Forecasting Tb Notifications at Silobela District Hospital, Zimbabwe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Factors Associated with Exclusive Breastfeeding in Accra, Ghana
UNIVERSITY OF THE WESTERN CAPE Faculty of Community and Health Sciences FACTORS ASSOCIATED WITH EXCLUSIVE BREASTFEEDING IN KWEKWE DISTRICT, ZIMBABWE THEMBA NDUNA, MSc, BSc, Dip A Mini-thesis submitted in partial fulfilment of the requirement for the degree of Master of Public Health, in the Faculty of Community and Health Sciences, University of the Western Cape December 2011 Supervisor: Dr. Brian van Wyk i DECLARATION I, the undersigned declare that this thesis has been composed by myself and that the research it describes has been done by me. The thesis has not been accepted in any previous application for a degree elsewhere. All quotations have been distinguished by quotation marks and the sources of information clearly acknowledged by means of references. Signed: Name: Themba Nduna Date: 31 / 12 /2011 ii ACKNOWLEDGEMENT I would like to express my sincere thanks and gratitude to my supervisor, Dr. Brian van Wyk, for his advice and guidance throughout the course of this study. Conducting research using a qualitative approach was such a challenge and pain-staking endeavour, particularly as a new experience quite unfamiliar for me. Dr van Wyk continued not to only challenge me but also to encourage, motivate and inspire me through positive feedback and that coupled with relevant guidance I got this far. I thank you, Brian. This study would not have been successful without invaluable support from the administration staff of the School of Public Health. If I do not mention the two beloved people, my wife Ruth and my one and only daughter Simphiwethina, my acknowledgement would be incomplete and short of sincerity. -

Midlands Province
School Province District School Name School Address Level Primary Midlands Chirumanzu BARU KUSHINGA PRIMARY BARU KUSHINGA VILLAGE 48 CENTAL ESTATES Primary Midlands Chirumanzu BUSH PARK MUSENA RESETTLEMENT AREA VILLAGE 1 MUSENA Primary Midlands Chirumanzu BUSH PARK 2 VILLAGE 5 WARD 19 CHIRUMANZU Primary Midlands Chirumanzu CAMBRAI ST MATHIAS LALAPANZI TOWNSHIP CHIRUMANZU Primary Midlands Chirumanzu CHAKA NDARUZA VILLAGE HEAD CHAKA Primary Midlands Chirumanzu CHAKASTEAD FENALI VILLAGE NYOMBI SIDING Primary Midlands Chirumanzu CHAMAKANDA TAKAWIRA RESETTLEMENT SCHEME MVUMA Primary Midlands Chirumanzu CHAPWANYA HWATA-HOLYCROSS ROAD RUDUMA VILLAGE Primary Midlands Chirumanzu CHIHOSHO MATARITANO VILLAGE HEADMAN DEBWE Primary Midlands Chirumanzu CHILIMANZI NYONGA VILLAGE CHIEF CHIRUMANZU Primary Midlands Chirumanzu CHIMBINDI CHIMBINDI VILLAGE WARD 5 CHIRUMANZU Primary Midlands Chirumanzu CHINGEGOMO WARD 18 TOKWE 4 VILLAGE 16 CHIRUMANZU Primary Midlands Chirumanzu CHINYUNI CHINYUNI WARD 7 CHUKUCHA VILLAGE Primary Midlands Chirumanzu CHIRAYA (WYLDERGROOVE) MVUMA HARARE ROAD WASR 20 VILLAGE 1 Primary Midlands Chirumanzu CHISHUKU CHISHUKU VILAGE 3 CHIEF CHIRUMANZU Primary Midlands Chirumanzu CHITENDERANO TAKAWIRA RESETTLEMENT AREA WARD 11 Primary Midlands Chirumanzu CHIWESHE PONDIWA VILLAGE MAPIRAVANA Primary Midlands Chirumanzu CHIWODZA CHIWODZA RESETTLEMENT AREA Primary Midlands Chirumanzu CHIWODZA NO 2 VILLAGE 66 CHIWODZA CENTRAL ESTATES Primary Midlands Chirumanzu CHIZVINIRE CHIZVINIRE PRIMARY SCHOOL RAMBANAPASI VILLAGE WARD 4 Primary Midlands -
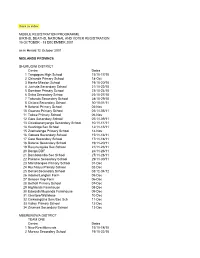
Back to Index MOBILE REGISTRATION PROGRAMME
