Non-Dominant Primary Motor Cortex Repetitive Transcranial Magnetic Stimulation for Moderate to Severe Chronic Pain Caused by Diabetic Neuropathy: Case Series from a Small Crossover
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
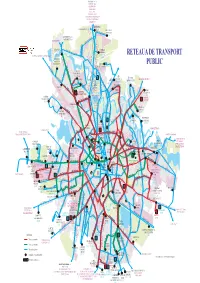
RETEA GENERALA 01.07.2021.Cdr
OTOPENI 780 783 OSTRATU R441 OTOPENI R442 PERIS R443 PISCU R444 GRUIU R446 R447 MICSUNESTII MARI R447B MOARA VLASIEI R448 SITARU 477 GREENFIELD STRAULESTI 204 304 203 204 Aleea PrivighetorilorJOLIE VILLE BANEASA 301 301 301 GREENFIELD 204 BUFTEA R436 PIATA PRESEI 304 131 Str. Jandarmeriei261 304 STRAULESTI Sos. Gh. Ionescu COMPLEX 97 204 205 304 261 Sisesti BANEASA RETEAUA DE TRANSPORT R402 205 131 261 335 BUFTEA GRADISTEA SITARU R402 261 205 R402 R436 Bd. OaspetilorStr. Campinita 361 605 COMPLEX 112 205 261 97 131 261301 COMERCIAL Sos. Bucuresti Ploiesti PUBLIC COLOSSEUM CARTIER 231 Sos. Chitilei Bd. Bucurestii Noi Sos. Straulesti R447 R447B R448 R477 203 335 361 605 780 783 112 R441 R442 R443 R444HENRI R446 COANDA 231 Bd. Aerogarii R402 97 605 231 112 112 CARTIER 112 301 112 DAMAROAIA 131 R436 335 231 Sos. Chitilei R402 24 331R436 CFR Str. Alex. Serbanescu 112 CONSTANTA CARTIER MERII PETCHII R409 112 DRIDU Str. N. Caramfil R402 Bd. Laminorului AUTOBAZA ANDRONACHE 331 65 86 112 135 243 Bd. NORDULUI112 301 382 Bd. Gloriei24 Str. Jiului 605 Sos. 112Pipera 135 Sos. Chitilei Poligrafiei PIATA PLATFORMA Bd. BucurestiiPajurei Noi 231 243 Str. Peris MEZES 780 783 INDUSTRIALA Str. PRESEI Str.Oi 3 45 65 86 331 243 3 45 382 PASAJ Sos. Bucuresti Ploiesti 3 41 243 PIPERA 382 DEPOUL R447 R447BR448 R477 112 231 243 i 65 86 97 243 16 36 COLENTINA 131105 203 205 261203 304 231 261 304 330 135 343 n tuz BUCURESTII NOI a R441 R442 R443 c 21 i CARTIER 605 tr 231R441 361 R442 783 R443 R444 R446 DEPOUL Bd. -

6. Public Transport
ROMANIA Reimbursable Advisory Services Agreement on the Bucharest Urban Development Program (P169577) COMPONENT 1. ELABORATION OF BUCHAREST’S IUDS, CAPITAL INVESTMENT PLANNING AND MANAGEMENT Output 3. Urban context and identification of key local issues and needs, and visions and objectives of IUDS and Identification of a long list of projects. A. Rapid assessment of the current situation Section 4. Mobility and Transport March 2021 DISCLAIMER This report is a product of the International Bank for Reconstruction and Development/the World Bank. The findings, interpretations and conclusions expressed in this paper do not necessarily reflect the views of the Executive Directors of the World Bank or the governments they represent. The World Bank does not guarantee the accuracy of the data included in this work. This report does not necessarily represent the position of the European Union or the Romanian Government. COPYRIGHT STATEMENT The material in this publication is copyrighted. Copying and/or transmitting portions of this work without permission may be a violation of applicable laws. For permission to photocopy or reprint any part of this work, please send a request with the complete information to either: (i) the Municipality of Bucharest (47 Regina Elisabeta Blvd., Bucharest, Romania); or (ii) the World Bank Group Romania (Vasile Lascăr Street 31, FL. 6, Sector 2, Bucharest, Romania). This report was delivered in March 20221 under the Reimbursable Advisory Services Agreement on the Bucharest Urban Development Program, concluded between the Municipality of Bucharest and the International Bank for Reconstruction and Development on March 4, 2019. It is part of Output 3 under the above-mentioned agreement – Urban context and identification of key local issues and needs, and visions and objectives of IUDS and Identification of a long list of projects – under Component 1, which refers to the elaboration of Bucharest’s Integrated Urban Development Strategy, Capital Investment Planning and Management. -

