Casper Ryan Thesis.Pdf (10.61Mb)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -

The Anatomic Analysis of the Vidian Canal and the Surrounding
Braz J Otorhinolaryngol. 2019;85(2):136---143 Brazilian Journal of OTORHINOLARYNGOLOGY www.bjorl.org ORIGINAL ARTICLE The anatomic analysis of the vidian canal and the surrounding structures concerning vidian neurectomy ଝ using computed tomography scans a,∗ a b Gülay Ac¸ar , Aynur Emine C¸ic¸ekcibas¸ı , ˙Ibrahim C¸ukurova , c a d Kemal Emre Özen , Muzaffer ¸ekerS , ˙Ibrahim Güler a Necmettin Erbakan University, Meram Faculty of Medicine, Department of Anatomy, Konya, Turkey b Health Sciences University, Izmir Tepecik Trainig and Research Hospital, Department of Otolaryngology-Head and Neck Surgery, Izmir, Turkey c Katip C¸elebi University, Faculty of Medicine, Department of Anatomy, Izmir, Turkey d Selcuk University, Faculty of Medicine, Department of Radiology, Konya, Turkey Received 15 September 2017; accepted 8 November 2017 Available online 26 December 2017 KEYWORDS Abstract Intrasphenoid Introduction: The type of endoscopic approach chosen for vidian neurectomy can be specified septum; by evaluating the vidian canal and the surrounding sphenoid sinus structures. Morphometric Objective: The variations and morphometry of the vidian canal were investigated, focusing on analysis; the functional correlations between them which are crucial anatomical landmarks for preoper- Pterygoid process ative planning. pneumatization; Methods: This study was performed using paranasal multidetector computed tomography Vidian canal; images that were obtained with a section thickening of 0.625 mm of 250 adults. Vidian neurectomy Results: The distributions of 500 vidian canal variants were categorized as follows; Type 1, within the sphenoid corpus (55.6%); Type 2, partially protruding into the sphenoid sinus (34.8%); Type 3, within the sphenoid sinus (9.6%). The pneumatization of the pterygoid process is mostly seen in vidian canal Type 2 (72.4%) and Type 3 (95.8%) (p < 0.001). -

Extracranial Course of Cranial Nerves
Extracranial course of cranial nerves Oculomotor, Trochlear, Abducent, Trigeminal, Facial and Accessory nerves Dr. Heba Kalbouneh Associate Professor of Anatomy and Histology Dr. Heba Kalbouneh Brainstem Mid brain Pons Medulla Pons Inferior view Facial nerve Anatomically, the course of the facial nerve can be divided into two parts: Motor: Innervates the muscles of facial Intracranial – the course of the nerve through expression, the posterior belly of the the cranial cavity, and the cranium itself. digastric, the stylohyoid and the stapedius Extracranial – the course of the nerve outside muscles. the cranium, through the face and neck. General Sensory: A small area around the concha of the auricle, EAM Special Sensory: Provides special taste sensation to the anterior 2/3 of the tongue. Parasympathetic: Supplies many of the glands of the head and neck, including: 1- Submandibular and sublingual salivary glands (via the submandibular ganglion/ chorda tympani) 2- Nasal, palatine and pharyngeal mucous glands (via the pterygopalatine ganglion/ greater petrosal) 3- Lacrimal glands (via the pterygopalatine ganglion/ greater petrosal) Dr. Heba Kalbouneh Intracranial course The nerve arises in the pons. It begins as two roots; a large motor root, and a small sensory root The two roots travel through the internal acoustic meatus. Pons Here, they are in very close proximity to the inner ear. 7th (motor) 8th Note: The part of the facial nerve that runs between the motor root of facial and vestibulocochlear nerve is sometimes Kalbouneh known as the nervus intermedius It contains the sensory and parasympathetic Heba fibers of the facial nerve Dr. Dr. Still within the temporal bone, the roots leave the internal acoustic meatus, and enter into the facial canal. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