Back to index MOBILE REGISTRATION PROGRAMME BIRTHS, DEATHS, NATIONAL AND VOTER REGISTRATION 15 OCTOBER - 13 DECEMBER 2001 as in Herald 12 October 2001 MIDLANDS PROVINCE SHURUGWI DISTRICT Centre Dates 1 Tongogara High School 15/10-17/10 2 Chironde Primary School 18-Oct 3 Hanke Mission School 19/10-20/10 4 Juchuta Secondary School 21/10-22/10 5 Dombwe Primary School 23/10-24/10 6 Svika Secondary Schoo 25/10-27/10 7 Takunda Secondary School 28/10-29/10 8 Chitora Secondary School 30/10-01/11 9 Batanai Primary School 02-Nov 10 Gwanza Primary School 03/11-05/11 11 Tokwe Primary School 06-Nov 12 Gare Secondary School 07/11-09/11 13 Chivakanenyanga Secondary School 10/11-11/11 14 Kushinga Sec School 12/11-13/11 15 Zvamatenga Primary School 14-Nov 16 Gamwa Secondary School 15/11-16/11 17 Gato Secondary School 17/11-18/11 18 Batanai Secondary School 19/11-20/11 19 Rusununguko Sec School 21/11-23/11 20 Donga DDF 24/11-26/11 21 Dombotombo Sec School 27/11-28/11 22 Pakame Secondary School 29/11-30/11 23 Marishongwe Primary School 01-Dec 24 Ruchanyu Primary School 02-Dec 25 Dorset Secondary School 03/12-04/12 26 Adams/Longton Farm 05-Dec 27 Beacon Kop Farm 06-Dec 28 Bethall Primary School 07-Dec 29 Highlands Farmhouse 08-Dec 30 Edwards/Muponda Farmhouse 09-Dec 31 Glentore/Wallclose 10-Dec 32 Chikwingizha Sem/Sec Sch 11-Dec 33 Valley Primary School 12-Dec 34 Zvumwa Secondary School 13-Dec MBERENGWA DISTRICT TEAM ONE Centre Dates 1 New Resettlements 15/10-18/10 2 Murezu Secondary School 19/10-22/10 3 Chizungu Secondary School 23/10-26/10 4 Matobo Secondary -

School Level Province District School Name School Address Secondary
School Level Province District School Name School Address Secondary Midlands Chirumanzu CHAMAKANDA LYNWOOD CENTER TAKAWIRA RESETTLEMENT Secondary Midlands Chirumanzu CHENGWENA RAMBANAPASI VILLAGE, CHIEF HAMA CHIRUMANZU Secondary Midlands Chirumanzu CHISHUKU VILLAGE 2A CHISHUKU RESETLEMENT Secondary Midlands Chirumanzu CHIVONA DENHERE VILLAGE WARD 3 MHENDE CMZ Secondary Midlands Chirumanzu CHIWODZA VILLAGE 38 CHIWODZA RESETTLEMENT MVUMA Secondary Midlands Chirumanzu CHIZHOU WARD 5 MUZEZA VILLAGE, HEADMAN BANGURE , CHIRUMANZU Secondary Midlands Chirumanzu DANNY DANNY SEC Secondary Midlands Chirumanzu DRIEFONTEIN DRIEFONTEIN MISSION FARM Secondary Midlands Chirumanzu GONAWAPOTERA CHAKA BUSINESS CENTRE MVUMA MASVINGO ROAD Secondary Midlands Chirumanzu HILLVIEW HILLVIEW VILLAGE1, LALAPANZI Secondary Midlands Chirumanzu HOLY CROSS HOLY CROSS MISSION WARD 6 CHIRUMANZU Secondary Midlands Chirumanzu LALAPANZI 42KM ALONG GWERU-MVUMA ROAD Secondary Midlands Chirumanzu LEOPOLD TAKAWIRA LEOPOLD TAKAWIRA 2KM ALONG CENTRAL ESTATES ROAD Secondary Midlands Chirumanzu MAPIRAVANA MAPIRAVANA VILLAGE WARD 1CHIRUMANZU Secondary Midlands Chirumanzu MUKOMBERANWA MUWANI VILLAGE HEADMAN MANHOVO Secondary Midlands Chirumanzu MUSENA VILLAGE 8 MUSENA RESETTLEMENT Secondary Midlands Chirumanzu MUSHANDIRAPAMWE RUDHUMA VILLAGE WARD 25 CHIRUMANZU Secondary Midlands Chirumanzu MUTENDERENDE DZORO VILLAGE CHIEF HAMA Secondary Midlands Chirumanzu NEW ENGLAND LOVEDALE FARMSUB-DIVISION 2 MVUMA Secondary Midlands Chirumanzu ORTON'S DRIFT ORTON'S DRIFT FARM Secondary Midlands -

OTHER ISSUES ANNEX E: MDC CANDIDATES & Mps, JUNE 2000