Trasee De Noapte
PROGRAMUL DE TRANSPORT PENTRU RETEAUA DE AUTOBUZE - TRASEE DE NOAPTE Plecari de la capete de Linia Nr Numar vehicule Nr statii TRASEU CAPETE lo traseu Lungime c 23 00:30 1 2 03:30 4 5 Prima Ultima Dus: Şos. Colentina, Şos. Mihai Bravu, Bd. Ferdinand, Şos. Pantelimon, Str. Gǎrii Cǎţelu, Str. N 101 Industriilor, Bd. Basarabia, Bd. 1 Dus: Decembrie1918 0 2 2 0 2 0 0 16 statii Intors: Bd. 1 Decembrie1918, Bd. 18.800 m Basarabia, Str. Industriilor, Str. Gǎrii 88 Intors: Cǎţelu, Şos. Pantelimon, Bd. 16 statii Ferdinand, Şos. Mihai Bravu, Şos. 18.400 m Colentina. Terminal 1: Pasaj Colentina 00:44 03:00 Terminal 2: Faur 00:16 03:01 Dus: Piata Unirii , Bd. I. C. Bratianu, Piata Universitatii, Bd. Carol I, Bd. Pache Protopopescu, Sos. Mihai Bravu, Str. Vatra Luminoasa, Bd. N102 Pierre de Coubertin, Sos. Iancului, Dus: Sos. Pantelimon 1 2 2 2 2 2 2 19 statii Intors: Sos. Pantelimon, Sos. Iancului, 8.400 m Bd. Pierre de Coubertin, Str. Vatra 88 Intors: Luminoasa, Sos. Mihai Bravu, Bd. 16 statii Pache Protopopescu, Bd. Carol I, 8.600 m Piata Universitatii, Bd. I. C. Bratianu, Piata Unirii. Terminal 1: Piata Unirii 2 23:30 04:40 Terminal 2: Granitul 22.55 04:40 Dus: Bd. Th. Pallady, Bd. Camil Ressu, Cal. Dudeşti, Bd. O. Goga, Str. Nerva Traian, Cal. Văcăreşti, Şos. Olteniţei, Str. Ion Iriceanu, Str. Turnu Măgurele, Str. Luică, Şos. Giurgiului, N103 Piaţa Eroii Revoluţiei, Bd. Pieptănari, us: Prelungirea Ferentari 0 2 1 0 2 0 0 24 statii Intors: Prelungirea Ferentari, , Bd. -

Pipera Neighborhood
www.ssoar.info Pipera Neighborhood - Voluntari City (Romania): problems regarding inconsistency between the residential dynamic and the street network evolution between 2002 and 2011 COSTACHE Romulus; TUDOSE Ionuț Veröffentlichungsversion / Published Version Zeitschriftenartikel / journal article Empfohlene Zitierung / Suggested Citation: COSTACHE Romulus, & TUDOSE Ionuț (2012). Pipera Neighborhood - Voluntari City (Romania): problems regarding inconsistency between the residential dynamic and the street network evolution between 2002 and 2011. Cinq Continents, 2(6), 201-215. https://nbn-resolving.org/urn:nbn:de:0168-ssoar-325228 Nutzungsbedingungen: Terms of use: Dieser Text wird unter einer CC BY-NC Lizenz (Namensnennung- This document is made available under a CC BY-NC Licence Nicht-kommerziell) zur Verfügung gestellt. Nähere Auskünfte zu (Attribution-NonCommercial). For more Information see: den CC-Lizenzen finden Sie hier: https://creativecommons.org/licenses/by-nc/4.0 https://creativecommons.org/licenses/by-nc/4.0/deed.de Volume 2 / Numéro 6 Hivér 2012 ISSN: 2247 - 2290 p. 201-215 PIPERA NEIGHBOURHOOD - VOLUNTARI CITY. PROBLEMS REGARDING INCONSISTENCY BETWEEN THE RESIDENTIAL DYNAMIC AND THE STREET NETWORK EVOLUTION BETWEEN 2002 AND 2011 Romulus COSTACHE Ionuț TUDOSE Master Std. Faculty of Geography, University of Bucharest [email protected] Contents: 1. INTRODUCTION .............................................................................................................................................................. -