Trigeminal Nerve, Mandibular Division Basic Anatomy and a Bit More
The palate and the faucial isthmus He who guards his mouth and his tongue keeps himself from calamity. Proverbs 21:23 Ph.D., Dr. David Lendvai Parts of the oral cavity Parts of the oral cavity 1. Vestibule of the oral cavity Borders: - lips and cheek (bucca) - dental arches 2. Oral cavity proper Borders: - roof: hard and soft palate - floor: oral diaphragm (mylohoid m.) - antero-laterally: dental arches - posteriorly: isthmus of the fauces Etrance of the oral cavity - Philtrum - Upper & lower lip - Angulus - Rubor labii - Nasolabial groove (Facial palsy) Sobotta Szentágothai - Réthelyi Aspectus anterior 1 zygomatic process 2 frontal process 2 4 alveolar process 1 4 Faller (left) lateral aspect 1 zygomatic process 2 frontal process 3 orbital surface 4 alveolar process 2 3 Sobotta 1 4 Faller (right) Medial aspect Sobotta Superior aspect Sobotta Inferior aspect Sobotta http://www.almanahmedical.eu Sobotta Florian Dental – Dr. S. Kovách Fehér Fehér Szél Szél http://www.hc-bios.com Structures of the hard palate - incisive papilla - palatine rugae - palatine raphe - torus Hard and soft palate Muscles of the soft palate - Levator veli palatini m. - Tensor veli palatini m. - Palatoglossus m. - Palatopharyngeus m. - M. uvulae Muscles of the soft palate Muscles of the soft palate Structures of the hard and soft palate - mucous membrane - palatine glands - bone / muscles Histology of the hard palate Mucoperiosteum Histology of the soft palate NASAL SURFACE - pseudostratified ciliated columnar epithelium - lamina propria - mucous glands - striated -
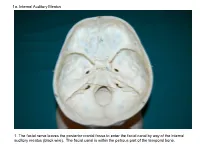
1A. Internal Auditory Meatus
1a. Internal Auditory Meatus 1. The facial nerve leaves the posterior cranial fossa to enter the facial canal by way of the internal auditory meatus (black wire). The facial canal is within the petrous part of the temporal bone. 1b. Internal Auditory Meatus The facial nerve leaves the posterior cranial fossa to enter the facial canal by way of the internal auditory meatus (black wire). 2. Hiatus of the Canal and Groove for the Greater Superficial Petrosal Nerve The greater superficial petrosal nerve leaves the facial canal to enter the middle cranial fossa by way of the hiatus of the canal for the greater superficial petrosal nerve (black wire). 3. Pterygoid Canal at Anterior Lip of the Lacerate Foramen The greater superficial petrosal nerve is joined by the deep petrosal nerve to form the nerve of the pterygoid canal (black and red wire). This nerve leaves the middle cranial fossa to enter the pterygopalatine fossa by way of the pterygoid canal. The posterior opening of the pterygoid canal is at the anterior lip of the lacerate foramen. The greater superficial nerve and the deep petrosal nerve travel within the cavernous sinus. 4. Pterygopalatine Fossa Seen Through the Pterygomaxillary Fissure The anterior opening of the pterygoid canal is into the pterygopalatine fossa (black wire). The pterygopalatine fossa is located medial to the pterygomaxillary fissure and contains the pterygopalatine ganglion. 5. External Auditory Meatus The chorda tympani nerve leaves the facial canal and crosses the middle ear (black wire). It then leaves the middle ear to arrive in the infratemporal fossa by way of the petrotympanic fissure. -

Diagrams of the Nerves of the Human Body
DIAGRAMS OF THE NERVES OF THE HUMAN BODY; EXHIBITING THEIR ORIGIN, DIVISIONS, AND CONNECTIONS, WITH THEIR DISTRIBUTION TO THE VARIOUS REGIONS OF THE CUTANEOUS SURFACE AND TO ALL THE MUSCLES. BY WILLIAM HENRY FLOWER, FELLOW OF THE ROYAL SOCIETY; FELLOW OF THE ROYAL COLLEGE OF SURGEONS. SECOND AMERICAN FROM THE SECOND ENGLISH EDITION. EDITED, WITH ADDITIONS, BY WILLIAM W. KEEN, M.D., LECTURER ON ANATOMY AND OPERATIVE SURGERY IN THE PHILADELPHIA SCHOOL OF ANATOMY; LECTURER ON PATHOLOGICAL ANATOMY IN THE JEFFERSON MEDICAL COLLEGE, FELLOW OF THE COLLEGE OF PHYSICIANS, Ac. PHILADELPHIA : TURNER HAMILTON, BOOKSELLER AND STATIONER, 106 S. TENTH STREET. 1874. Entered according to the Act of Congress, in the year 1874, by TURNER HAMILTON, in the Office of the Librarian of Congress. All rights reserved. EDITOR’S PREFACE TO THE FIRST AMERICAN EDITION. The signal benefit derived from these diagrams as illustrations in teaching, and their great convenience for ready reference in practice, have led to their republication, reduced to one-fourth the size of the originals. The Editor has made some additions where greater detail seemed desirable, has grouped the spinal nerves in their plexuses, and has added to the text a synopsis of the various sympathetic ganglia. His alterations have been very slight, and limited almost exclusively to the mechanical arrangement, e.g. in the mode of bifurcation of the brachial plexus. 1729 Chestnut Street, Philadelphia, January 1, 1874. PREFACE TO THE SECOND EDITION. These diagrams were originally published in 1860. They were designed by the author while engaged in teaching anatomy at the Medical School attached to the Middlesex Hospital. -