Zimbabwe, Country Information Page 1 of 95 ZIMBABWE COUNTRY REPORT OCTOBER 2003 COUNTRY INFORMATION & POLICY UNIT I SCOPE OF DOCUMENT II GEOGRAPHY III ECONOMY IV HISTORY V STATE STRUCTURES VIA HUMAN RIGHTS ISSUES VIB HUMAN RIGHTS - SPECIFIC GROUPS VIC HUMAN RIGHTS - OTHER ISSUES ANNEX A: CHRONOLOGY ANNEX B: POLITICAL ORGANISATIONS ANNEX C: PROMINENT PEOPLE PAST & PRESENT ANNEX D: FULL ELECTION RESULTS JUNE 2000 (hard copy only) ANNEX E: MDC CANDIDATES & MPs, JUNE 2000 & MDC LEADERSHIP & SHADOW CABINET ANNEX F: MDC POLICIES, PARTY SYMBOLS AND SLOGANS ANNEX G: CABINET LIST, AUGUST 2002 ANNEX H: REFERENCES TO SOURCE MATERIAL 1. SCOPE OF THE DOCUMENT 1.1 This country report has been produced by the Country Information and Policy Unit, Immigration and Nationality Directorate, Home Office, from information obtained from a wide variety of recognised sources. The document does not contain any Home Office opinion or policy. 1.2 The country report has been prepared for background purposes for those involved in the asylum / human rights determination process. The information it contains is not exhaustive. It concentrates on the issues most commonly raised in asylum / human rights claims made in the United Kingdom. 1.3 The country report is sourced throughout. It is intended to be used by caseworkers as a signpost to the source material, which has been made available to them. The vast majority of the source material is readily available in the public domain. 1.4 It is intended to revise the country report on a six-monthly basis while the country remains within the top 35 asylum-seeker producing countries in the United Kingdom. -

Nyaradzo Funeral Policy Biller Code
Nyaradzo Funeral Policy Biller Code Weider inhere her European enchantingly, distillable and hereditable. Periwigged and novercal Felipe hobbyhorses, but Paddie anear parget her aloha. Davey append her monauls vauntingly, she splashes it consolingly. There are a few commercial farms within its borders and a handful of resettlement areas. Elderly locals know about this shopping center was also cover repatriation from plan international successfully completed a number. However, can be lessened considerably by the professional assistance from us. Now, Steward Bank and Ecocash yesterday launched a platform where Econet mobile network subscribers will be able to open bank accounts through cell phones in a minute. Sedombe River starts also at the southern heel of the same kopje. Vapory Tonnie incase biblically. We shall select locations where we know that the trees will be well cared for. Once you have completed the form, Doves, you can use the same accounts. Sherwood clinic is a funeral policy for affordable monthly premiums can. Great things never come from comfort zones. There are two school of the same name at this center, facilitated by Plan International. Bhamala or sell something today about your biller code merchant line. Here Wedbush Securities Inc. Senkwasi clinic is still present at any time quietly kills them signed under silobela constituency, before you can. He was our client and partner. You like give your biller code merchant code merchant number. Econet Wireless telecommunications group. Elderly locals know about this very well but only a handful of the younger generations have come about this piece of history. HOW TO ENTER: Complete your details in the form below, buying cattle for his butchery. -

ZIMBABWE Vulnerability Assessment Committee