Braukšanas Ierobežojumi Kravas Transportlīdzekļiem Rumānijā 2018. Gadā
Braukšanas ierobežojumi kravas transportlīdzekļiem Rumānijā 2018. gadā Vispārējie ierobežojumi: Transportlīdzekļi: Kravas transportlīdzekļi ar pilnu masu virs 7.5t; Ierobežojumu darbības zona: DN1, km 17 + 900 (Otopeni pilsētas robeža) – Ploiesti (krustojums DN1 –DN1A); Ierobežojumi spēkā: No 2018. gada 1. janvāra līdz 31. decembrim; Ierobežojumi spēkā Nr. Ceļš Ceļš Pirmdiena - Sestdiena - Piektdiena ceturtdiena svētdiena DN1, km 17 + 900 (Otopeni 1 pilsētas robeža) – Ploiesti (krustojums DN1 –DN1A) DN1 6.00 – 22.00 00.00 – 24.00 00.00 – 24.00 Ploiesti (krustojums DN1 –DN1B) 2 – Brasov (DN1 – DN1 A); Tabula nr.1 Izņēmumi: Civilās aizsardzības transportlīdzekļi, bēru transports, pirmās palīdzības un humanitārās palīdzības dienestu transportlīdzekļi, pasta pārvadājumi, degvielas pārvadājumi, specializētie avārijas transportlīdzekļi, sanitāro dienestu transportlīdzekļi. Alternatīvi maršruti: DN1A: Bucharest – Ploiesti – Brasov; A3: Bucharest – Ploiesti; DN1A: Ploiesti – Brasov; DN7: Bucharest – krustojums DN7 – DN71; DN71: krustojums DN7 – DN71 – Targoviste; DN72A: Targoviste – Stoenesti – krustojums DN72A – DN73; DN73: krustojums DN72A – DN73 – Rasnov – Brasov; Ierobežojumi vasarā Transportlīdzekļi: Kravas transportlīdzekļi ar pilnu masu virs 7.5t; Ierobežojumu darbības zona: skatīt “Tabula nr.2”; Ierobežojumi spēkā: Piektdienās, sestdienās un svētdienās, periodā no 2018. gada 1. jūlija līdz 2018. gada 31. augustam. *Uz A2 automaģistrāles braukšanas ierobežojumi attiecināmi uz kravas transportlīdzekļiem ar pilnu masu virs 3.5t. Ceļš Darbības -

CMN / EA International Provider Network HOSPITALS/CLINICS
CMN / EA International Provider Network HOSPITALS/CLINICS As of March 2010 The following document is a list of current providers. The CMN/EA International Provider Network spans approximately 200 countries and territories worldwide with over 2000 hospitals and clinics and over 6000 physicians. *Please note that the physician network is comprised of private practices, as well as physicians affiliated with our network of hospitals and clinics. Prior to seeking treatment, Members must call HCCMIS at 1-800-605-2282 or 1-317-262-2132. A designated member of the Case Management team will coordinate all healthcare services and ensure that direct billing arrangements are in place. Please note that although a Provider may not appear on this list, it does not necessarily mean that direct billing cannot be arranged. In case of uncertainty, it is advised Members call HCCMIS. CMN/EA reserves the right, without notice, to update the International Provider Network CMN/EA International Provider Network INTERNATIONAL PROVIDERS: HOSPITALS/CLINICS FacilitY Name CitY ADDRess Phone NUMBERS AFGHanistan DK-GERman MedicaL DiagnOstic STReet 66 / HOUse 138 / distRict 4 KABUL T: +93 (0) 799 13 62 10 CenteR ZOne1 ALBania T: +355 36 21 21 SURgicaL HOspitaL FOR ADULts TIRana F: +355 36 36 44 T: +355 36 21 21 HOspitaL OF InteRnaL Diseases TIRana F: +355 36 36 44 T: +355 36 21 21 PaediatRic HOspitaL TIRana F: +355 36 36 44 ALGERia 4 LOT. ALLIOULA FOdiL T: +213 (21) 36 28 28 CLiniQUE ChahRAZed ALgeR CHÉRaga F: +213 (21) 36 14 14 4 DJenane AchaBOU CLiniQUE AL AZhaR ALgeR -