Tikrit University – College of Dentistry Dr.Ban I.S. Head & Neck Anatomy
Tikrit University – college of Dentistry Dr.Ban I.S. head & neck Anatomy 2nd y. Infratemporal fossa: This is a space lying beneath the base of the skull between the lateral wall of the pharynx and the ramus of the mandible. It is also referred to as the parapharyngeal or lateral pharyngeal space. Boundaries Its medial boundary is the lateral surface of the lateral pterygoid plate . The lateral wall is the ramus of the mandible and its coronoid process. The anterior wall is the posterior surface of the maxilla, at the upper margin of which is a gap between it and the greater wing of sphenoid—the inferior orbital fissure. The roof of the fossa is formed medially by the infratemporal surface of the greater wing of the sphenoid (perforated by the foramen ovale and foramen spinosum). This infratemporal surface 1 cden.tu.edu.iq Tikrit University – college of Dentistry Dr.Ban I.S. head & neck Anatomy 2nd y. of the sphenoid is bounded laterally by the infratemporal crest, where the bone takes an almost right-angled turn upwards to become part of the side of the skull, deep to the zygomatic arch and part of the temporal fossa. Thus the roof of the infratemporal fossa lateral to the infratemporal crest is not bony, but is the space deep to the zygomatic arch where the temporal and infratemporal fossae communicate. The posterior boundary is the styloid process with the carotid sheath behind it. Contents 2 cden.tu.edu.iq Tikrit University – college of Dentistry Dr.Ban I.S. head & neck Anatomy 2nd y. -

Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens After Decalcification
Hindawi Publishing Corporation International Journal of Otolaryngology Volume 2012, Article ID 418650, 7 pages doi:10.1155/2012/418650 Research Article Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens after Decalcification Longping Liu, Robin Arnold, and Marcus Robinson Discipline of Anatomy and Histology, University of Sydney, Anderson Stuart Building F13, Sydney, NSW 2006, Australia Correspondence should be addressed to Marcus Robinson, [email protected] Received 29 July 2011; Revised 10 November 2011; Accepted 12 December 2011 AcademicEditor:R.L.Doty Copyright © 2012 Longping Liu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The whole course of the chorda tympani nerve, nerve of pterygoid canal, and facial nerves and their relationships with surrounding structures are complex. After reviewing the literature, it was found that details of the whole course of these deep nerves are rarely reported and specimens displaying these nerves are rarely seen in the dissecting room, anatomical museum, or atlases. Dissections were performed on 16 decalcified human head specimens, exposing the chorda tympani and the nerve connection between the geniculate and pterygopalatine ganglia. Measurements of nerve lengths, branching distances, and ganglia size were taken. The chorda tympani is a very fine nerve (0.44 mm in diameter within the tympanic cavity) and approximately 54 mm in length. The mean length of the facial nerve from opening of internal acoustic meatus to stylomastoid foramen was 52.5 mm. -

Atlas of the Facial Nerve and Related Structures
Rhoton Yoshioka Atlas of the Facial Nerve Unique Atlas Opens Window and Related Structures Into Facial Nerve Anatomy… Atlas of the Facial Nerve and Related Structures and Related Nerve Facial of the Atlas “His meticulous methods of anatomical dissection and microsurgical techniques helped transform the primitive specialty of neurosurgery into the magnificent surgical discipline that it is today.”— Nobutaka Yoshioka American Association of Neurological Surgeons. Albert L. Rhoton, Jr. Nobutaka Yoshioka, MD, PhD and Albert L. Rhoton, Jr., MD have created an anatomical atlas of astounding precision. An unparalleled teaching tool, this atlas opens a unique window into the anatomical intricacies of complex facial nerves and related structures. An internationally renowned author, educator, brain anatomist, and neurosurgeon, Dr. Rhoton is regarded by colleagues as one of the fathers of modern microscopic neurosurgery. Dr. Yoshioka, an esteemed craniofacial reconstructive surgeon in Japan, mastered this precise dissection technique while undertaking a fellowship at Dr. Rhoton’s microanatomy lab, writing in the preface that within such precision images lies potential for surgical innovation. Special Features • Exquisite color photographs, prepared from carefully dissected latex injected cadavers, reveal anatomy layer by layer with remarkable detail and clarity • An added highlight, 3-D versions of these extraordinary images, are available online in the Thieme MediaCenter • Major sections include intracranial region and skull, upper facial and midfacial region, and lower facial and posterolateral neck region Organized by region, each layered dissection elucidates specific nerves and structures with pinpoint accuracy, providing the clinician with in-depth anatomical insights. Precise clinical explanations accompany each photograph. In tandem, the images and text provide an excellent foundation for understanding the nerves and structures impacted by neurosurgical-related pathologies as well as other conditions and injuries. -

Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens After Decalcification
Hindawi Publishing Corporation International Journal of Otolaryngology Volume 2012, Article ID 418650, 7 pages doi:10.1155/2012/418650 Research Article Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens after Decalcification Longping Liu, Robin Arnold, and Marcus Robinson Discipline of Anatomy and Histology, University of Sydney, Anderson Stuart Building F13, Sydney, NSW 2006, Australia Correspondence should be addressed to Marcus Robinson, [email protected] Received 29 July 2011; Revised 10 November 2011; Accepted 12 December 2011 AcademicEditor:R.L.Doty Copyright © 2012 Longping Liu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The whole course of the chorda tympani nerve, nerve of pterygoid canal, and facial nerves and their relationships with surrounding structures are complex. After reviewing the literature, it was found that details of the whole course of these deep nerves are rarely reported and specimens displaying these nerves are rarely seen in the dissecting room, anatomical museum, or atlases. Dissections were performed on 16 decalcified human head specimens, exposing the chorda tympani and the nerve connection between the geniculate and pterygopalatine ganglia. Measurements of nerve lengths, branching distances, and ganglia size were taken. The chorda tympani is a very fine nerve (0.44 mm in diameter within the tympanic cavity) and approximately 54 mm in length. The mean length of the facial nerve from opening of internal acoustic meatus to stylomastoid foramen was 52.5 mm. -
![NASAL CAVITY and PARANASAL SINUSES, PTERYGOPALATINE FOSSA, and ORAL CAVITY (Grant's Dissector [16Th Ed.] Pp](https://docslib.b-cdn.net/cover/6054/nasal-cavity-and-paranasal-sinuses-pterygopalatine-fossa-and-oral-cavity-grants-dissector-16th-ed-pp-1806054.webp)
NASAL CAVITY and PARANASAL SINUSES, PTERYGOPALATINE FOSSA, and ORAL CAVITY (Grant's Dissector [16Th Ed.] Pp
NASAL CAVITY AND PARANASAL SINUSES, PTERYGOPALATINE FOSSA, AND ORAL CAVITY (Grant's Dissector [16th Ed.] pp. 290-294, 300-303) TODAY’S GOALS (Nasal Cavity and Paranasal Sinuses): 1. Identify the boundaries of the nasal cavity 2. Identify the 3 principal structural components of the nasal septum 3. Identify the conchae, meatuses, and openings of the paranasal sinuses and nasolacrimal duct 4. Identify the openings of the auditory tube and sphenopalatine foramen and the nerve and blood supply to the nasal cavity, palatine tonsil, and soft palate 5. Identify the pterygopalatine fossa, the location of the pterygopalatine ganglion, and understand the distribution of terminal branches of the maxillary artery and nerve to their target areas DISSECTION NOTES: General comments: The nasal cavity is divided into right and left cavities by the nasal septum. The nostril or naris is the entrance to each nasal cavity and each nasal cavity communicates posteriorly with the nasopharynx through a choana or posterior nasal aperture. The roof of the nasal cavity is narrow and is represented by the nasal bone, cribriform plate of the ethmoid, and a portion of the sphenoid. The floor is the hard palate (consisting of the palatine processes of the maxilla and the horizontal portion of the palatine bone). The medial wall is represented by the nasal septum (Dissector p. 292, Fig. 7.69) and the lateral wall consists of the maxilla, lacrimal bone, portions of the ethmoid bone, the inferior nasal concha, and the perpendicular plate of the palatine bone (Dissector p. 291, Fig. 7.67). The conchae, or turbinates, are recognized as “scroll-like” extensions from the lateral wall and increase the surface area over which air travels through the nasal cavity (Dissector p.