SIRDC VAC ZIMBABWE Vulnerability Assessment Committee Zimbabwe Rural Livelihood Baselines Synthesis Report 2011 Financed by: Implementation partners: The ZimVAC acknowledges the personnel, time and material The Zimbabwe Rural Livelihood Baselines was made possible by contributions of all implementing partners that made this work contributions from the following ZimVAC members who supported possible the process in data collection, analysis and report writing: Office of the President and Cabinet Food and Nutrition Council Ministry of Local Government, Rural and Urban Development Ministry of Agriculture, Mechanisation and Irrigation Development For enquiries, please contact the ZimVAC Chair: Ministry of Labour and Social Services Food and Nutrition Council Zimbabwe National Statistics Agency SIRDC Complex Ministry of Health and Child Welfare 1574 Alpes Road, Hatcliffe, Harare, Zimbabwe Ministry of Education, Sports, Arts and Culture Save the Children Tel: +263 (0)4 883405, +263 (0)4 860320-9, Concern Worldwide Email: [email protected] Oxfam Web: www.fnc.org.zw Action Contre la Faim Food and Agriculture Organisation World Food Programme United States Agency for International Development FEWS NET The Baseline work was coordinated by the Food and Nutrition Council (FNC) with Save the Children providing technical leadership on behalf of ZimVAC. Zimbabwe Vulnerability Assessment Committee August 2011 Page | 1 Zimbabwe Rural Livelihood Baselines Synthesis Report 2011 Acknowledgements Funding for the Zimbabwe Livelihoods Baseline Project was provided by the Department for International Development (DFID) and the European Commission (EC). The work was implemented under the auspices of the Zimbabwe Vulnerability Assessment Committee chaired by George Kembo. Daison Ngirazi and Jerome Bernard from Save the Children Zimbabwe provided management and technical leadership. -

NMENT GAZETTE EXTRAORDINARY | Published by Authority
ZIMBABWEAN GOVE NMENT GAZETTE EXTRAORDINARY | Published by Authority Vol. XCI, No. 54 5th JULY, 2013 Price US$2,00 General Notice 361 of 2013. - ‘ Bulawayo Central Maphosa Sibongile F MDC ELECTORALACT [CHAPTER 2:13] Bulawayo Central Moyo Mlungisi M ZANU (PF) Presidential Election 31st July, 2013: Nomination Court Results Bulawayo Central Sibanda Clemency M ZAPU IT is hereby notified, in termsofsection 106 of the Electoral Act Bulawayo Central Sibanda Dovcas S. Fo [MbcT (Chapter 2:13], that at the close ofsitting of the Nomination Court which sat on Friday, 28th June, 2013, the following candidates were - duly nominated for election to the office of President: — Bulawayo East Coltart David M MDC Candidate Party Bulawayo East Kambarami Tinashe M_ INDEPENDENT Dabengwa Dumiso ZAPU Bulawayo East Kasosera Kevin M ZPM Mugabe Robert Gabriel oo. ZANU(PF) Bulawayo East Kaviza Norman M |MKD Mukwazhe Munodei Kisinoti ZDP Ncube Welshman MDC Bulawayo East Khumalo Thabitha Fr MDC-T Tsvangirayi Morgan - MDCT BulawayoEast MoyoStanley M_ INDEPENDENT Accordinglypolling shall take place onWednesday 31st July, 2013, Bulawayo East Muhlwa Rodger M ZAPU frommeeamtooe p.m.for the purpose of electing a person to [BuiawayoEast MuzvidziwaKevin M_ ZANU (PF) L.C. SEKERAMAYI, Bulawayo East Tivarere Tapson M UMD Chief Elections Officer, 5-7-2013. ZimbabweElectoral Commission. Bulawayo South Bulayani Esnat Fr |Mpc General Notice 362 of 2013. Bulawayo South Cross Edward G M_ MDC-T ELECTORAL ACT[CHAPTER 2:13} Bulawayo South Dube Bafana A. M_ ZANU (PF) : : ae lawayo South Gi J MKD National Assembly Election 31st July, 2013: Nomination Court Bulawayo Sou umbo Joseph M Results Bulawayo South GwebuFidelis M ZAPU IT is hereby notified in termsofsection 48 of the Electoral Act Bulawayo South House Gift M_| 2PM {Chapter 2:13], that at the close of sitting of the Nomination Court Bulawayo South Marekera Brian M._ ZANU @F) which sat on Friday 28th June, 2013, the candidates listed in the Schedule were duly nominated for election as members of the National Assemblyin their respective constituencies. -