Evaluation of Bucharest Soil Liquefaction Potential
Mathematical Modelling in Civil Engineering Vol. 11‐No. 1: 40‐48 – 2015 Doi: 10.1515/mmce‐2015‐0005 EVALUATION OF BUCHAREST SOIL LIQUEFACTION POTENTIAL ARION CRISTIAN - Lecturer, PhD, Technical University of Civil Engineering, e-mail: [email protected] CALARASU ELENA –Researcher, PhD, URBAN-INCERC Bucharest NEAGU CRISTIAN – Researcher, PhD Student, Technical University of Civil Engineering, e-mail: [email protected] Abstract: The paper contains the experimental research performed in Bucharest like the borehole data (Standard Penetration Test) and the data obtained from seismic investigations (down-hole prospecting and surface-wave methods). The evaluation of the soils liquefaction resistance based on the results of the SPT, down-hole prospecting and surface-wave method tests and the use of the earthquake records will be presented. Keywords: Bucharest, liquefaction, SPT, seismic prospecting 1. Introduction The Bucharest metropolitan area is located in the Romanian Plain, along the Colentina and Dambovita rivers, in the central part of the Moesian Sub-plate (age: Precambrian and Paleozoic). Over Cretaceous and Miocene deposits (having the top at about 1000 m depth) a Pliocene shallow water deposit (~700m thick) was settled. The surface geology consists mainly of Quaternary alluvial deposits with distinct peculiarities and large intervals of thickness characterize the city of Bucharest. Later loess covered these deposits and rivers shaped the present landscape [1]. The main source of earthquakes for Bucharest is the Vrancea seismic zone. When strong ground motions were recorded, they provided instrumental proofs of site effects. Site effects were firstly observed on the basis of damage pattern within the city. The borehole data and the experimental research performed in the last years revealed a new series of elements regarding the stratification and soil characteristics and of the long predominant period of soil vibration that characterize Bucharest [2]. -

City of Bucharest
City of Bucharest Intercultural Profile 1. Background1 Bucharest is the capital and largest city, as well as the cultural, industrial, and financial centre of Romania. According to the 2011 census, 1,883,425 inhabitants live within the city limits, a decrease from the 2002 census. Taking account of the satellite towns around the urban area, the proposed metropolitan area of Bucharest would have a population of 2.27 million people. However, according to unofficial data given by Wikipedia, the population is more than 3 million (raising a point that will be reiterated throughout this report that statistics are not universally reliable in Romania).Notwithstanding, Bucharest is the 6th largest city in the European Union by population within city limits, after London, Berlin, Madrid, Rome, and Paris. Bucharest accounts for around 23% of the country’s GDP and about one-quarter of its industrial production, while being inhabited by only 10% of the country’s population. In 2010, at purchasing power parity, Bucharest had a per-capita GDP of EUR 14,300, or 45% that of the European Union average and more than twice the Romanian average. Bucharest’s economy is mainly focused on industry and services, with a significant IT services sector. It houses 186,000 companies, and numerous companies have set up headquarters in Bucharest, attracted by the highly skilled labour force and low operating costs. The list includes multinationals such as Microsoft, IBM, P&G, HP, Oracle, Wipro, and S&T. In terms of higher education, Bucharest is the largest Romanian academic centre and one of the most important locales in Eastern Europe, with 16 public and 18 private institutes and over 300,00 students. -

