amer ica. Plants of this section are woody shrubs to small trees that lack spines, are glabrous to pubescent with un branched or dendritically branched trichomes, and have tapered anthers with small terminal pores. Section Cyphomandropsis is closely related to Solanum sect. Pachyphylla (formerly genus Cyphomandra), from which it differs by lacking discrete, enlarged connectives on the abaxial anther surfaces. -
Vegetation Community Monitoring at Congaree National Park: 2014 Data Summary
National Park Service U.S. Department of the Interior Natural Resource Stewardship and Science Vegetation Community Monitoring at Congaree National Park 2014 Data Summary Natural Resource Data Series NPS/SECN/NRDS—2016/1016 ON THIS PAGE Tiny, bright yellow blossoms of Hypoxis hirsuta grace the forest floor at Congaree National Park. Photograph courtesy of Sarah C. Heath, Southeast Coast Network. ON THE COVER Spiraling compound leaf of green dragon (Arisaema dracontium) at Congaree National Park. Photograph courtesy of Sarah C. Heath, Southeast Coast Network Vegetation Community Monitoring at Congaree National Park 2014 Data Summary Natural Resource Data Series NPS/SECN/NRDS—2016/1016 Sarah Corbett Heath1 and Michael W. Byrne2 1National Park Service Southeast Coast Inventory and Monitoring Network Cumberland Island National Seashore 101 Wheeler Street Saint Marys, GA 31558 2National Park Service Southeast Coast Inventory and Monitoring Network 135 Phoenix Drive Athens, GA 30605 May 2016 U.S. Department of the Interior National Park Service Natural Resource Stewardship and Science Fort Collins, Colorado The National Park Service, Natural Resource Stewardship and Science office in Fort Collins, Colorado, publishes a range of reports that address natural resource topics. These reports are of interest and applicability to a broad audience in the National Park Service and others in natural resource management, including scientists, conservation and environmental constituencies, and the public. The Natural Resource Data Series is intended for the timely release of basic data sets and data summaries. Care has been taken to assure accuracy of raw data values, but a thorough analysis and interpretation of the data has not been completed. -
Dichotomous Keys to the Species of Solanum L
A peer-reviewed open-access journal PhytoKeysDichotomous 127: 39–76 (2019) keys to the species of Solanum L. (Solanaceae) in continental Africa... 39 doi: 10.3897/phytokeys.127.34326 RESEARCH ARTICLE http://phytokeys.pensoft.net Launched to accelerate biodiversity research Dichotomous keys to the species of Solanum L. (Solanaceae) in continental Africa, Madagascar (incl. the Indian Ocean islands), Macaronesia and the Cape Verde Islands Sandra Knapp1, Maria S. Vorontsova2, Tiina Särkinen3 1 Department of Life Sciences, Natural History Museum, Cromwell Road, London SW7 5BD, UK 2 Compa- rative Plant and Fungal Biology Department, Royal Botanic Gardens, Kew, Richmond, Surrey TW9 3AE, UK 3 Royal Botanic Garden Edinburgh, 20A Inverleith Row, Edinburgh EH3 5LR, UK Corresponding author: Sandra Knapp ([email protected]) Academic editor: Leandro Giacomin | Received 9 March 2019 | Accepted 5 June 2019 | Published 19 July 2019 Citation: Knapp S, Vorontsova MS, Särkinen T (2019) Dichotomous keys to the species of Solanum L. (Solanaceae) in continental Africa, Madagascar (incl. the Indian Ocean islands), Macaronesia and the Cape Verde Islands. PhytoKeys 127: 39–76. https://doi.org/10.3897/phytokeys.127.34326 Abstract Solanum L. (Solanaceae) is one of the largest genera of angiosperms and presents difficulties in identifica- tion due to lack of regional keys to all groups. Here we provide keys to all 135 species of Solanum native and naturalised in Africa (as defined by World Geographical Scheme for Recording Plant Distributions): continental Africa, Madagascar (incl. the Indian Ocean islands of Mauritius, La Réunion, the Comoros and the Seychelles), Macaronesia and the Cape Verde Islands. Some of these have previously been pub- lished in the context of monographic works, but here we include all taxa. -

Southern Garden History Plant Lists
Southern Plant Lists Southern Garden History Society A Joint Project With The Colonial Williamsburg Foundation September 2000 1 INTRODUCTION Plants are the major component of any garden, and it is paramount to understanding the history of gardens and gardening to know the history of plants. For those interested in the garden history of the American south, the provenance of plants in our gardens is a continuing challenge. A number of years ago the Southern Garden History Society set out to create a ‘southern plant list’ featuring the dates of introduction of plants into horticulture in the South. This proved to be a daunting task, as the date of introduction of a plant into gardens along the eastern seaboard of the Middle Atlantic States was different than the date of introduction along the Gulf Coast, or the Southern Highlands. To complicate maters, a plant native to the Mississippi River valley might be brought in to a New Orleans gardens many years before it found its way into a Virginia garden. A more logical project seemed to be to assemble a broad array plant lists, with lists from each geographic region and across the spectrum of time. The project’s purpose is to bring together in one place a base of information, a data base, if you will, that will allow those interested in old gardens to determine the plants available and popular in the different regions at certain times. This manual is the fruition of a joint undertaking between the Southern Garden History Society and the Colonial Williamsburg Foundation. In choosing lists to be included, I have been rather ruthless in expecting that the lists be specific to a place and a time. -

Chemical and Nutrient Characterization of Solanum Pseudocapsicum Berries
African Journal of Biotechnology Vol. 4 (11), pp. 1300-1303, November 2005 Available online at http://www.academicjournals.org/AJB ISSN 1684–5315 © 2005 Academic Journals Full Length Research Paper Chemical and nutrient characterization of Solanum pseudocapsicum berries A. A. Aliero, D. S. Grierson and A. J. Afolayan* Department of Botany, University of Fort Hare, Alice, 5700, South Africa. Accepted 4 August, 2005 Solanum pseudocapsicum is a poisonous plant, yet it is used in traditional medicine topically for the treatment of boils and gonorrhoea, and orally as male tonic and for abdominal pain. Chemical analyses of the berries were carried out by GC-MS and photometric procedures. Twenty-five components were identified from the GC-MS spectra, constituting 99.80% of the extract composition. The major components were predominated by alkaloids (38.55%), hydrocarbons (22.18%), fatty acid (19.38%), alcohol (13.27%), and carboxylic acids derivatives (3.73%). The results of the mineral nutrient evaluation showed that the berries contains substantial amount of phosphorous and nitrogen. The majority of the components identified in this plant are known to be poisonous, which explains the toxic nature of these berries on animals including human beings. The possible exploitation of these components as a source of pharmaceutical and biodegradable industrial raw material is discussed. Key words: Solanum pseudocapsicum, berries, chemical composition, alkaloids nutrients. INTRODUCTION Solanum pseudocapsicum L. (Solanaceae), known as and McDonald, 1997; Parisi and Farancia, 2000; Watson winter cherry, is a poisonous plant. It is often cultivated et al., 2004). However, phytomedical investigations of the as an indoor ornamental plant due to its beautiful but species have revealed that the plant possesses cytotoxic, poisonous berries.