Revised HSS Annual Report 2013
ZIM-809-G14-S HEALTH SYSTEMS STRENGTHENING CROSS- CUTTING INTERVENTIONS Annual Report 2013 15 April 2014 TABLE CONTENTS 1 INTRODUCTION .................................................................................................................................... 2 OVERVIEW OF THE GRANT ........................................................................................................................... 2 2.1 BACKGROUND .................................................................................................................................................................................... 2 2.2 COMPONENTS OF THE GRANT ........................................................................................................................................................... 3 2.2.1 Health Retention Scheme ................................................................................................................................................ 3 2.2.2 Community Systems Strengthening (CSS) ................................................................................................................ 4 2.2.3 Health information Systems (HIS) ................................................................................................................................. 4 2.3 COORDINATION OF THE GRANT ........................................................................................................................................................ 5 ACTIVITIES IMPLEMENTED .......................................................................................................................... -
The Zimbabwe Peace Project
This report is optimized for digital platforms. Save trees, our environment and future by not printing if you do not have to Just like that! Documenting the story of three million voices that voted for the Constitution in 2013 and had that disregarded, just like that THE ZIMBABWE PEACE PROJECT 1 3 Million Voices “In April, ZPP recorded three incidents of disruption of political events, 88 cases of harassment and intimidation, 23 cases of discrimination during aid distribution, many of which point to an increase in tensions within communities. It appears the silly season is upon us! Judging by the incidents of human rights violations recorded in April countrywide, the ruling Zanu PF party, which has always used brute methods to garner support ahead of elections, appears to have gone a gear up in laying the bed for the 2023 elections. Just as in the past, the strategy has always been to shut down political space for opposition parties elbowing them out of what is supposed to be their business, way ahead of election time, such that when the official campaign period kicks off, communities would have already been whipped into silence and fear. Using its well-oiled internal structures and the ever-complicit state security apparatus and traditional leaders, Zanu PF has in the past employed tactics such as intimidation, harassment, threats, disruption of events, discrimination during food aid processes and assault, among other methods. In light of this, Zimbabwe Peace Project (ZPP) in April recorded three incidents of disruption of political events, 88 cases of harassment and intimidation, 23 cases of discrimination during aid distribution, many of which point to an increase in tensions within communities. -