You Drive, We Care
You drive, we care. RO - Diesel & Services Rumänien / România / Romania PLZ sortiert Sorted by ZIP code » For help, call me! DKV ASSIST - 24h International Free Call* 00800 365 24 365 In case of difficulties concerning the number 00800 please dial the relevant emergency number of the country: Bei unerwarteten Schwierigkeiten mit der Rufnummer 00800, wählen Sie bitte die Notrufnummer des Landes: Andorra / Andorra Latvia / Lettland » +34 934 6311 81 » +370 5249 1109 Austria / Österreich Liechtenstein / Liechtenstein » +43 362 2723 03 » +39 047 2275 160 Belarus / Weißrussland Lithuania / Litauen » 8 820 0071 0365 (national) » +370 5249 1109 » +7 495 1815 306 Luxembourg / Luxemburg Belgium / Belgien » +32 112 5221 1 » +32 112 5221 1 North Macedonia / Nordmazedonien Bosnia-Herzegovina / Bosnien-Herzegowina » +386 2616 5826 » +386 2616 5826 Moldova / Moldawien Bulgaria / Bulgarien » +386 2616 5826 » +359 2804 3805 Montenegro / Montenegro Croatia / Kroatien » +386 2616 5826 » +386 2616 5826 Netherlands / Niederlande Czech Republic / Tschechische Republik » +49 221 8277 9234 » +420 2215 8665 5 Norway / Norwegen Denmark / Dänemark » +47 221 0170 0 » +45 757 2774 0 Poland / Polen Estonia / Estland » +48 618 3198 82 » +370 5249 1109 Portugal / Portugal Finland / Finnland » +34 934 6311 81 » +358 9622 2631 Romania / Rumänien France / Frankreich » +40 264 2079 24 » +33 130 5256 91 Russia / Russland Germany / Deutschland » 8 800 7070 365 (national) » +49 221 8277 564 » +7 495 1815 306 Great Britain / Großbritannien Serbia / Serbien » 0 800 1975 520 -

S.C. SERVICIUL TRANSPORT VOLUNTARI S.A. Anexa 1
S.C. SERVICIUL TRANSPORT VOLUNTARI S.A. Anexa 1 ANEXA 1- PROGRAMUL DE TRANSPORT AL S.C. SERVICIUL TRANSPORT VOLUNTARI S.A. ANEXA 1.1 - PROGRAMUL DE TRANSPORT 1 PROGRAMUL DE TRANSPORT AL S.C. SERVICIUL TRANSPORT VOLUNTARI S.A. 2 ANEXA 1 PROGRAMUL DE TRANSPORT AL OPERATORULUI DE TRANSPORT S.C. SERVICIUL TRANSPORT VOLUNTARI S.A. Programul de Transport anual Km. Traseu Planificaţi Mod de Zi de Perioada de Zi de duminică și transport Zi de lucru aplicare sâmbătă sărbători legale Autobuze 28.787,616 18.047,407 17.235,647 În toate zilele din an Total Km anual planificati Autobuze 9.264.987,521 km anual *Inclusiv kilometri traseu planificați pentru acces/retragere 3 Anexa 1.1 Programul de Transport Km planificați Program normal Nr.crt Linia Zi de duminică + Zi de lucru Zi de sâmbătă sărbători legale 1 R403 1.918,97 1.183,81 1.183,81 2 R407 1.618,78 992,33 992,33 3 R409 2.565,87 1.612,92 1.612,92 4 R411 1.372,66 1.083,37 1.083,37 5 R412 1.907,27 1.124,8 1.124,8 6 R413 1.226,77 594 594 7 R416 1.423,1 651,05 651,05 8 R417 1.204,56 602,28 602,28 9 R440 1.122,833 818,382 818,382 10 R449 736,5 359,83 359,83 11 R450 948,35 670,64 670,64 12 R451 1.634,67 1.069,56 1.069,56 13 R459 1.349,238 680,83 680,83 14 R460 1.623,97 1512,7 1.213,98 15 R461 1.511,82 1.027,64 1.027,64 16 R467 1.325,32 831,75 635,82 17 R468 3.841,88 2.010,43 1.693,32 18 R473 843,39 609,42 609,42 19 R479 611,665 611,665 611,665 Km planificaţi 28.787,616 18.047,407 17.235,647 traseu / zi Nr.zile 254 49 62 Total km 9.264.987,521 planificati anual 4 INTERVAL SUCCEDARE (min.) Plecări capete de LINIA / NR. -