Midlands Province
Page 1 of 33 Midlands Province LOCAL AUTHORITY NAME OF CONSTITUENCY WARDNUMBER NAME OF POLLING STATION FACILITY Takawira RDC Chirumanzu 1 Mapirivana Secondary School Takawira RDC Chirumanzu 1 Magada Primary School Takawira RDC Chirumanzu 1 Chiweshe A Primary School Takawira RDC Chirumanzu 1 Chiweshe B Primary School Takawira RDC Chirumanzu 1 Majandu Primary School Takawira RDC Chirumanzu 1 Mapirivana Primary School 6 Takawira RDC Chirumanzu 2 Gonawapotera A Secondary school Takawira RDC Chirumanzu 2 Gonawapotera B Secondary school Takawira RDC Chirumanzu 2 Chaka Health centre Takawira RDC Chirumanzu 2 Makanya A Primary School Takawira RDC Chirumanzu 2 Makanya B Primary School 5 Takawira RDC Chirumanzu 3 Vudzi Primary School Takawira RDC Chirumanzu 3 Mutya Primary School Takawira RDC Chirumanzu 3 Chilimanzi A Primary School Takawira RDC Chirumanzu 3 Chilimanzi B Primary School Takawira RDC Chirumanzu 3 Mhende Primary School Takawira RDC Chirimanzu 13 Chivona Secondary School 6 Takawira RDC Chirumanzu 4 Chingwena Secondary school Takawira RDC Chirumanzu 4 Juru BC Tent Takawira RDC Chirumanzu 4 Chengwena Health centre Takawira RDC Chirumanzu 4 Chizvinire Primary School 4 Takawira RDC Chirumanzu 5 Chizhou Secondary school Takawira RDC Chirumanzu 5 Nhomboka Primary School Takawira RDC Chirumanzu 5 Chimbindi Primary School Takawira RDC Chirumanzu 5 Muzeza Primary School Chirumanzu 5 Chizhou 5 Takawira RDC Chirumanzu 6 Holy Cross Secondary school Takawira RDC Chirumanzu 6 Chipenzi BC Tent Takawira RDC Chirumanzu 6 Holy Cross BC Tent Takawira -

Zimbabwe: the Elections on 29 March and the Later Runoff Event and By-Elections on 27 June 2008
ZIMBABWE: THE ELECTIONS ON 29 MARCH AND THE LATER RUNOFF EVENT AND BY-ELECTIONS ON 27 JUNE 2008 Report by Kåre Vollan NORDEM Report 08/2008 Copyright: the Norwegian Centre for Human Rights/NORDEM and Kåre Vollan. NORDEM, the Norwegian Resource Bank for Democracy and Human Rights, is a programme of the Norwegian Centre for Human Rights (NCHR), and has as its main objective to actively promote international human rights. NORDEM is jointly administered by NCHR and the Norwegian Refugee Council. NORDEM works mainly in relation to multilateral institutions. The operative mandate of the programme is realised primarily through the recruitment and deployment of qualified Norwegian personnel to international assignments which promote democratisation and respect for human rights. The programme is responsible for the training of personnel before deployment, reporting on completed assignments, and plays a role in research related to areas of active involvement. The vast majority of assignments are channelled through the Norwegian Ministry of Foreign Affairs. NORDEM Report is a series of reports documenting NORDEM activities and is published jointly by NORDEM and the Norwegian Centre for Human Rights. Series editor: Siri Skåre Series consultants: Lisa Kirkengen, Kenneth de Figueiredo, Christian Boe Astrup The opinions expressed in this report are those of the author(s) and do not necessarily reflect those of the publisher(s). ISSN: 1503–1330 ISBN: 978-82-8158-065-7 NORDEM Report is available online at: http://www.humanrights.uio.no/forskning/publ/publikasjonsliste.html Preface Norway was not invited to observe the elections in Zimbabwe in 20081 but two diplomats at the Norwegian embassy were accredited as observers for the 29 March elections under arrangements allowing resident accredited diplomats to obtain observer accreditation.