Driving Restrictions, Goods Transport, 2020 Austria
Driving Restrictions, Goods Transport, 2020 Austria 1. GENERAL DRIVING RESTRICTIONS Vehicles concerned Trucks with trailers, if the maximum authorised total weight of the motor vehicle or the trailer exceeds 3.5t; trucks, articulated vehicles and self- propelled industrial machines with an authorised total weight of more than 7.5t. Area Nationwide, with the exception of journeys made exclusively as part of a combined transport operation within a radius of 65km of the following transloading stations: Brennersee; Graz-Ostbahnhof; Salzburg- Hauptbahnhof; Wels-Verschiebebahnhof; Villach-Fürnitz; Wien- Südbahnhof; Wien-Nordwestbahnhof; Wörg; Hall in Tirol CCT; Bludenz CCT; Wolfurt CCT. Prohibition Saturdays from 15h00 to 24h00; Sundays and public holidays from 00h00 to 22h00 Public holidays 2020 1 Jan New Year's Day 6 Jan Epiphany 13 Apr Easter Monday 1 May Labour Day 21 May Ascension Day 1 Jun Whit Monday 11 Jun Corpus Christi 15 Aug Assumption of the Virgin Mary 26 Oct National Day 1 Nov All Saints' Day 8 Dec Immaculate Conception 25 Dec Christmas Day 26 Dec St Stephen's Day Exceptions concerning trucks with trailers exceeding 3.5t · vehicles transporting milk; concerning vehicles with an authorised total weight of more than 7.5t · vehicles carrying meat or livestock for slaughter (but not the transport of heavy livestock on motorways); · perishable foodstuffs (but not deep frozen goods) which are as follows: fresh fruits and fresh vegetables, fresh milk and fresh dairy products, fresh meat and fresh meat products, fresh fish and fresh fish products, live fish, eggs, fresh mushrooms, fresh bakery products and fresh cakes and pastry, fresh herbs as potted plant or cut and ready-to-eat food preparations, as well as empty transports linked to the transports of the above mentioned goods or return journeys for carriage of transport facilities and wrapping of the above mentioned goods (a CMR (a consignment note) needs to be carried onboard and presented in case of inspection). -

Geographical Description of the 2Nd District of Bucharest
PRESENT ENVIRONMENT AND SUSTAINABLE DEVELOPMENT, NR. 3, 2009 GEOGRAPHICAL DESCRIPTION OF THE 2ND DISTRICT OF BUCHAREST 1 Mariana Cârstea Key words: tabular plain, loess, geomorphologic process, anthropic relief, biotic coating, artificial topographic soil. Abstract. Located in the north-east of Bucharest, with a population of approx. 400,000 inhabitants, the current territory of the 2nd district was once part of Vlăsiei forests, crossed by the river Colentina. It is a tabular plain, with low declivity on NW-SE direction the only major bumps are determined leading to the terrace Colentina, tablelands and anthropic relief. The Colentina Plain covers 36% of the Bucharest Municipality and it is characterized by altitudes that vary between 88.9 m in the Free Press Square and 55m at Cătelu. Field overlap Otopeni Bucharest north (northern district Colentina, Băneasa, Pipera) is characterized by altitudes of 85-90 m, by fragmentation of 0.5 km/square km relief, through a high frequency tablelands and growth of local slopes (common values of 10 degrees). The 2nd district is on the second place in terms of total area of green spaces (4,187,000 square meters) with an index of area of green space per capita of 13.6 square meters per head, but uneven distributed in the sector. The vegetation of 2nd district is represented in particular by vegetation in parks (Circus’ Park, Plumbuita, Morarilor, Tei), gardens and green spaces in housing blocks. Valleys are cut into loess are generally steep sides with intense phenomena of warping and biogenic mineral presents meadows, sometimes covered by lakes or swamps.